Preview of ATP-IV
advertisement

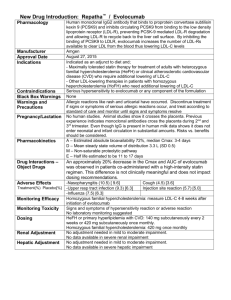
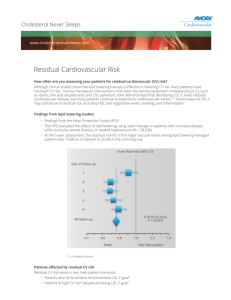
Lipid Management Standard and Advanced Preview of ATP-IV Thomas G. Allison, PhD, MPH Mayo Clinic Rochester, MN USA DISCLOSURE Relevant Financial Relationship(s) None Off Label Usage None Treatment Categories, LDL-C Goals and Cut-points: ATP-III Risk Category CHD or CHD risk equivalent 2 Risk Factors 10-yr risk 10–20% 10-yr risk <10% <2 Risk Factors LDL-C Goal Consider Drug Therapy <100 mg/dL 130 mg/dL* <130 mg/dL <130 mg/dL 130 mg/dL 160 mg/dL <160 mg/dL 190 mg/dL * 100–129 mg/dL = after TLC, consider statin, niacin, or fibrate therapy Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001;285:2486-2497. Major ATP III Risk Factors • Age Male ≥ 45 years Female ≥ 55 years • Family History Male first degree relative < 55 years Female first degree relative < 65 years • HDL-C < 40 mg/dL • Hypertension • Current Smoking CAD Equivalents • • • • • • • Coronary Artery Disease (CAD) Diabetes Mellitus Abdominal Aortic Aneurysm Carotid Artery Disease (>50% stenosis) Prior CVA or TIA Peripheral Arterial Disease Framingham Score >20% 10 yr Risk CAD Risk Equivalents? • Chronic Renal Insufficiency • Abnormal Coronary Calcium Scores – Agatston score > 400 Goals for Therapy: 2004 Addendum • NCEP ATP III guidelines for LDL Therapy LDL-C <160 for 1 or less risk factors LDL-C <130 for 2+ risk factors < 100 is a therapeutic option LDL-C <100 for CAD and CAD equivalents <70 is option for very high risk patients 1. 2. 3. 4. 5. CAD + multiple risk factors, especially diabetes CAD + severe or poorly controlled risk factor(s) CAD + metabolic syndrome Acute coronary syndrome CAD event despite baseline LDL-C < 100 LDL-C Therapy • • • • • • Lifestyle Change Statins Bile Acid Sequestrants Ezetimibe Niacin Plant Stanols, Sterols, Phytosterols Residual Risk: Non-HDL-C • ATP III: Non-HDL-C is a secondary target of drug therapy when TG ≥ 200mg/dL • Represents all the triglyceride-rich lipoproteins – considered atherogenic • Non-HDL-C = Total Cholesterol – HDL-C • Valid even if patient is non-fasting • Cost-Effective Targets for Therapy after LDL-C Goal in Patients with TG 200 mg/dL LDL-C target (mg/dL) Non-HDL-C target (mg/dL) CHD or CHD risk equivalent <100 <130 No CHD, 2+ RF <130 <160 No CHD, <2 RF <160 <190 Patient Category Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001;285:2486-2497. Potential Goal Modifying Factors • Lp(a) • High sensitivity CRP • Metabolic Syndrome Definition of the Metabolic Syndrome Defined by presence of >3 risk factors Risk Factor Defining Level Waist circumference (abdominal obesity) >40 in (>102 cm) in men >35 in (>88 cm) in women Triglyceride level >150 mg/dl HDL-C level <40 mg/dl in men <50 mg/dl in women Blood pressure >130/>85 mmHg Fasting glucose >100 mg/dl Grundy, et al. Diagnosis and management of the metabolic syndrome: an AHA/NHLBI Scientific Statement. Circulation 2005;112:2735-2752. Dr. Allison Attempts to Call Forth the Contents of ATP-IV Will ATP-IV Signal a New Wave of Lipid Management? Sweeping Changes? Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel IV) Expert Panel Membership Co-Chairs Alice H. Lichtenstein, D.Sc. Tufts University Boston, Massachusetts Neil Stone, M.D. Northwestern University School of Medicine Chicago, Illinois C. Noel Bairey Merz, M.D. University of California, Los Angeles Daniel Rader, M.D. University of Pennsylvania Conrad Blum, M.D. Columbia University Jennifer Robinson, M.D, M.P.H. University of Iowa Robert H. Eckel, M.D. University of Colorado, Denver Frank M. Sacks, M.D. Harvard University School of Public Health Anne Carol Goldberg, M.D., FACP, FAHA Washington University J. Sanford Schwartz, M.D. University of Pennsylvania Ronald M. Krauss, M.D. Children's Hospital Oakland Research Institute Sidney C. Smith, Jr. M.D. University of North Carolina Donald M. Lloyd-Jones, M.D., Sc.M. Northwestern University Karol Watson, M.D., Ph.D. University of California at Los Angeles Patrick McBride, M.D., M.P.H. University of Wisconsin Peter W. F. Wilson, M.D. Emory University School of Medicine Status Expected Availability for Public Review and Comment: Spring 2011 Expected Release Date: Fall 2011 Issues for ATP-IV 1. Should the goals for LDL-C in primary prevention be lowered? 2. What to do with CRP – routine use in risk stratification, secondary target? 3. What about secondary target? – Non-HDL-C, HDL-C, apo B, LDL Particle concentration? 4. Move from 10-year to lifetime risk? Jupiter Trial • To test the hypothesis that statin treatment will reduce CV events in patients without baseline CVD with “normal” LDL-C (< 130 mg/dL) and elevated hsCRP (≥ 2.0 mg/L) Ridker PM et al. NEJM 2008;359:2195-2207 • The most innovative and potentially important lipid-lowering trial since the 2004 ATP-II Addendum Jupiter Methods • 17,802 subjects (38% women) – Men ≥ 50 years; women ≥ 60 years – Triglycerides < 500 mg/dL • Randomized to Rosuvastatin 20 mg/day or placebo • Planned 60 month follow-up • Primary outcome was major CV event – Including elective revascularization Jupiter Results • Study terminated early on 3-30-08 with median follow-up of 1.9 years • Compliance at study termination was 75% • 44% reduction in primary endpoint – 0.77% versus 1.36% per year • 20% reduction in total mortality – 1.00% versus 1.25% per year 12-Month Laboratory Results (Medians) Rosuvastatin Placebo hs-CRP 2.2 3.5 LDL-C 55 110 HDL-C 52 50 TG 99 119 JUPITER Questions • Would a lower-cost, generic statin show similar benefit? • Is measurement of hsCRP necessary for risk stratification in primary prevention – Ridker conflict of interest issues • Was the benefit due to LDL-C lowering or hsCRP lowering? Risk Factors in Jupiter Subjects • • • • • • Average age = 66 years Current smokers = 16% Metabolic syndrome = 41% Family history of premature CAD = 11% 25% had fasting glucose > 102 mg/dL 25% had systolic BP > 145 mmHg PROVE IT - TIMI 22: Study Design 4,162 patients with an Acute Coronary Syndrome < 10 days ASA + Standard Medical Therapy Double-blind “Standard Therapy” Pravastatin 40 mg “Intensive Therapy” Atorvastatin 80 mg 2x2 Factorial: Gatifloxacin vs. placebo Duration: Mean 2 year follow-up (>925 events) Primary Endpoint: Death, MI, Documented UA requiring hospitalization, revascularization (> 30 days after randomization), or Stroke Changes from (Post-ACS) Baseline in Median LDL-C LDL-C (mg/dL) 120 Median LDL-C (Q1, Q3) 100 95 (79, 113) Pravastatin 40mg 80 21% 62 (50, 79) 60 49% Atorvastatin 80mg 40 P<0.001 20 <24h Rand. 30 Days 4 Mos. 8 Mos. 16 Mos. Final Note: Changes in LDL-C may differ from prior trials: • 25% of patients on statins prior to ACS event • ACS response lowers LDL-C from true baseline PROVE IT: Concomitant Therapies PCI for initial ACS pre-random. 69% Aspirin 93% Warfarin 8% Clopidogrel (initial) (at F/U) 72% 20% B-blockers 85% ACE 69% ARB 14% All-Cause Death or Major CV Events in All Randomized Subjects 30 Pravastatin 40mg (26.3%) 25 20 % with 15 Event Atorvastatin 80mg (22.4%) 16% relative risk reduction (p = 0.005) 10 5 But absolute residual risk is 22% 0 0 3 6 9 12 15 18 21 Months of Follow-up 24 27 30 Sources of Residual Risk • Not providing appropriate medical therapy? • Inadequate control of non-lipid risk factors? • Not addressing emerging risk factors? – CRP, Lp(a) • Inadequate control of lipids using LDL target only? – – – – – Non-HDL HDL or apo A-1 Apo B LDL particle number LDL particle size Secondary Lipid Target • In ATP-III, non-HDL-C was identified as the secondary lipid target – Sum of cholesterol in all atherogenic lipoproteins • LDL-C, Lp(a)-C, VLDL-C, IDL-C • No major trial since publication of ATP-III in 2001 that specifically treated non-HDL-C Lowering non-HDL-C • • • • • Increase the statin dose Add fibrate Add niacin High dose fish oil Exercise, CHO restriction, weight loss FIELD Study Fenofibrate to Prevent Cardiovascular Events in Diabetics FIELD Study Investigators Lancet 2005; 366:1849-1861 FIELD Mortality No significant benefit shown in ACCORD-Lipids for fenofibrate added to Simvastatin 40 mg/day. NEJM 2010, March 14. LDL Particles Cause Atherosclerosis Low Density Lipoprotein particles (LDL) are the causal agents in atherosclerosis.1 The more LDL particles a person has, the higher the risk for plaque buildup that causes heart attacks, regardless of how much cholesterol those particles carry. 1 Fredrickson et al. NEJM 1967; 276: 148 LDL-C is not LDL Apo B POLAR SURFACE COAT Phospholipid Free cholesterol This is LDL NONPOLAR LIPID CORE Cholesterol Ester Triglyceride This is LDL Cholesterol James Otvos 2007 lipoproteins EDTA sugars LDL Particle Number Distribution in MESA LDL-C <100 mg/dL (n=1,425) 5th 25 10% (n=141) 20th 42% (n=603) 50th 80th percentile 36% (n=509) 10% (n=150) 2% (n=22) 20 Percent of Subjects 15 10 5 0 700 1000 1300 1600 (nmol/L) LDL Size (nm) 21.3 (0.7) 20.5 (0.6) 20.1 (0.5) HDL-C (mg/dL) 58 (18) 47 (15) 41 (11) Triglycerides (mg/dL) 98 (60) 136 (71) 199 (75) AHA/ADA “Metabolic Syndrome/Metabolic Risks” meeting. San Francisco, May 3-5, 2006 LDL Particle Number Distribution in MESA LDL-C = 100-118 mg/dL 5th 25 1% (n=10) 20th 24% (n=215) 50th 54% (n=484) 80th 19% (n=168) percentile 3% (n=26) 20 Percent of Subjects 15 22% 10 MetSyn (-) (n=903) 5 0 700 25 20 0% (n=0) 1000 4% (n=20) 1300 33% (n=153) 1600 (nmol/L) 46% (n=210) 15 Percent of Subjects 17% (n=76) 63% MetSyn (+) (n=459) 10 5 0 700 1000 1300 AHA/ADA “Metabolic Syndrome/Metabolic Risks” meeting. San Francisco, May 3-5, 2006 1600 (nmol/L) Probability of Event-free Survival CHD Event Associations of NMR LDL Particle Number (LDL-P) versus LDL Cholesterol (LDL-C) Low LDL-C – Low LDL-P (n=1249) High LDL-C – Low LDL-P (n=284) High LDL-C – High LDL-P (n=1251) Low LDL-C – High LDL-P (n=282) Years of Follow-up Cromwell WC et al: J Clinical Lipidology 2007;1:583-592 Brief Comments Apo B or Non-HDL versus LDL-P • Apo B and non-HDL are likely better predictors of risk than LDL-C in patients with cardiometabolic syndrome • Non-HDL costs nothing extra to measure • Apo B measurement does not require unique, expensive technology • Apo B gives equal weight to each particle: LDL, Lp(a), VLDL, IDL – Not equal atherogenicity – Treatment strategies different for each particle • Non-HDL similarly lumps particle types together Example 1 – TC=200, HDL=50, TG=200, non-HDL=150 Example 2 – TC=170, HDL=20, TG=500, non-HDL=150 • Is risk equivalent for these 2 patients? Prediction of Lifetime Risk for Cardiovascular Disease by Risk Factor Burden at 50 Years of Age Donald M. Lloyd-Jones et al Circulation 2006;113:791-798 Generic Prevention Drugs Drug Monthly Cost Statin $4.00 Beta blocker $4.00 Metformin $4.00 ACE-inhibitor ± HCTZ $4.00 Amlodipine $4.00 All national discount pharmacy chains – Lower price ($10) for 3 months supply Can potentially reduce cost further with a pill cutter Living Under the Umbrella of Good Cardiovascular Health LDL-C FBG SBP <100 <100 <120 Predictions for ATP-IV 1. The goals for LDL-C in primary prevention will be lowered. 2. There will be a stronger statement on hsCRP, but routine use in risk stratification or use as secondary target will not be specifically endorsed. 3. Non-HDL-C will remain the secondary lipid target, but optional use of apo B or LDL-P will be endorsed. 4. A new risk calculator providing lifetime risk estimates will be provided. • Comments? • Questions?