File
advertisement

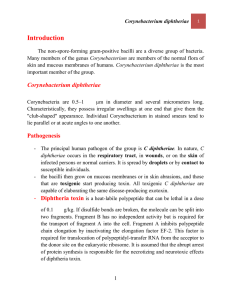
Diphtheria • Is an acute infectious disease of the childhood characterized by local inflammation of the epithelial surface , formation of a membrane , and severe toxemia Epidemiology : • Age groups : Pre – school age children • Occurs in the autumn and winter months. Caused by ---- Gram positive bacilli, Corynebacterium diphtheria Cont .. Source : - secretions and discharge from an infected person or carrier – Human are chief reservoirs Mode of transmission : – Contact or through droplets of secretion Portal of entry : – Respiratory tract – May enter through the conjuntiva or skin wound Risk factors 1. Poor nutrition. 2. Outbreak in the community. 3. Crowded or unsanitary living conditions. 4. Low vaccine coverage among infants and children. 5. Lack of mass immunization programmes amongst children and adults at high risk. 6. Insufficient information for the general public on dangers of the disease and the benefits of immunization. 7. Lack of vaccines in many areas. Pathogenesis • Entry ------ the bacilli multiply locally in the throat and elaborate a powerful exotoxin ----- produce local and systemic symptoms. Local lesions : • Exotoxin causes necrosis of the epithelial cells and liberates serous and fibrinous material which forms a grayish white pseudomembrane • The membrane bleeds on being dislodged • Surrounding tissue is inflamed and edematous Cont … Systemic lesions : • Exotoxin affects the heart , kidney and CNS Heart : – Myocardial fibers are degenerated and the heart is dilated – Conduction disturbance CNS : polyneuritis Kidney : renal tubular necrosis Clinical features • Incubation period : 2 – 5 days Constitutional symptoms: • Onset : acute with fever ( 39 C ) , malaise , headache and loss of appetite • Child looks very sick and toxic • Delirium • Circulatory collapse ( myocarditis ) Local manifestation Depend on the site of lesion: Nasal diphtheria : • Unilateral or bilateral serosanguineous ( blood and serous fluid ) discharge from the nose • Excoriation of upper lip • Toxemia is minimal Faucial diphtheria : • Redness and swelling over fauces • Exudates on the tonsils coalesces to form grayish white pseudo membrane • Regional lymph nodes are inflamed • Sore throat and • dysphagia Fauces ( throat ) Fauces : - two pillars of mucous membrane. Anterior : known as the palatoglossal arch and Posterior : the palatopharyngeal arch Between these two arches is the palatine tonsil. Cont … Laryngotracheal diphtheria : – Membrane over the larynx results in brassy ( hardness ) cough and hoarse voice – Respiration ------- noisy – Suprasternal and subcostal recession – Restlessness – Increasing respiratory effort – Use of accessory muscles Unusual sites : • Conjunctiva and skin In the skin : • Ulcers ( tender ) Diagnosis • clinical history , examination and identification of diphtheria bacilli from the site of lesion. • Culture • Albert`s staining • Fluorescent antibody technique Schick Test –Schick test: It is an intradermal test, the test is carried out by injecting intradermally into the skin of forearm 0.2 ml of diphtheria toxin, while into the opposite arm is injected as a control, the same amount of toxin which has been inactivated by heat. Interpretation • Negative reaction: If a person had immunity to diphtheria, no reaction will be observed on either arm. • Positive reaction: An area of in duration 10-15 mm in diameter generally appears within 24-36 hours reaching its maximum development by 4-7 days, the control arm shows no change. The person is susceptible to diphtheria. • False positive reaction: A red flush develops in both arms, the reaction fades very quickly, and disappears by 4th day. This is an allergic type of reaction found in certain individuals • Combined reaction: the control arm shows pseudo positive reaction and the test arm is true +ve reaction, susceptible and need vaccination Differential diagnosis Nasal diphtheria : • Foreign body in nose , • Rhinorrhea • • • • • Laryngeal diphtheria : Croup Acute epiglottitis Laryngotracheobronchitis Peritonsillar abscess Retropharyngeal abscess Cont …. Faucial diphtheria : Acute streptococcal membranous tonsillitis ( high grade fever , child less toxic ) Viral membranous tonsillitis : • high grade fever , • WBC : normal or low , • Antibiotic : no effects Herpetic tonsillitis ( Gingivitis and stomatitis ) Infectious mononeucleosis : • Generalised rash and lymphadenopathy besides oral mucosal lesions Treatment Principles : • Neutralization of free circulating toxin by administration of antitoxin • Antibiotic to eradicate bacteria • Supportive and symptomatic therapy • Management of complication Antitoxin • • • • Diphtheria antitoxin : Pharyngeal or laryngeal diphtheria of 48 hours duration : 20,000 to 40,000 units. Nasopharyngeal lesions : 40,000 – 60,000 units Extensive disease of 3 or more days duration or patient with swelling of neck : 80,000 – 120,000 units Antitoxin may be repeated if the clinical improvementis slower Antibiotics Penicillin : • Procaine penicilline ( 3 – 6 lac units IM at 12 hourly intervals till the patient is able to swallow ) • Oral penicillin ( 125 – 250 mg qid ) • Erythromycin ( 25 – 30 mg / kg / day ) for 14 days • Three negative cultures at 24 hours intervals should be obtained before the patient is declared free of the organism Supportive and symptomatic therapy • Bed rest for 2 – 3 weeks ( to reduce cardiac complications ) • Antipyretics and sedative ( if required ) • Monitor rate and rhythm of the heart Management of complication Respiratory obstruction : • Humidified oxygen • Tracheostomy Myocarditis : • Fluids and salt restriction • Sedation and oxygen supply • Diuretics and digoxin Neurological complications : • Palatal paralysis ( NG feeding ) • Generalised weakness ( as polio ) Complications Myocarditis : • Occurs towards the end of the first or beginning of second week • Abdominal pain , vomiting , dyspnea , tachycardia Neurological complications : ( Traid ) – Palatal paralysis ( 2 weeks ) – General polyneuritis ( 3 – 6 weeks ) – Loss of accommodation ( 3 weeks ) Renal complications : • Oliguria and proteinuria indicate kidney complications Prevention Vaccination: Immunisation with diphtheria toxoid, combined with tetanus and pertussis toxoid (DTP vaccine), should be given to all children at two, three and four months of age. Booster doses are given between the ages of 3 and 5 . The child is given a further booster vaccine before leaving school and is then considered to be protected for a further 10 years (16 – 18 years). Prognosis • Death may occur due to : – Respiratory obstruction – Myocarditis – Respiratory paralysis