additional records identified through other sources = # relevant
advertisement
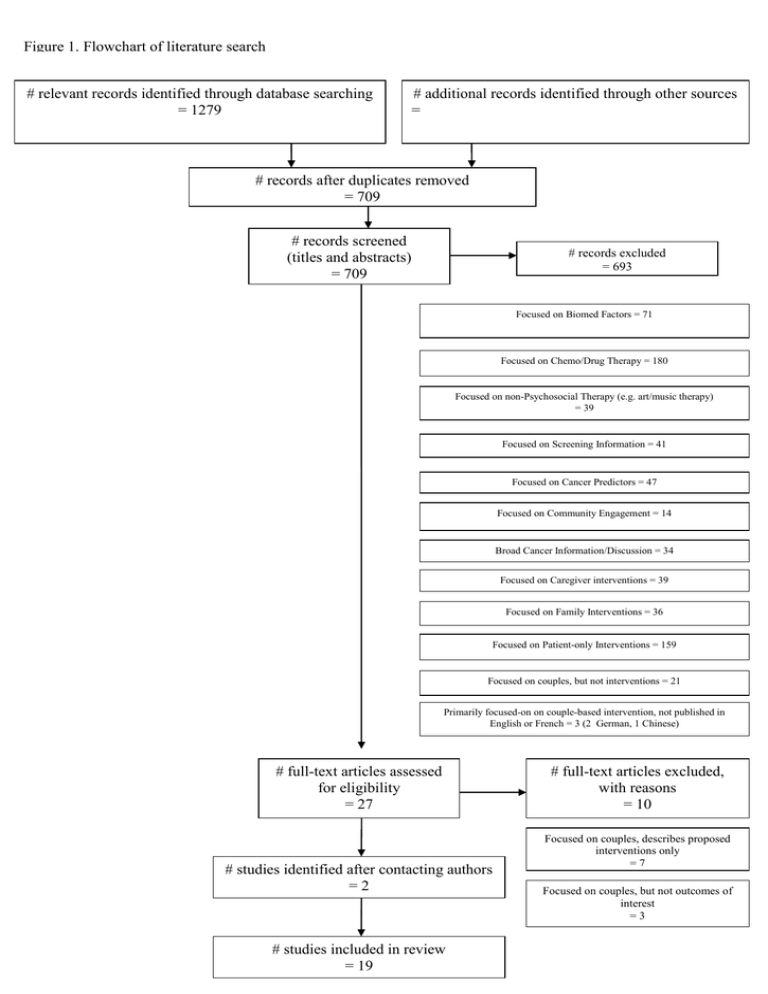
Figure 1. Flowchart of literature search # relevant records identified through database searching = 1279 # additional records identified through other sources = # records after duplicates removed = 709 # records screened (titles and abstracts) = 709 # records excluded = 693 Focused on Biomed Factors = 71 Focused on Chemo/Drug Therapy = 180 Focused on non-Psychosocial Therapy (e.g. art/music therapy) = 39 Focused on Screening Information = 41 Focused on Cancer Predictors = 47 Focused on Community Engagement = 14 Broad Cancer Information/Discussion = 34 Focused on Caregiver interventions = 39 Focused on Family Interventions = 36 Focused on Patient-only Interventions = 159 Focused on couples, but not interventions = 21 Primarily focused-on on couple-based intervention, not published in English or French = 3 (2 German, 1 Chinese) # full-text articles assessed for eligibility = 27 # studies identified after contacting authors =2 # studies included in review = 19 # full-text articles excluded, with reasons = 10 Focused on couples, describes proposed interventions only =7 Focused on couples, but not outcomes of interest =3 Table 1. Summary of couple-based interventions Description of intervention Initial Intervention Program Follow-up Badger et al. (2007) Three-arm intervention trial comparing a Telephone Interpersonal Counselling intervention (TIP-C) with a self-managed exercise intervention (also delivered by telephone) and an Attention Control (AC) group who received printed information on breast cancer. TIP-C involved weekly phone calls that focused on cancer education, social support, awareness and management of depressive and anxiety symptoms, and on changes in participants’ roles in life. Partners in the TIP-C condition received a separate call every second week. Exercise intervention focused on low-impact exercise four times a week. Patients in AC group received brief weekly telephone calls; partners every second week. Six weekly TIP-C sessions (M = 34 minutes) 6 weeks; 10 weeks Badger et al. (2010) Two-arm intervention trial comparing two different telephone-delivered interventions. The Telephone Interpersonal Counselling intervention (TIP-C) intervention involved weekly phone calls that focused on mood and affect, emotional expression, interpersonal communication and relationships, social support, and cancer information. Partners received a separate call every second. Health Education Attention Condition (HEAC) involved weekly phone calls for patients, and bi-weekly phone calls partners. Participants received written materials from the National Cancer Institute regarding prostate cancer diagnosis and treatments, nutrition, exercise, and quitting smoking. No counselling was offered in this condition. 8 weekly phone calls (patients); 4 bi-weekly phone calls (partners) 8 weeks; 16 weeks Baucom et al. (2009) Relationship Enhancement (RE): places emphasis on viewing the couple as a unique and dynamic unit. Content is tailored to the specific needs of the individuals in each couple. Couples are taught problem-solving skills regarding medical treatments and their relative practical implications for everyday life, emotional expressiveness skills to facilitate active listening and discussion of particular breast cancer issues, and are encouraged to seek positive meaning and existential growth from their cancer experience Six 75-minute biweekly sessions 12-months Budin et al. (2008) Four-arm intervention comparing: disease management (DM); disease management and standardised psychoeducation (SE); disease management and telephone counselling (TC); disease management and standardised psychoeducation and telephone counselling (SE + TC). The DM intervention served as the control condition and involved the delivery of standard treatment protocol. The SE intervention involved the presentation of four psychoeducation videos that addressed coping with diagnosis, recovering from surgery, adjuvant therapy, and ongoing recovery. The TC intervention was designed to increase the patient’s and the partner’s sense of control over the cancer experience. Four phase-specific TC sessions were tailored and delivered separately to patients and partners. The SE+TC intervention combined DM with the SE videos and the TC framework. Telephone counselling (TC), standardised education (SE), TC+SE, and disease management (DM) was phase specific: delivered when participants entered new phase (T0/T1baseline/diagnosis, T2 – postsurgery, T3 – adjuvant therapy, T4 – ongoing recovery Varied depending on treatment course Description of intervention Initial Intervention Program Follow-up Campbell et al. (2006) Telephone coping skills targeting African-American prostate cancer survivors and their partners. A coping skills training intervention (CST) delivered by telephone was compared to a usual care (control condition). CST specifically aimed to provide information about prostate cancer and its’ long-term effects, teach problem-solving skills, and provide training in cognitive and behavioural coping skills. Six weekly 60-minute Coping Skills Training (CST) sessions Postintervention Donnelly et al. (2000) A pre-post pilot study of an intervention using interpersonal psychotherapy (IPT) by telephone for patients with advanced breast cancer. IPT focuses on exploring the psychosocial and physical impact of cancer and treatment, preparing the patient and partner for future events related to treatment, encouraging communication, improving emotional expression, fostering independence, facilitating coping, and optimizing social support. Weekly sessions (M=16 patients, M=11 partners) during chemotherapy, Postintervention Kayser, Feldman, Borstelmann, & Daniels (2010) Partners in Coping Program (PICP) was provided by a trained therapist in fortnightly sessions. Sessions followed various themes including improving coping ability, supportive communication and sexual functioning, assessing couples’ social support, and caring for children. Standard Social Work Services (SSWS) couples were provided with the contact details of a social worker who could link them to various services including individual and family counselling, community support services. Nine 60-minute biweekly over an average of 5 months n/a Kuijer et al. (2004) Focus on the enhancement of relationship equity in order to improve relationship quality and decrease psychological distress . An experimental group was compared with a wait-list control group. The intervention was led by a psychologist and couples were encouraged to discuss openly their relationship before and after the cancer diagnosis and their own views of problems in their relationship and potential solutions. They were given homework tasks to complete where they detailed their ideal support wishes, the goal being to enhance supportive communication and to highlight any existing inequities in their own relationship. Five 90-minute biweekly sessions 3-months Kurtz et al. (2005) A 20-week symptom-management intervention that included five face-to-face sessions and five telephone sessions with a trained nurse was compared to a usual-care control group. The intervention focused on reviewing the physical and psychological symptoms experienced by the patient, the involvement of their partner in managing these, and outlining specific guidelines for both patient and partner to follow to best manage these symptoms. These guidelines were revisited and reassessed at each follow-up. 10 contact (5 face-to-face, 5 telephone) over 20 weeks 10 weeks; 20 weeks Description of intervention Initial Intervention Program Follow-up Manne et al. (2005) Investigated the efficacy of a couple-based group intervention for women with breast cancer. The intervention focused on enhancing supportive exchanges between patients and their partners, and developing coping skills. Session themes included couple-level stress management, couple-focused coping, issues with sexuality, communication skills, and planning for post-treatment life. Six 90-minute weekly 6-months McCorkle et al. (2007) A prospective randomised controlled trial comparing standardised nursing intervention protocol (SNIP) with a usual care (control) condition for patients and spouses following a radical prostatectomy. SNIP focuses monitoring and managing symptoms, teaching self-care, encouraging use of community resources and supportive relationships, and counselling patients and family members. Patients’ and partners’ needs (psychosocial and physical) are addressed individually, and specific strategies for providing support are discussed. Couple-based strategies are also discussed and a shared management plan is devised. 16 contacts (8 in-home, 8 telephone) over 8 weeks, SNIP 3-months; 6 months McLean et al. (2008) A pilot study with a cohort of couples where patients had been diagnosed with a variety of advanced cancer types. The intervention presented to couples was an adaptation of Emotionally Focused Couple Therapy (EFT) that had been specifically formulated for patients with advanced cancer and their partners. EFT emphasises the sharing of emotions, and in the context of an advanced cancer diagnosis, normalizing feelings of separation by clarifying patients’ and partners’ insecurities and restructuring their communication styles. 8-20 sessions of EFT After four sessions; After eight sessions; 3 months postintervention McLean et al. (2011) The intervention presented to couples was an adaptation of Emotionally Focused Couple Therapy (EFT) that had been specifically formulated for patients with advanced cancer and their partners. EFT emphasises the sharing of emotions, and in the context of an advanced cancer diagnosis, normalizing feelings of separation by clarifying patients’ and partners’ insecurities and restructuring their communication styles. Eight, one-hour weekly sessions 8 weeks; 12 weeks Nezu et al. (2003) Problem-solving therapy for patients and a ‘supportive other’ (defined as PST-SO) with problem-solving therapy for patients only (PST) with and with a wait-list control group. PST focuses on teaching couples to identify the precise nature of problems faced, producing a range of solutions, evaluating and understanding consequences of particular actions and proceeding with the most favourable, and then monitoring the outcomes of the chosen solution. PST/PST-SO: Ten 90-minute weekly sessions 6 and 12months Northouse et al. (2005) Description of intervention Initial Intervention Program Follow-up The FOCUS program consists of five central components: family involvement, optimistic attitude, coping effectiveness, uncertainty reduction and symptom management. Initial phase: Three 90-minute home visits spaced one-month apart 3 and 6months Booster phase: Two phone calls to both patient and caregiver (~30 minutes/call) provided after 3month follow-up Northouse et al. (2007) The FOCUS program consists of five central components: family involvement, optimistic attitude, coping effectiveness, uncertainty reduction and symptom management. Three 90-minute home visits and two phone calls to both patient and caregiver (~30 minutes/call) spaced 2-weeks apart, between baseline and 4-month follow-up 4 and 8months Northouse et al. (2011) The FOCUS program consists of five central components: family involvement, optimistic attitude, coping effectiveness, uncertainty reduction and symptom management. Breif FOCUS: 2 x 90-minute home visits, one 30 minute phone call 3 months; 6 months Extensive Focus: 4 x 90-minute home visits, two 30 minute phone calls Porter et al. (2009) A partner-assisted emotional disclosure (PAED) intervention was compared with a partner-assisted educational (EDU) intervention for patients with gastrointestinal cancer and their partners. The intervention focused on decreasing the ‘holding back’ of cancer-related disclosures to partners, increasing relationship quality and intimacy, decreasing psychological distress. The PAED intervention involved training couples in effective disclosure of their cancer-related concerns. Patients were asked to describe a particular cancer experience to their partner in detail. The partner’s role was to support the patient’s disclosure, and they were instructed to empathise with and understand the particular experience, avoid problem-solving, and use reflective listening. Couples in the EDU intervention also attended four sessions with a therapist, but received general cancer information only. 4 face-to-face sessions Scott, Halford, & Ward (2004) Description of intervention Initial Intervention Program Follow-up Three-arm intervention, consisting of a Medical Information (MI) intervention, a Patient Coping training (PC) intervention, and the CanCOPE intervention. The MI intervention involved the provision of educational materials regarding patients’ particular cancer and associated treatments, as well as five brief telephone calls. No specific psychological intervention was administered in the MI intervention. The PC intervention combined the educational materials from the MI intervention with supportive counselling and education in coping skills (e.g. problem solving skills, identification of negative thinking) from a registered psychologist. CanCOPE had a similar focus to the PC intervention, though it was undertaken with couples to enhance coping and support between patient and partner, primarily through the teaching of supportive communication skills. MI: Five 15-minute phone calls, medical information booklets 6 and 12months PC: Four 2-hour sessions: pre & post-surgery, 1 week & 6-months after; Two 30-minute phone calls 1 & 3-months post-surgery CanCOPE: Five 2-hour sessions: pre & post surgery, 1 week, 5 weeks & 6-months after; Two 30minute phone calls 1 & 3-months post-surgery Table 2. Delivery of couple-based interventions Total length Total length of of Delivery of Author intervention intervention intervention (minutes) (minutes) patient partner Badger et al. (2007) Badger et al. (2010) Telephone; separate Telephone; separate 204 304 102 180 Experience of Intervention Deliverers Undergo specific training to deliver intervention? Followed specific protocol to deliver intervention? Outline plans to maintain treatment fidelity Psychiatric Nurse Counsellor (with oncology expertise) No Yes Yes TIP-C: Masters-level nurse; social worker with psychiatric and oncology expertise No Yes Yes Advanced doctoral students in clinical psychology, trained in couple therapy and the effects of cancer on relationships No Yes Yes Nurse Yes Yes Yes African-American, doctoral level medical psychologist Yes, systematic training of 6 the intervention sessions Yes Clinical psychologist undertaking post-doctoral fellowship in psychooncology Yes, 4-session seminar, 4day worshop, study of intervention manual Yes HEAC: research assistants Baucom et al. (2009) Face-toface; counsellor Budin et al. (2008) Telephone & face-toface & videos; separate Campbell et al. (2006) Telephone Donnelly et al. (2000) Telephone 450 360 450 360 Yes Total length of intervention (minutes) patient Total length of intervention (minutes) partner 540 Author Delivery of intervention Kayser et al. 2010 Face-toface; counsellor 540 Kuijer et al. (2004) Face-toface; counsellor 450 Kurtz et al. (2005) Face-to-face and telephone Manne et al. (2005) Face-toface; group McCorkle et al. (2007) Face-to-face and telephone McLean et al. (2008) Face-toface; counsellor McLean et al. (2011) Face-to-face Experience of Intervention Deliverers Undergo specific training to deliver intervention? Masters-level clinical social worker Followed specific protocol to deliver intervention? Outline plans to maintain treatment fidelity Yes Yes Yes, 8-hour training program 450 540 480 540 480 Psychologist No Yes No Nurse No Yes Yes Unclear - Group intervention lead by a small team of therapists (20 therapists used in total) Yes, 6-hour training program Yes Yes Advanced Practice Nurses, board certified nurse practioners No Yes No Psychologists; doctoral candidate No Yes No Psychologist Trained in Emotion Focused Therapy Yes No Total length of intervention (minutes) patient Total length of intervention (minutes) partner Experience of Intervention Deliverers Undergo specific training to deliver intervention? Followed specific protocol to deliver intervention? Outline plans to maintain treatment fidelity Yes, 15-hour training program Yes Yes Yes Yes Yes Masters-level nurse Yes, 40-hour training program Yes Yes Masters-level nurse Yes, 40-hour training program Yes Yes Masters-level therapist (social worker or psychologist) No Yes Yes Three female psychologists, experience ranged from 3-15 years No Yes Yes Author Delivery of intervention Nezu et al. (2003) Face-toface; counsellor 900 900 15 advanced psychology graduate students & 3 social workers (all had minimum masters degree and two years field experience) Northouse et al. (2005) Face-toface; counsellor 330 330 Masters-level nurse Northouse et al. (2007) Face-toface; counsellor 330 Brief FOCUS: 210 330 Brief FOCUS: 210 Northouse et al. (2011) Face-toface; counsellor Porter et al. (2009) Face-toface; counsellor 210 210 Scott et al. (2004) Face-toface; counsellor 660 /14660 Extensive FOCUS: 420 Extensive FOCUS: 420 Table 3. Description of Patients and Partners Patients Partners 54.27 (6.44) 53.20 (4.51) 71.86 55.20 Caucasian 81.59 85.08 African-American 10.96 5.88 Hispanic 3.08 2.98 Asian 1.36 1.54 Other 3.01 4.34 Breast 49.83 Prostate 21.07 Gynaecological 2.17 Lung 9.74 Head & Neck 0.50 Leukaemia 1.63 Non-Hodgkins 0.17 Hodgkins 0.13 Gastrointestinal 11.12 Brain 0.33 Other 3.30 Stage I 27.72 Stage II 25.91 Stage III 21.18 Stage IV 25.19 Mean, SD, Age (years) Gender, % female Ethnicity, % Cancer Site, % Cancer Stage, % Partner Relationship, % Spouse 85.85 Family Member 10.32 Friend 3.83 High School or less 31.45 30.67 Some university/University graduate 68.54 69.33 Education, % Table 4. Patient Outcome Measures Author QoL Badger et al. (2007) Badger et al. (2010) Spiritual well-being: subscale of Quality of Life-Breast Cancer Psychological Distress Depression: Centre for Epidemiologic al Studies Depression Scale (CESD) Anxiety: Positive and Negative Affect Schedule (PANAS; ); SF-12; Index of Clinical Stress Depression: Centre for Epidemiologic al Studies Depression Scale (CESD) Anxiety: Positive and Negative Affect Schedule (PANAS; ); SF-12; Index of Clinical Stress Physical Distress UCLA Prostate Cancer Index; Multidimen sioanl Fatigue Inventory (MFI) Sexuality Social Adjustment Social wellbeing scale; Perceived Social SupportFamily scale (PSS-FA) Marital Functioning Appraisal Coping SelfEfficacy Communication Problem solving Author Baucom et al. (2009) Budin et al. (2008) QoL Psychological Distress Brief Symptom Inventory; Posttraumatic Growth Inventory; Functional Assessment of Cancer TherapyBreast (FACT-B); Self-image scale Psychosocial Adjustment to Illness Scale Self Report (PAIS-SR); Profile of Adaptation to Life Clinical Scale Psychological Well-being subscale (PAL-C) Physical Distress Brief Fatigue Inventory (BFI); Brief Pain Inventory; Rotterdam Symptom Scale Self-rated Health Subscale (SRHS); PAL-C physical symptoms subscale; Breast Cancer Treatment Response Inventory (BCTRI); BCTRI Side Effects Severity subscale Sexuality Social Adjustment Derogatis Inventory of Sexual Functioning (DISF) Marital Functioning Quality of Marriage Index (QMI) PAIS- Vocational, Domestic, Social subscale Appraisal Coping SelfEfficacy Communication Problem solving Author QoL Campbell et al. (2006) Short-Form Health Survey (SF36) Kuijer et al. (2004) Kurtz et al. (2005) Physical Distress Sexuality Expanded Prostate Cancer Index Composite (EPIC) Expanded Prostate Cancer Index Composite (EPIC) Social Adjustment Marital Functioning Impact of Event Scale (IES); Mental Health Inventory (MHI) Donnelly et al. (2000) Kayser et al. (2010) Psychological Distress Functional Assessment of Cancer TherapyBreast (FACT-B) Centre for Epidemiologic al Studies Depression Scale (CESD) Depression: Centre for Epidemiologic al Studies Depression Scale (CESD) 0-10 Ladder Medical Outcomes Study (MOS); Short-Form Health Survey (SF-36) Medical Outcomes Study (MOS); Short-Form Health Survey (SF36) Appraisal Coping SelfEfficacy Self-Efficacy for Symptom Control Inventory (SESCI) Communication Problem solving Author Manne et al. 2005 McCorkle et al. (2007) McLean et al. (2008) McLean et al. (2011) QoL Psychological Distress Impact of Event Scale (IES); Mental Health Inventory (MHI) Depression: Centre for Epidemiologic al Studies Depression Scale (CESD) Beck Depression Inventory (BDI-II) Beck Depression Inventory (BDI-II); Beck Hopelessness Scale (BHS) Physical Distress Cancer Rehabilitati on Evaluation System (CARES) Sexuality Social Adjustment Marital Functioning Appraisal Coping Partner Unsupportiv e Behaviours Scale (from Partner Responses to Cancer Inventory) Cancer Rehabilitatio n Evaluation System (CARES) Cancer Rehabilitatio n Evaluation System (CARES) Revised Dyadic Adjustment Scale (RDAS) Revised Dyadic Adjustment Scale (RDAS) Relationship -Focused Coping Scale (RFCS) SelfEfficacy Communication Problem solving Author QoL Nezu et al. (2003) Clinician Rated Northouse et al. (2005) Functional Assessment of Cancer TherapyBreast (FACT-B); Functional Assessment of Cancer TherapyGeneral (FACT-G); Short-Form Health Survey (SF36) Psychological Distress Clinician Rated: Hamilton Rating Scale for Depression; Self-Report: Profile of Mood States (POMS); Brief Symptom Inventory (BSI) Partner Rated: Katz Adjustment ScaleRelative’s Form (KASR) Physical Distress Sexuality Social Adjustment Marital Functioning Appraisal Coping SelfEfficacy Communication Problem solving Social Problem Solving Inventory (SPSI-R) Functional Assessment of Cancer TherapyBreast (FACT-B); Functional Assessment of Cancer TherapyGeneral (FACT-G); Short-Form Health Survey (SF-36) Brief Coping Orientations to Problems Experienced (BriefCOPE) Uncertainty : Mishel Uncertainty in Illness Scale; Hopelessnes s: Beck Hopelessnes s Scale (BHS) Author QoL Northouse et al. (2007) Functional Assessment of Cancer TherapyGeneral (FACT-G); Short-Form Health Survey (SF36) Northouse et al. (2011) Functional Assessment of Cancer TherapyGeneral (FACT-G); Short-Form Health Survey (SF36) Porter et al. (2009) Psychological Distress Physical Distress Functional Assessment of Cancer TherapyGeneral (FACT-G) Sexuality Social Adjustment Marital Functioning Uncertainty : Mishel Uncertainty in Illness Scale; Hopelessnes s: Beck Hopelessnes s Scale (BHS) Illness: Appraisal of Illness Scale Uncertainty : Mishel Uncertainty in Illness Scale; Hopelessnes s: Beck Hopelessnes s Scale (BHS) Expanded Prostate Cancer Index Composite (EPIC) Risk of Distress Scale (RFD) Profile of Mood StatesShort Form (POMS-SF) Appraisal Quality of Marriage Index (QMI); Miller Social Intimacy Scale (MSIS) Coping Brief Coping Orientations to Problems Experienced (Brief-COPE ) Brief Coping Orientations to Problems Experienced (Brief-COPE ) SelfEfficacy Lewis Cancer SelfEfficacy Scale Communication Lewis Mutuality and Interpersonal Sensitivity Scale Problem solving Author Scott et al. (2004) QoL Psychological Distress Psychosocial Adjustment to Illness Scale Self Report (PAIS-SR); Impact of Event Scale (IES) Physical Distress Sexuality Sexual Self Schema (SSS) for Women; Brief Index of Sexual Functioning (BISF) Social Adjustment Marital Functioning Appraisal Coping Revised Ways of Coping Questionnair e - Cancer Version (WOC-CA) SelfEfficacy Communication Qualitative review of interview; Coded using rapid interaction coding system Problem solving Table 5. Partner Outcome Measures Author QoL Badger et al. (2007) Badger et al. (2010) Baucom et al. (2009) Spiritual well-being: subscale of Quality of Life-Breast Cancer Psychological Distress Depression: Centre for Epidemiological Studies Depression Scale (CES-D) Anxiety: Positive and Negative Affect Schedule (PANAS; ); SF12; Index of Clinical Stress Depression: Centre for Epidemiological Studies Depression Scale (CES-D) Anxiety: Positive and Negative Affect Schedule (PANAS; ); SF12; Index of Clinical Stress Brief Symptom Inventory; Posttraumatic Growth Inventory Physical Distress Sexuality Social Adjustment Marital Functioning Social wellbeing scale; Perceived Social SupportFamily scale (PSSFA) UCLA Prostate Cancer Index; Multidimensioanl Fatigue Inventory (MFI) Derogatis Inventory of Sexual Quality of Marriage Index Appraisal Coping Selfefficacy Communication Problem Solving Author QoL Budin et al. (2008) Profile of Mood States- Short Form (POMSSF); Caregiver Strain Index Campbell et al. (2006) Impact of Event Scale (IES); Mental Health Inventory (MHI) Donnelly et al. (2000) Kayser et al. 2010 Psychological Distress Psychosocial Adjustment to Illness Scale Self Report (PAIS-SR); Profile of Adaptation to Life Clinical Scale Psychological Well-being subscale (PALC) Quality of Life Questionnaire for Spouses (QL-SP); Illness intrusiveness Rating Scale (IIRS) Physical Distress Self-rated Health Subscale (SRHS); PAL-C - physical symptoms subscale Sexuality Social Adjustment PAISVocational, Domestic, Social subscale Marital Functioning Appraisal Coping Selfefficacy SelfEfficacy for Symptom Control Inventory (SESCI) Communication Problem Solving Author Kuijer et al. (2004) Kurtz et al. (2005) Manne et al. (2005) McCorkle et al. (2007) McLean et al. (2008) QoL Psychological Distress Centre for Epidemiological Studies Depression Scale (CES-D) Physical Distress Sexuality Depression: Centre for Epidemiological Studies Depression Scale (CES-D) Beck Depression Inventory (BDIII) Marital Functioning Appraisal Coping Selfefficacy 0-10 Ladder Medical Outcomes Study (MOS); Short-Form Health Survey (SF36) Depression: Centre for Epidemiological Studies Depression Scale (CES-D) Impact of Event Scale (IES); Mental Health Inventory (MHI) Social Adjustment Cancer Rehabilitation Evaluation System (CARES) Cancer Rehabilitation Evaluation System (CARES) Author's own mastery index Partner Unsupportive Behaviours Scale (from Partner Responses to Cancer Inventory) Cancer Rehabilitation Evaluation System (CARES) Revised Dyadic Adjustment Scale (RDAS) Communication Problem Solving Author QoL McLean et al. (2011) Psychological Distress Beck Depression Inventory (BDIII); Beck Hopelessness Scale (BHS); Caregiver Burden Scale (Time subscale); Caregiver Burden Subscale (Difficulty subscale) Physical Distress Sexuality Social Adjustment Marital Functioning Appraisal Coping Selfefficacy Problem Solving Revised Dyadic Adjustment Scale (RDAS) Social Problem Solving Inventory (SPSIR) Nezu et al. (2003) Northouse et al. (2005) Communication Functional Assessment of Cancer TherapyGeneral (FACT-G); Short-Form Health Survey (SF36) Functional Assessment of Cancer TherapyGeneral (FACTG) Expanded Prostate Cancer Index Composite (EPIC) Uncertainty: Mishel Uncertainty in Illness Scale; Hopelessness: Beck Hopelessness Scale (BHS) Caregiving: Appraisal of Caregiving Scale Brief Coping Orientations to Problems Experienced (Brief-COPE ) Lewis Cancer SelfEfficacy Scale Author QoL Northouse et al. (2007) Functional Assessment of Cancer Treatment (FACT-G; alpha .90) Northouse et al. (2011) Functional Assessment of Cancer TherapyGeneral (FACT-G); Short-Form Health Survey (SF36) Porter et al. (2009) Scott et al. (2004) Psychological Distress Physical Distress Functional Assessment of Cancer Treatment (FACT-G; alpha .90) Sexuality Social Adjustment Marital Functioning Uncertainty: Mishel Uncertainty in Illness Scale; Hopelessness: Beck Hopelessness Scale (BHS) Illness: Appraisal of Illness Scale Expanded Prostate Cancer Index Composite (EPIC) Uncertainty: Mishel Uncertainty in Illness Scale; Hopelessness: Beck Hopelessness Scale (BHS) Risk of Distress Scale (RFD) Coping Brief Coping Orientations to Problems Experienced (Brief-COPE ) Selfefficacy Communication Lewis Mutuality and Interpersonal Sensitivity Scale Brief Coping Orientations to Problems Experienced (Brief-COPE ) Quality of Marriage Index (QMI); Miller Social Intimacy Scale (MSIS) Profile of Mood States- Short Form (POMSSF) Psychosocial Adjustment to Illness Scale Self Report (PAIS-SR); Impact of Event Scale (IES) Appraisal Sexual Self Schema (SSS) for Women; Brief Index of Sexual Functioning (BISF) Revised Ways of Coping Questionnaire - Cancer Version (WOC-CA) Qualitative review of interview; Coded using rapid interaction coding system Problem Solving