PowerPoint 演示文稿

LIU Chuan Yong
刘传勇
Institute of Physiology
Medical School of SDU
Tel 88381175 (lab)
88382098 (office)
Email: liucy@sdu.edu.cn
Website: www.physiology.sdu.edu.cn
Section 4
Regulation of the Circulation
Introduction
The aim of the circulatory regulation is to regulate the blood flow of organs to fit their metabolic requirement in different condition.
The regulation of blood flow are of three major types:
Neural
Humoral
Local
Neural control of blood flow
affects blood flow in large segments of the systemic circulation,
shifting blood flow from the nonmuscular vascular bed to the muscles during exercise
changing the blood flow in the skin to control body temperature.
Humoral control
hormones, ions, or other chemicals in blood
cause either local increase or decrease in tissue flow
or widespread generalized changes in flow.
Local control of blood flow
in each individual tissue,
the flow being controlled mainly in proportion to that tissue’s need for blood perfusion
I. Neural Regulation of the
Circulation
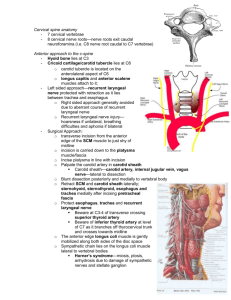
1. Innervation of the Circulatory
System
Cardiac innervation
Innervation of blood vessels
Sympathetic vasoconstrictor fiber
Sympathetic vasodilator fiber
Parasympathetic nerve fiber to peripheral vessels
Cardiac innervation
Sympathetic nerve – noradrenergic fiber;
Parasympathetic nerve- cholinergic fiber
Noradrenergic sympathetic nerve
to the heart increase the cardiac rate (chronotropic effect)
the force of cardiac contraction (inotropic effect).
C holinergic vagal cardiac fibers decrease the heart rate.
Cardiac innervation (contin.)
moderate amount of tonic discharge in the cardiac sympathetic nerves at rest
a good deal of tonic vagal discharge
( vagal tone ) in humans
When the vagi are cut in experiment animals, the heart rate rises
Innervation of blood vessels
Sympathetic vasoconstrictor fiber
Distribution: Almost all segments of the circulation.
The innervation is powerful in the kidneys, gut, spleen and skin,
is less potent in both skeletal and cardiac muscle and in the brain.
Innervation of blood vessels
Sympathetic vasoconstrictor fiber
(contin.)
Almost all vessels, such as arteries, arterioles, venules and veins are innervated,
except the capillaries, precapillary sphincters and most of the metarterioles.
Tone: Usually the sympathetic vasoconstrictor fibers keep tonic.
Innervation of blood vessels
2) Sympathetic vasodilator fiber
The sympathetic nerves to skeletal muscles carry sympathetic vasodilator fibers as well as constrictor fibers.
In animals, such as the cat, dog, these sympathetic vasodilator fibers release acetylcholine at their endings and cause vasodilation.
Importance: increase the blood flow in skeletal muscle during exercise and stress.
Innervation of blood vessels
3) Parasympathetic nerve fiber to peripheral vessels
Parasympathetic nerve fibers innervate vessels of the blood vessels in
Meninges ( 脑膜 , 髓膜 )
the salivary glands,
the liver
the viscera in pelvis
the external genitals.
Importance: Regulate the blood flow of these organs in some special situations .
2 Cardiovascular Center
The control center of cardiovascular activities is the nucleus groups at different levels for controlling cardiovascular activities,
including
spinal cord,
brain stem,
hypothalamus,
limbic system,
cerebral cortex
cerebellum.
Cardiovascular Center
if the brain of an anesthetized animal is sectioned at the level of the lower pons, the blood pressure falls.
If the section is made at the level of the obex, the fall in blood pressure is more profound .
Cardiovascular centers of the brainstem
Medulla oblongata is essential to
Cardiovascula r centers .
Cardiovascular centers of the brainstem
vasoconstrictor-area
vasodilator area
cardioinhibitory area
relay station of afferent nerve
1 . rostral ventrolateral medulla, rVLM
(Vasoconstrictor area) :
2. Caudal ventrolateral medulla, cVLM
( Vasodilator area )
3 . NTS ( nucleu of solitary tract relay station of afferent nerve)
4 . Cardioinhibitory area
1). vasoconstrictor-area (rVLM)
(neurotransmitter: NE neurons )
(l) the cardiac sympathetic center
(2) the sympathetic vasoconstrictor center
2).
vasodilator area (cVLM)
(NE neurons) to inhibit action of Cl area
→ vasodilation
3).cardioinhibitory area
( dorsal vagal nucleus and nucleus ambigulus ) the cardial vagus center
4).relay station of afferent nerve
NTS (nucleu of solitary tract) to accept and integrate afferent impulses and then affect other centers
3. Reflex Regulation of the
Circulation
Baroreceptor reflexes
Reflex involving arterial chemoreceptors
CNS ischemic response
(1) Baroreceptor reflexes
1) Physiological anatomy of the baroreceptors.
Carotid sinus
At the bifurcation of the common carotid arteries
the root of internal carotid artery shows a little bulge
has stretch receptors in the adventitia
are sensitive to arterial pressure fluctuations
Carotid sinus.
(contin.)
Afferent nerves from these stretch receptors travel in the carotid sinus nerve
which is a branch of the glossopharyngeal nerve. (IXth cranial nerve)
Aortic arch.
baroreceptors are also present in the adventitia of the arch of aorta
have functional characteristics similar to the carotid sinus receptors.
their afferent nerve fibers travel in the aortic nerve,
which is a branch of the vagus nerve. (Xth cranial nerve)
2) buffer nerves activity
The carotid sinus nerves and vagal fibers from the aortic arch are commonly called the buffer nerves
At normal blood pressure levels, the fibers of the buffer nerve discharge at a low rate.
When the pressure in the sinus and aortic arch rises, the discharge rate increases;
when the pressure falls, the rate declines.
Sinus Nerve response to Blood Pressure
The carotid sinus baroreceptors are not stimulated by intrasinus pressure between 0 – 60 mmHg (aortic baroreceptors,
0-30mmHg).
Between 60 to 80 mmHg, the carotid sinus baroreceptors respond progressively more and more strongly.
The response is the greatest at pressure level near the normal mean arterial pressure (100 mmHg).
At sinus pressure above 180 mmHg, there is no further increase in response .
3) Relationship between the isolated carotid sinus pressure and the blood pressure
Raising the carotid sinus pressure leads to a fall in arterial blood pressure.
Lowering the carotid sinus pressure leads to a rise in arterial blood pressure
CSP, carotid sinus pressure; FABP, femoral artery blood pressure
Set point : The point where the carotic sinus
(isolated) pressure and blood pressure are the same.
4) Concept and mechanism of baroreceptor reflex
Any drop in systemic arterial pressure decreases the discharge in the buffer nerves,
and there is a compensatory rise in blood pressure and cardiac output.
Any rise in blood pressure produce dilation of the arterioles and decreases cardiac output until the blood pressure returns to its previous normal level.
Arterial
Pressure
Baroreceptor
Vasoconstrictor Center
Cardio-acceleratory Area
Cardio-inhibitory Area +
Carotid Sinus
Aortic Arch
Sinus Nerve
Vagus Nerve
Peripheral Vascular Dilation
Heart Rate Contractility
Peripheral Resistance ( R)
Cardiac Output (Q)
Arterial pressure decrease back towards normal
(5) Importance of the baroreceptor reflex
To keep the arterial pressure relatively constant
Through short term regulation of blood pressure in the rang of 70 mmHg to 150 mmHg, maintain the mean blood pressure at about 100 mmHg
Tonic regulation of blood pressure
Pressure buffer system – reduce the blood fluctuation during the daily events, such as changing of the posture, respiration, excitement, and so forth.
(6) Baroreceptor Resetting
Baroreceptor will adapt to the long term change of blood pressure.
That is, if the blood pressure is elevated for a long period of time, several days or years, the set point will transfer to the elevated mean blood pressure.
Obviously, the adaptation of the baroreceptor prevents the baroreceptor reflex from acting as a long term control system.
That makes the baroreceptor system unimportant for long-term regulation of arterial pressure
(2) Reflex involving arterial chemoreceptors
Chemoreceptors: situated in the carotid body and aortic body
They have a very rich blood supply,
which make them ideal for sampling chemical changes in the blood.
Chemoreceptors are sensitive to the decreased Po
2
, increased P
CO2 and increased hydrogen ion concentration in the plasma.
Afferent:
Afferent nerve fibers form the carotid body travel in the carotid sinus nerve, which is a branch of glossopharyngeal nerve.
Aortic body is innervated by the aortic nerve, which is a branch of the vagus
Response: Stimulation of chemoreceptors leads to a reflex increase in vasomotor tone,
which causes generalized vasoconstriction and hence a rise in blood pressure.
Importance: Chemoreceptor mechanism is important in regulation of blood pressure when it fall below the range in which baroreceptors act (70 mmHg).
(3) CNS ischemic response
Chemoreceptor reflex is useful in regulation of blood pressure when it falls to a level between
40 and 70 mmHg.
But if the blood pressure below 40 mmHg, the last ray of hope for survival is the central nervous system (CNS) ischemia response.
So it sometimes called the “last ditch stand” pressure control mechanism.
As the name indicates, it is evoked by ischemia
(poor blood flow) of the central nervous system.
CNS ischemia reduces blood flow to the vasomotor centre (VMC).
Reduction in blood flow to the VMC leads to reduced Po
2 region. and elevated Pco
2 in the medulla
Both these factors stimulate the VMC directly, leading to vasoconstriction and consequently rise in blood pressure.
II Chemical and hormonal control of cardiovascular function
Introduction
Various hormones, chemicals
Start at a low pace ,
Have long-lasting influences on cardiovascular function.
Hormones and chemicals are classified into two groups
Vasoconstrictors
Vasodilators
Vasoconstrictors and Vasodilators
Vasoconstrictors
Epinephrine and Norepinephrine
Angiotensin II
Vasopressin
Vasodilators
EDRF (NO)
Epinephrine and Norepinephrine
The adrenal medulla secrete both epinephrine (80%) and norepinephrine
(20%)
carried by blood flow to everywhere in the body.
In the blood, only a little norepinephrine comes form the endings of the adrenergic fibers.
Adrenergic receptors
Epinephrine
Norepinephrine
α
1 receptor on vessels
β
1 receptor on heart
β
2 receptor on vessels
(skeletal muscle and liver)
Vasoconstriction
Positive effect
Vasodilation
Effect
On heart in vitro (contractility and automaticity).
both increase the force and rate of contraction of the isolated heart.
mediated by β1 receptors.
Effect
On peripheral resistance .
Norepinephrine produces vasoconstriction in most if not all organs via α1 receptors
epinephrine dilates the blood vessels in skeletal muscle and the liver via β2 receptors.
overbalances the vasoconstriction produced by epinephrine elsewhere, and the total peripheral resistance drops.
Effect
On heart in vivo (heart rate and cardiac output) .
When norepinephrine is infused introvenously
the systolic and diastolic blood pressure rise.
The hypertension stimulates the carotid and aortic baroreceptors,
producing reflex bradycardia that override the direct cardioacceleratory effect of norepinephrine.
Consequently, the heart rate and cardiac out falls.
Effect
On heart in vivo
Epinephrine causes a widening of the pulse pressure
baroreceptor stimulation is insufficient to obscure the direct effect of the hormone on the heart,
cardiac rate and output increase.
Angiotensin II
very potent vasoconstrictor
formed in the plasma through a chain reaction.
The chain is triggered by a substance, renin, released form kidneys.
Renin is released from kidneys in response to renal ischemia , which may be due to a fall in blood pressure.
Effect of Angiotensin II
powerful constrictor
release aldosterone from the adrenal cortex
acts on the brain to create the sensation of thirst.
inhibit the baroreceotor reflex and
increase the release of norepinephrine from the sympathetic postganglionic fiber.
Vasopressin
Also called antidiuretic hormone (ADH),
formed in the hypothalamus (mainly)
secreted through the posterior pituitary gland.
even more powerful than angiotensin as a vasoconstrictor.
The high concentration of vasopressin during hemorrhage can raise the arterial pressure as much as 40 to 60 mmHg.
Vasopressin
The amount of endogenous vasopressin in the circulation of normal individuals does not normally affect blood pressure.
it does not increase blood pressure when small doses are injected in vivo
Acts on the brain to cause a decrease in cardiac output.
(in the area of postrema, one of the circumventricular organs)
Acts on the kidney
Endothelium – Derived Relaxing Factor
Metabolism
Effect of NO
Relax the vascular smooth muscle directly
Mediate vascular dilator effect of some hormones and transmitters (Ach, bradykinin, VIP, substance P)
Inhibit the tonic excitation of some neurons in the vasomotor centre.
Inhibit the norepinephrine release from the sympathetic postganglionic fiber.
One or more of these effects are physiological.
III Autoregulation of Local Blood
Pressure
Role of Vasodilator Substances.
CO
2
, Lactic acid, Adnosine, Adnosine phosphate compounds, Histamine, K + and H +
Myogenic Activity
Heterometric autoregulation
IV Long-Term mechanism for
Arterial Pressure Regulation
Renal –body Fluid Mechanism
V Summary of the Integrated
Multifaceted System for
Arterial Pressure Regulation
Introduction
• Arterial pressure is regulated but by
several interrelated systems
• each of which performs a specific function.
If the blood pressure drops suddenly
two problems confronts the pressure control system
The first is survival,
to return the arterial pressure immediately to a high enough level
that the person can live trough the acute episode.
If the blood pressure drops suddenly
The second is to return the blood volume eventually to its normal level
so that the circulatory system can reestablish full normality,
including return of the arterial pressure all the way back to its normal value
Three kind of mechanisms in regulating the blood pressure
react rapidly, within seconds or minutes;
respond over an intermediate time period, minutes or hours
provide long-term pressure regulation, days, months, and years.
1, Rapidly Acting Pressure Control Mechanisms,
Acting Within Seconds or Minutes
The baroreceptor feedback mechanism.
The central nervous system ischemic mechanism.
The chemoreceptor mechanism
Effect of Rapidly Acting Pressure
Control Mechanisms
To cause constriction of the veins and provide transfer of blood into the heart.
To cause increased heart rate and contractility of the heart and provide greater pumping capacity by the heart
To cause constriction of the peripheral arterioles to impede the flow of the blood out of the arteries.
All these effects occur almost instantly to raise the arterial pressure back into a survival range.
2. Pressure Control Mechanisms
That Act After Many Minutes
The renin-angiotensin vasoconstrictor mechanism
Stress-relaxation of the vasculature
Shift of fluid through the tissue capillary wall in and out of the circulation to adjust the blood volume as needed.
(1) The renin-angiotensin vasoconstrictor mechanism
(2) Stress-relaxation of the vasculature
When the pressure in the blood vessels becomes too high,
they become stretched and keep on stretching more and more for minutes or hours;
as a result, the pressure in the vessels falls toward normal.
This continuing stretch of the vessels, called stress-relaxation, can serve as an intermediateterm pressure “buffer”.
(3) Shift of fluid through the tissue capillary wall in and out of the circulation
• any time the capillary pressure falls too low,
• fluid is absorbed by capillary osmosis from the tissue into the circulation,
• thus building up the blood volume and increasing the pressure in the circulation.
Pressure Control Mechanisms
That Act After Many Minutes
become mostly activated within 30 minutes to several hours.
can last for long periods, days if necessary.
During this time, the nervous mechanisms usually fatigue and become less and less effective
3, Long-Term Mechanisms for
Arterial Pressure Regulation
The renal –blood volume pressure control mechanism.
Aldosterone
Importance
It takes a few hours to show significant response for these mechanisms.
Return the arterial pressure all the way back.