Mesenteric panniculitis
advertisement

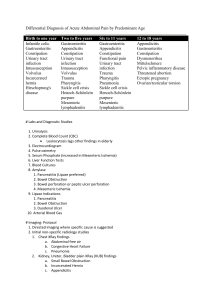
Mesenteric panniculitis BEN ROMDHANE MH Hopital AVICENNE BOBIGNY Mesenteric panniculitis • inflammatory disorder of the fatty tissue of the bowel mesentery • Uncommon • several names( resulting in considerable confusion ): lipodystrophy, mesenteric Weber-Christian disease, fibrosing mesenteritis, sclerosing mesenteritis retractile mesenteritis • varied terminology reflects the pathological spectrum • now considered to be one single disease • chronic nonspecific inflammatory process in the mesentery • rarely may lead to fibrosis and retraction • If inflammation predominates over fibrosis the process is known as mesenteric panniculitis • when fibrosis and retraction predominate, terms: fibrosing mesenteritis, retractile mesenteritis or sclerosing mesenteritis are more commonly used • MP supposed to be very rare, approximately 250 cases reported in the literature • With increased use of abdominal diagnostic imaging, MP is diagnosed more often • Recently reported prevalence of 0.6% of all patients undergoing an abdominal CT for various indications Pathogenesis • infiltration of mesenteric fat by : inflammatory cells, mainly lymphocytes and fat-laden macrophages • with inflammation, a mixture of fat necrosis and fibrosis may be present in the mesentery • exact cause remains unclear • MP occurs independently or in association with other disorders • A variety of possible causative factors have been proposed: autoimmune disorders ischemia prior abdominal surgery • also suggested paraneoplastic response • This possible association with a concomitant malignancy highlighted in a study by Daskalogiannaki • reporting the presence of a coexisting abdominal or distal malignancy in 69% of patients with CT features of MP • In other studies prevalence of malignancy not different from general population of patients undergoing CT for all various indications Clinical characteristics • mostly middle or late adulthood, • male predominance. • Clinical manifestations may be related to the inflammation or to mass-effect • Presenting symptoms may vary • may also be entirely asymptomatic • commonly include non-specific abdominal pain • Palpable abdominal mass may be present may lead to the clinical misdiagnosis (aortic aneurysm ...) • Laboratory findings: often within the normal range or demonstrate non-specific findings: mild leucocytosis and elevation of the erythocyte sedimentation rate. • before the advent of modern diagnostic imaging, MP was diagnosed exclusively as an unexpected finding at exploratory laparotomy or autopsy Diagnosis • A definite diagnosis of MP can be made only by pathologic analysis • However, the incidental benign and often asymptomatic nature of MP usually does not justify biopsy • In these cases, diagnosis may be suggested by characteristic imaging features from the radiological literature from pathologically proven cases US features • often quite subtle may be easily overlooked • poorly defined hyperechoic change of the mesenteric fat • decrease in mesenteric compressibility • may be seen in various conditions with mesenteric involvement( lipomatous tumors... • CT always recommended to analyze any USfound mesenteric abnormalities A. C. van Breda Vriesman Eur Radiol (2004) CT features • increased density of mesenteric fatty tissue (approximately− 40 to −60 HU) compared to the attenuation values of normal retroperitoneal or subcutaneous fat (−100 to −160 HU) • hyperattenuating fat surrounds mesenteric vessels • but does not displace them • some regional mass-effect by displacing locally small bowel loops • mass most frequently located at the left side corresponding to jejunal mesentery Piessen G Annales de chirurgie 131 2006 • Other CT features reported • may be valuable clues for the diagnosis: the fat-ring sign, tumoral pseudocapsule soft-tissue nodules Fat-ring sign • Fat-ring sign or “fatty halo 75–85% • low-density fat surrounding vessels and nodules • preservation of normal fat density, corresponding to unaffected noninflamed fat interposed between vessels or nodules and inflammatory cells at histopathology • non-specific • also reported incidentally in non-Hodgkin’s lymphoma in which chemotherapy treatment has led to reduction of the mesenteric lymphadenopathy, leaving a fine haziness throughout the mesenteric fat Tumoral pseudocapsule • peripheral band with soft-tissue attenuation limiting the inflammatory mesenteric mass • thickness of this dense stripe usually does not exceed 3 mm • reported in 50–59% of patients • lipomatous tumor (lipoma or liposarcoma) may be well-defined by a similar dense rim • but these lesions will often show some mass-effect on the mesenteric vessels in contrast to M P A. C. van Breda Vriesman Eur Radiol (2004) Soft-tissue nodules • small soft-tissue nodules scattered within the hyperattenuating mesenteric mass • in 80% of cases • Correspond probably to lymph nodes • usually less than 5 mm in diameter • Mesenteric lymph nodes larger than 10 mm atypical for MP • biopsy or fine-needle aspiration must be considered to exclude malignancy SM • most commonly appears as a soft-tissue mass in the small bowel mesentery • The mass may envelop the mesenteric vessels, and collateral vessels • Mesenteric thickening and fibrosis often with nodular masses involving the appendices epiploicae of the colon • Calcification may be present, usually in the central necrotic portion of the mass • it may be related to the fat necrosis • Cystic components also described • may be the result of lymphatic or venous obstruction and necrotic change • Enlarged mesenteric or retroperitoneal lymph nodes may be present Farzana Nawaz Ali, Case Reports in Medicine2010 Farzana Nawaz Ali, Case Reports in Medicine 2010 Imaging-based differential diagnosis • misty mesentery :Alteration in the density of the mesenteric fat on CT • with an extensive differential diagnosis • MP reserved for idiopathic inflammation leading to a misty mesentery • imaging diagnosis can therefore be made only after exclusion of any of the following alternative causes of a misty mesentery Mesenteric edema • Many causes • heart failure, portal hypertension, mesenteric vascular thrombosis and lymphedema. • mesenteric edema secondary to a systemic disease, usually associated with generalized subcutaneous edema and ascites. • Ascites is not a feature of MP and indicates an alternative diagnosis Inflammation • acute pancreatitis is the typical inflammatory process associated with increased CT density of the mesenteric fat • usually centered in the peripancreatic region • With usually increased levels of amylase in serum and urine enabling the diagnosis • Focal inflammations such as appendicitis and colonic diverticulitis may also cause local hyperattenuation of adjacent mesenteric fat • these diagnoses must be carefully ruled out Mesenteric Hemorrhage • hemorrhage, caused by blood dissecting from mesenteric vessels or from the bowel wall • may be traumatic or spontaneous • A history of trauma, use of anticoagulantia • or high-density peritoneal fluid suggests the correct diagnosis Neoplasm • Non-Hodgkin’s lymphoma most common mesentery tumor • Typically bulky lymphadenopathy, • often also n the retroperitoneum, indicating the correct diagnosis • Shrinkage of mesenteric lymphadenopathy after chemotherapy may result in residual scarring that may mimic MP • Needs reviewing the patient’s prior CT scans • lymphoma manifested as nodal mass in the root of the mesentery may mimic SM • no calcification unless previously treated • Both can encase mesenteric vasculature • lymphoma almost never result in ischemia • fat halo sign favors a diagnosis of SM • large, nodes favor lymphoma • Treated lymphoma may also produce a misty mesentery simulating the MP • Primary mesenteric neoplasms (desmoid, mesenteric cyst, lipomatous tumors) cause mass-effect on mesenteric vessels • Other tumors :mesothelioma, or metastatic tumors:( pancreatic, colon or ovarian carcinoma ) may affect the mesentery by soft-tissue tumor deposits, or may cause mesenteric edema by lymphatic obstruction • correct diagnosis made by identification of the primary tumor or detection of extramesenteric peritoneal nodules, or by cytological analysis of ascites A. C. van Breda Vriesman Eur Radiol (2004) • Carcinoid tumor may simulate SM • ill-defined, infiltrating soft-tissue mass in the root of the mesentery with calcification and desmoplastic reaction • fat ring sign favors a diagnosis of SM • enhancing mass in bowel wall or hypervascular liver metastases : sign diagnosis of carcinoid tumor • primary mesenteric mesothelioma can produce mesenteric soft-tissue implants in mesentery, also seen in the omentum and along the bowel surfaces. • Ascites not associated with SM • Calcification not common Treatment • Treatment usually empirical • may consist of steroids, colchicine, immunosuppressive agents, or orally administered progesterone • In SM Surgical resection difficult due to vessel compromise may be of no clear benefit • colostomy may be necessary with colonic involvement by SM • Variable course With treatment: relatively benign course progression of the disease eventually leads to death In some cases, complete resorption • CT suggest the diagnosis of SM • CT useful in distinguishing SM from other mesenteric diseases such as lymphoma or carcinoid tumor • Biopsy necessary for SM diagnosis • CT optimal study for the follow up