Cardiovascular 12 – Regulation of the CVS
advertisement
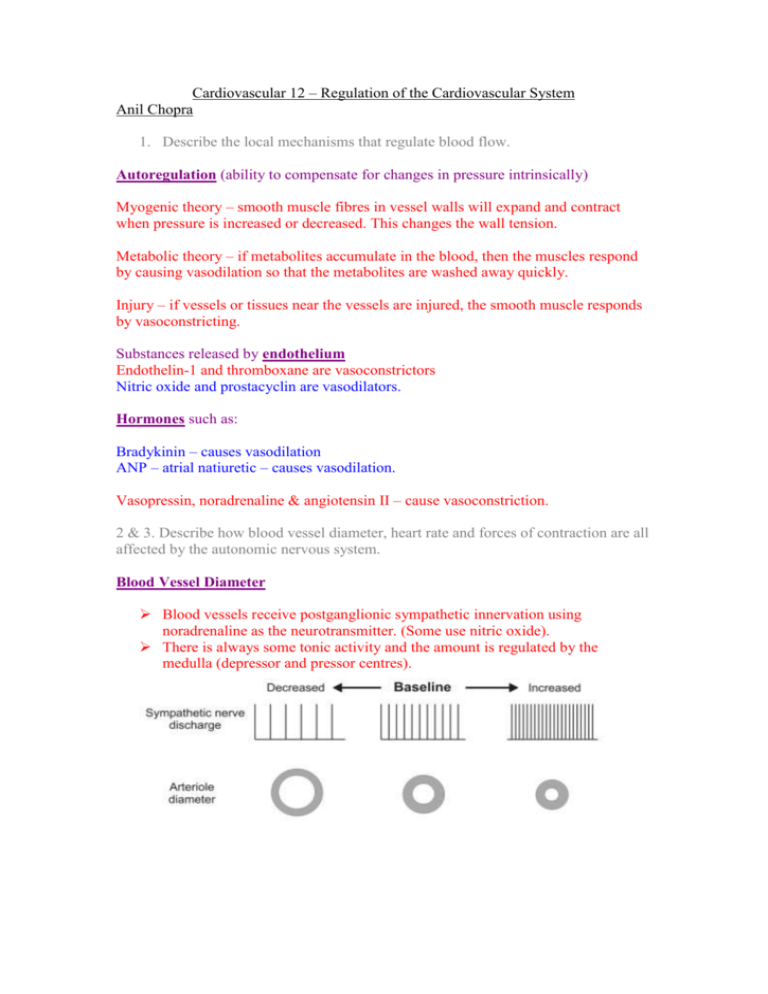
Cardiovascular 12 – Regulation of the Cardiovascular System Anil Chopra 1. Describe the local mechanisms that regulate blood flow. Autoregulation (ability to compensate for changes in pressure intrinsically) Myogenic theory – smooth muscle fibres in vessel walls will expand and contract when pressure is increased or decreased. This changes the wall tension. Metabolic theory – if metabolites accumulate in the blood, then the muscles respond by causing vasodilation so that the metabolites are washed away quickly. Injury – if vessels or tissues near the vessels are injured, the smooth muscle responds by vasoconstricting. Substances released by endothelium Endothelin-1 and thromboxane are vasoconstrictors Nitric oxide and prostacyclin are vasodilators. Hormones such as: Bradykinin – causes vasodilation ANP – atrial natiuretic – causes vasodilation. Vasopressin, noradrenaline & angiotensin II – cause vasoconstriction. 2 & 3. Describe how blood vessel diameter, heart rate and forces of contraction are all affected by the autonomic nervous system. Blood Vessel Diameter Blood vessels receive postganglionic sympathetic innervation using noradrenaline as the neurotransmitter. (Some use nitric oxide). There is always some tonic activity and the amount is regulated by the medulla (depressor and pressor centres). Heart Rate & Force of Contraction Sympathetic stimulation results in an increased heart rate and also causes a large Ca2+ influx into the cells on influx as well as increasing intracellular stores of Ca2+. This results in an increased force of conduction. Stroke volume is also increased with increased venous return and decreased intrathoracic pressure (both increase end-diastolic ventricular volume). Parasympathetic stimulation results in decreased heart rate and does not increase contraction force. 4. State the location of the Baroreceptors. Baroreceptors in the carotid sinus & aortic arch. 5. Define cardiac output, stroke volume, mean systemic arterial pressure and state the determinants. Cardiac output: Vol of blood pumped out of the heart per minute CO = SV x HR (stroke volume x heart rate) Stroke volume: Vol of blood ejected on each pump SV = EDV – ESV (End diastolic volume – end systemic volume). Mean systemic arterial pressure: arterial pressure used; NOT average. MAP = CO x TPR (cardiac output x total peripheral resistance) MAP = DP x 1/3PP (diastolic pressure x 1/3 pulse pressure) 6. Indicate how Baroreceptors control blood pressure. Increase in Blood pressure Increased Stretch of baroreceptors Afferent pathway of vagus nerve and glossopharyngeal nerve Medulla oblongata Decrease in Blood pressure Decreased Stretch of baroreceptors Afferent pathway of vagus nerve and glossopharyngeal nerve Medulla oblongata Increases parasympathetic activity to heart and decreases sympathetic activity to heart and vessels Increases sympathetic activity to heart and decreases parasympathetic activity to heart. 7 & 8. Describe the changes in impulse activity in the carotid sinus nerve, parasympathetic and sympathetic stimulation nerves following an increase or decrease in blood pressure & construct an integrated picture of the various systems that control blood pressure and be able to apply this to specific clinical examples involving blood loss or fluid overload. Maintaining arterial pressure Mean systemic arterial pressure = cardiac output x total peripheral resistance Arterial pressure haemorrhage Cardiac output Heart rate CO = HR x SV Stroke volume Arterial pressure Ventricular end diastolic volume Venous return Venous pressure Firing of baroreceptors Parasymp discharge to heart Reflexes Peripheral resistance Cardiac contractility Venous tone Symp discharge to heart Symp discharge to veins Arteriolar constrictio n Symp discharge to arterioles Decrease in Blood pressure Increase in Blood pressure