Obesity. Diet, Exercise and Drugs. How much pain?
advertisement

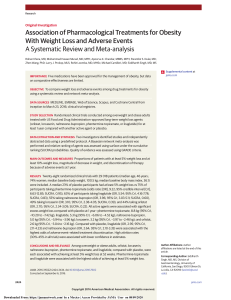
Obesity. Diet, Exercise and Drugs. How much pain? How much Patrick English gain? Consultant Physician. Derriford Overview • Dietary intervention – Effectiveness of major studied interventions • Exercise – Major studied interventions – Metabolic effects – Weight loss effects • CombinedStrategies-LookAHEAD • Pharmacotherapy – GLP-1 and Orlistat – Newer agents Dietary interventions • Energy restriction – VLCD – LCD – Liquid meal replacements • Mediterranean • Low CHO/Low GI/Low fat/Macronutrient restriction/freedom Dietary interventions • Goal is maintenance of weight loss achieved • Few studies of good quality and long duration • Energy restriction is ultimately the key Low GI: Cochrane Review 2009. Low glycaemic index or low glycaemic load diets for overweight and obesity • 6 RCTs Low GI vs standard with 202 participants, 5/5226/52 duration • Possible small benefit with low GI – 1 kg greater WL at 6/12 – TC -0.22mM – LDL -0.24mM • unconvincing Low CHO. Obesity Reviews 2009. Hession • Low CHO/High protein vs Low fat/Low Cal/Higher CHO • Systematic review 2000-2007 • Adults , Mean BMI ≥28, duration > 6/12 • 13 studies-longest 36/12, total number 1022 patients • Attrition rate 36% • At 6/12 favours Low CHO -4.02kg • At 12/12 Favours low CHO -1.05 kg • In the one trial to go to 3 yrs-no difference Mediterranean: Shai NEJM 2008 • Low CHO vs LF vs Med diet (which was as low in fat as LF) • 2yrs • 322 patients, 52 yo, BMI 31 • Adherence 95.4% 1yr, 84.6% 2y • WL in LF vs Low CHO vs Med = 2.9kg vs 4.7kg* vs 4.4 kg* • inT2DM glucose 1.8mmol/L in Med with HOMA-IR Longer term studies: Douketis IJO 200 • Systematic review-BMI ≥ 25, prespecified approved WL intervention, clinical trial, > 2yrs, > 100 subjects • 16 dietary/lifestyle interventions, 6 with FU = 4yrs. Results based on completers • 5698 subjects, mean age:40-59, Mean wt 78116kg, Attrition 31-64% • 13 studies split induction (3-18/12) then maintenance, 3 studies just induction over 2-4 yrs • <5kg WL after 2-3yrs (3.5±2.4kg, range 0.910kg) • <5kg after 4-7 yrs (3.6±2.6kg, range 1.8-10kg) Liquid meal replacements. Flechtner-Mors Ob Res 2000 • 100 patients BMI-25-40 • 1200-1500 kcal/d restriction with diet vs meal replacement shakes x 2 for 12/52 • 1 x meal replacement shake and snack daily as part of maintenance 4 yrs • Attrition of 42 patients at 2 yrs, 32 persuaded to rejoin • WL 1.3 vs 7.1kg 12/52, 4.1kg vs 9.5kg at 4 y, 75% FU • SBP 13.3 mmHg in intensive gp, glucose fell in both by 0.6-0.65mM Take Home – Different dietary composition little effect long term though suggestive for Low CHO/Med – Adherence and energy content most important – Adherence low with severely CHO restricted diets at 1 year (< 50% vs 60=% with other approaches) – Interventions with large weight loss up front with lifestyle change subsequently may have a bigger effect 1. – Astrup Lancet 2004; counselling 364:897-9 2. Dansinger JAMA 3. Dansinger Ann Intas Med Dietary has2005; a 293:43-53 modest effect 2007: 147:41-50 4. Astrup Obes Rev 2000; 1:17-19 5. Anderson Am J Clin Nut 2001; 74:579-84 stand alone intervention (-1.9 BMI units 3) Exercise/Activity-Studied interventions • Resistance training • Aerobic training – Long duration – Short duration • HIT Metabolic/Weight loss effects of Resistance Training • Resistance training – Poorly studied for weight loss2 – Intensity and duration not clearly defined – Better studied in type 2 diabetes and lowers HbA1c 0.57% (6 mmol/mol)1 – Has greater effect if > 150 mins week1 – Combined with AET may be more effective than AET alone (muscle mass) in reducing VAT2 – New trial underway-Washburn et al Contemp Clin Trials July 2012 Metabolic/Weight Loss effects Aerobic training • The more you do, the harder you go, the more you get1, 2 but effects are modest2 • Increased physical activity and fitness improves health risk independent of weight1,2 but does not completely alleviate effects of weight1 • Unfit lean men double risk mortality vs fit lean men3 (1.8/1000 man yrs vs 3.6) • Unfit men with waist <87cm higher mortality than fit men waist > 99cm (7.8/1000 man years vs 1.9)3 • In DM unfit men of all weight categories 2.7-2.8 x mortality of those with high fitness levels and normal weight4 • Limited data on those with BMI > 354, 5 1. Jakicic Obesity Dec 2009 2. Shaw K. Cochrane Database Syst Rev 2009 3. Lee CD Am J Clin Nutr 1999. 4. Church Metabolic/Weight Loss effects Aerobic training • Typically 0.5-3kg weight loss with physical activity alone1 • If supervised activity 45mins/daily for 16 months M lost 5.2kg v 0.5kg no exercise, W 0.6kg increase vs 2.9kg increase2 • Effect of exercise interventions less than that if dietary interventions, 4kg vs 7.2kg at 1 year 1, 3 • Combined intervention more effective still in short term studies 1, 4 0.6% placebo vs 8.4%/5.5% (M/F) exercise vs 11.4%/7.5% combined 1. Jakicic Obesity Dec 2009 2. Donnelly Arch Int Med 2003 3. Wood PD NEJM 1988 4. Hagan Med Sci Sports Exerc 1986 Effects of Physical activity (aerobic) on long term weight loss/maintenance • Following weight loss 33-50% lost weight is regained in 1218 months1 • Physical activity may be critical in weight loss maintenance2 • Those maintaining 10% weight loss at 24 months reported performing 275 minutes of activity above baseline levels2 (338 mins vs 63 mins) • Those who failed to maintain weight loss increased by 74 mins/week (128 mins vs 54 mins)2. • NWCR-those who maintained 13.6kg WL > 12 months reported >2,800kcal/wk of LTPA3 • 76% of those who maintain weight loss report using physical activity as a WL strategy4 1. Jakicic Obesity Dec 2009 2. Jakicic Arch Int Med 2008 3. KlemAm J Clin Nutr 1997 4. Kayman Am J Clin Nut 1990 Exercise and prevention of weight gain • Australian Longitudinal study of womens health1: – 8726 18-23 yo F followed for 4 yrs – 41% gained ≥ 5% BW – Sitting > 33hrs/wk increased risk of weight gain by 20% • Healthy Worker Project2 – avge weight gain 0.6kg F and 0.4kg M over 2 yrs – 1 extra walking session/week reduced wt of 0.8kg F and 0.4kg M 1. Ball K Int J Obes Relat Metab Disord 2002 2. French S Int J Obes Relat Metab Disord 1994 HIT (Panorama) • All out intervals > 90% VO2 peak, seconds to minutes with recovery period • Classically Wingate Test-30s all out vs high force on cycle ergometer 4-6 rpts with 4 min recovery • Used 3x weekly for 2-6/52 – At 2/52 2x duration effort at 80% base VO2 peak (26-51 mins) – Improves oxidative capacity mitochondrial enzymes 15-35% (euivalent to 10.5 hrs endurance training), increases GLUT-4 expression and muscle glycogen • Not used as weight loss strategy but Summary-Activity/Exercise and obesity • The more you do and the harder you do it the more weight loss you get • Health benefits accrue from improved fitness as well as weight loss • Required levels of activity are more than most suppose • Most people struggle to achieve activity targets so strategies targeted at improving adherence required • The more contact people have the better they do Studies that help us in real world Counterweight Look AHEAD • www.counterweight.org • Primary care led • OMA training practice nurses in 20 practices • Groups (1 hrs) and 1:1 (1030 minutes each) • 6 appointments in 3 months, then at least quarterly • Lifestyle but pharmacotherapy available • Links with supporting physician/dietitian • Diabetes Care 30:1374-1383, 2007 • Obesity 14: 737-752 2006 • Arch Int Med 170: 1566-75 2010 • 0-6months: weekly visits, 3 group, 1x1:1. • 7-12 months: 3 visits/m, 2 group, 1x 1:1 (?Orlistat) • 2-4 yrs: 1 face to face 1:1/m, 1 x email/phone, refresher groups/ campaigns • 5+yrs: monthly individualised contact/refresher groups/campaigns What do they have in Common? • Based on evidence of what works • Clear structure to programme • Emphasis on motivation and engagement of patient • Use of goal setting and structured meal plans with calculated energy deficits • More frequent contact than usually afforded in everyday practice • The use of pharmaceutical agents if lifestyle alone did not achieve goals What did they achieve? Counterweight • 47.9% with 1 year follow up data • Mean weight change -3.0kg • 30% had 5% weight loss (40% high attenders) • Estimated 6.3% of prescribing costs (8.4% in high attenders) • Savings cover 40% of programme costs What did they achieve? Look AHEAD 1 yr • 97.1% 1 year follow up exam • Mean 8.6% weight loss (0.7% C) • 37.8% had > 10% weight loss (3.2% control) • 68% > 5% weight loss • HbA1c 7.3 6.6% (0.14% C), use of medicines 7.8% ( 2.2% C), BP 7/3, TG and cholesterol and % with MS 93.678.9%) • fitness 20.9 vs 5.8% • Look AHEAD 4 year • 93% assessed in each of the 4 years • Mean 6.15% WL (0.88% control) • HbA1c 0.36% ( 0.09 % controls) • Less medication use-if no OHG at baseline only 42% using at 4 yrs vs 67% in controls Look AHEAD good news • Percentage of people meeting all 3 treatment goals for BP, HbA1C and LDL – 10.823.6% ILI vs 9.5 16.0% C – fitness and weight in controls – Controls got baseline education and 3 group sessions in one year and this was enough for substantial improvements from baseline OK-some drugs • GLP-1 • Orlistat • Phentermine/Topiramate Phase 3 studies underway-awaiting approval • Tesofensine –phase 3 x2 underway • Bupropion/Naltrexone, Buproprion/Zonisamideawaiting approval • Pramlintide & combinations Orlistat license • BMI > 30 or >28 with risk factors • Need to lose 2.5kg prior to treatment removed from license • Need to lose 5% bodyweight at three months to continue treatment longterm • Reconsider if significant regain occurs at any time • NICE recommendation in 2001 Proportion of patients achieving beneficial weight loss with Orlistat over one year (NGT) Patients (%) 100 Placebo + diet (n=340) Orlistat + diet (n=343) p<0.05 80 60 68.5% p<0.05 49.2% 38.8% 40 17.7% 20 0 5% Weight loss (%) 10% Adapted from Sjöström. Lancet 1998; 352: 167-172 (ITT population) Proportion of patients with T2D achieving beneficial weight loss with Orlistat over one year Taken from Miles JM, Diabetes Care 2002;25(7):1123-8 and Kelley DE, Diabetes Care 2002;25(6):1033-41. Weight control is more difficult to achieve in patients with type 2 diabetes Change in BMI (kg/m2) 0 Non-diabetic Diet-treated diabetic Drug-treated diabetic –2 –4 –6 p<0.01 vs non-diabetic –8 –10 Adapted from Khan et al. Reprinted with permission from the North American Association for the Study of Obesity © 2000. Obes Res 2000; 8: 43–8 UK Orlistat Multimorbidity Study Improvements in risk factors Total Chol LDL Chol Sys BP Dias BP OGTT Score Orlistat -0.12 -0.3 -6.0 -5.5 -0.37 Placebo +0.16 -0.02 -2.3 -3.1 +0.09 All differences at least p<0.05 Orlistat-Summary • In NGT patients approx 4-6kg extra weight loss with orlistat vs. placebo short term. • 70% 5% WL and 40% 10% WL • In T2DM approx 50% of this • 10, 631 patietns in 16 studies 1-4 yrs in Cochrane review 2009, with WL approx 2.9 kg v placebo in these1 • Improves cardiovascular risk factors, glycaemia to small extent1. • No CV or mortality data1 1.Padwal; Cochrane Database Syst Rev 2009 Liraglutide Astrup Lancet 2009 • GLP-1 analogue • 1.2-3.0mg vs placebo and orlistat over 20/52 • WL = 4.8kg (1.2mg) vs 5.5.kg (1.8mg) vs 6.3kg (2.4mg) vs 7.2 kg (3.0mg) vs 2.8kg (placebo) vs 4.1 kg (orlistat) at 20/52 • 76% with 3.0mg lost > 5%, vs 41% orlistat vs 30% placebo • Withdrawal rates 19% placebo, 11-22% liraglutide and 17% orlistat. Nausea in 24-47% in those on liraglutide • At 2yrs WL 7.8 vs 5.4 kg Liraglutide vs Orlistat (p=0.09) with SBP 12.5 vs Topiramate/PhentermineQnexa • Topiramate-GABA agonist, unkown action in obesity. SE monotherapy • Phentermine-NA lateral hypothalamus, β2-stumulation, appetite • Combination at 92mg/15mg and 46mg/7.5mg preparations in Phase 3 studies-EQUATE, EQUIP, CONQUER • CONQUER Lancet 2011, Gadde et al • 2487 patients, BMI 27-45 plus 2 comorbidiities • WL 1.4 kg vs 8.1 kg vs 10.2kg (9.8%) with 70% > 5% WL vs 21% placebo depression and anxiety A/Es in high dose group vs low dose group vs placebo (7% vs 4% vs 4%) Tesofensine • Tesofensine – inhibits NA/DA, 5HT re-uptake presynaptically and studied in AD and PD – Phase IIb studies 10.6% WL 24 weeks in 1 mg dose but increased heart rate 7.4bpm • Buproprion inhibits reuptake DA and NA and activates POMC neurons, α-MSH release, appetite • Naltrexone blocks β-endorphin inhibition of POMC α-MSH release • Zonisamide-anit-epilepsy with DA and 5HT activity • Combined with Naltrexone SR 32mg/Bupropion SR 360 mg = Contrave • Phase III studies: COR-I (Greenaway Lancet 2010), II; COR-BMOD, COR-Diabetes – 552 with DM and obesity, A1c 7-10% – WL 5% vs 1.8% – A1c 0.6% • With Zonisamide ? Greater WL in Phase II, Phase III awaited Pramlintide • With Metreleptin-Phase II, 12.7% WL at 20/52 • With Sibutramine • With Phentermine • With Exenatide Summary-Drugs • Orlistat only drug with long term license and profile • Liraglutide looks promising • Others coming through but not greatly increased weight loss over current agents to date. Newer centrally acting drugs in development • Long term use is required and attrition limits effectiveness • Need for hard endpoint studies Adiposity signalling Schwarz Nature vol 404 6 April 2000 The hypothalamus in weight control Schwarz Nature vol 404 6 April 2000 Integrating adiposity and satiety signals Schwarz Nature vol 404 6 April 2000