and TIA Management - Alberta Provincial Stroke Strategy
advertisement
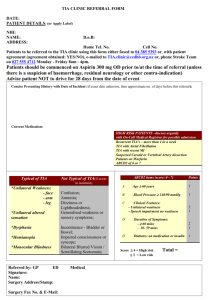
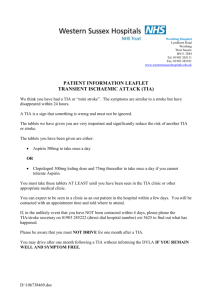
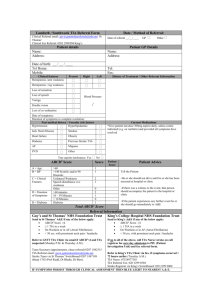
TIA Hotline (ASPIRE Project) and TIA Management Shelagh Coutts BSc, MBChB, MD, FRCP(C) March 13th, 2009 Telehealth Presentation Objectives • What is a TIA and what isn’t? • How can we differentiate high risk from low risk TIAs? What are the data? • How urgently should TIA patients receive diagnosis, assessment, investigation and management? • How to facilitate rapid assessment of TIA? The ASPIRE Project and the TIA Hotline. Patient 1 • Jerome is a 85 year old male with HT, CHF, hyperlipidemia. • Complains of three spells in the previous four days that have been referred as TIAs • Spells involve loss of consciousness • Are these TIAs? Diagnosing ‘spells’ • Phenomenology: before, during, after the event • Was the event witnessed? What did witnesses observe? • What is the setting? (vascular risk factors, elderly, young without risk factors) Patient 1 • Upon rising from seated to standing patient develops a sense of dizziness and unsteadiness and feels very lightheaded • Then experiences blurring of the vision starting peripherally and loses consciousness Patient 1 • Upon rising from seated to standing patient develops a sense of dizziness and unsteadiness and feels very lightheaded • Then experiences blurring of the vision starting peripherally and loses consciousness • Syncope The Definition of Stroke/ TIA • A clinical syndrome characterized by the sudden onset of a focal neurological deficit presumed to be on a vascular basis. Conditions Misdiagnosed as TIA: •Migraine aura •Syncope, postural hypotension •Seizure •Vertigo •Transient Global Amnesia •Anxiety/Hyperventilation •Confusion •Unexplained fall •Peripheral nerve palsy etc. Focal versus non focal symptoms • Localised cerebral ischemia causes focal symptoms. • Non focal symptoms such as faintness , dizziness or generalized weakness are rarely due to focal cerebral ischemia. Focal neurological symptoms • • • • • • Motor: weakness, clumsiness, ataxia* – one side of body. Speech/language: difficulty speaking or expressing, slurred speech*. Sensory symptoms: abnormal feeling. Visual: monocular, binocular, diplopia.* Vestibular: vertigo.* *in isolation not usually stroke. Non focal Neurological symptoms •Generalized weakness and/or sensory disturbance. •Light-headedness •Faintness •Blackouts •Incontinence of urine or feces •Confusion •Tinnitus. Top 6 symptoms likely to be a TIA-1 Sudden onset, lasting minutes to hours, resolves 6. Vertigo only if present with brainstem symtoms 5. Hemibody numbness 4. Double vision, crossed numbness or weakness, slurred speech, ataxia of gait Top 6 symptoms likely to be a TIA - 2 3. Speech disturbance for a defined period of time (definite dysarthria, muteness or marked word finding difficulty, paraphasic speech) 2. Monocular or hemifield visual loss (not blurring of entire visual field) 1. Hemibody weakness Top 7 symptoms unlikely to be a TIA 7. Postural dizziness alone 6. Tingling of all 4 extremities 5. Syncopal events 4. Momentary word finding trouble that is not new 3. Positional and recurrent numbness of one limb 2. Scintillating or flashing visual disturbances Symptoms unlikely to be a TIA - 2 1. Almost anything with hyperventilation or chest pain (but make sure it isn’t cardiac!) Why are these patients important? 90 Day Prognosis after ED Dx of TIA •180 / 1707 (10.5%) patients had stroke – 91 occurred in first 2 days – Age > 60, DM, Sx > 10 min, weakness, speech •428 (25.1%) had some adverse event – More than half occurred in first 4 days Johnston SC, JAMA 2000;284:2901-2906 Independent Risk Factors for Stroke Following TIA • Independent risk factors for stroke following suspected TIA include: – – – – – Age >= 60 years Diabetes mellitus Motor weakness Speech impairment Symptom duration > 10 minutes Johnston et al. JAMA 2000;284:2901-6. ABCD2 Score Derived a 7 point score to stratify the clinical risk of stroke after TIA: •A: age > 60 years – 1 point •B: BP (systolic>140mmHg, diastolic>90 mmHg). Either 1 point. (max 1 point) •C: clinical – unilateral weakness =2, speech only = 1, •D: Duration, >60 minutes =2, 10-59 =1, <10 =0. •D: Diabetes mellitus =1 Johnston, SC, Lancet 2007;369:283-292. ABCD2 Score Predictive Value of the ABCD2 progostic score Prognostic scores for screening: caution advised Highest scores medium scores lowest scores = recurrent stroke Most events actually occur in those of medium risk! So be careful of too high a cutoff. 1 22 How urgently should high risk TIA patients be assessed? Does it make a difference? Express Study ASPIRE TIA Triaging Consensus • Urgent triage and assessment of TIA should be province wide • Access to expertise should not be dependent on geography. • TIA Triaging algorithm created at Aug 2008 meeting • Facilitate urgent access for high risk patients using a TIA Hotline • Backing of the APSS and the Educational Strategy of the APSS Conclusions • Either ABCD2 >=4 OR Speech or motor symptoms can identify high risk symptoms • They have similar sensitivity (88-100%) and specificity (31-52%) to identify high risk stroke patients • ASPIRE Consensus group choose these cutoffs for TIA Triaging within Alberta Hotline process • North - every TIA hotline call will result in contact with a Telestroke Neurologist • South - TIAs will be screened by operator using risk algorithm; • High or if referring physician requests it still - Stroke Neurologist • Low risk and if no specific request - fax referral in to clinic ASPIRE Data • The TIA Hotline and TIA Triaging Strategy overlap with APSS Educational Strategy as well as Pillar 1 - quality improvement • Data will be tracked by TIA Hotlines (SARCC in the south and the CCL/UCL in the north) • Stroke Prevention Clinic referral forms will be faxed to a central number to track all TIAs that come to referral across the province ASPIRE Outcomes • Rate of recurrent stroke determined by presentations to emergency departments and admissions to hospital will be tracked using administrative data • Two years ‘pre’ compared to two years ‘post’ implementation • Is the TIA Hotline/Triaging strategy effective? Is it worth the cost and effort? • Ongoing feedback and refinement TIA Hotline ‘go live’ dates • North including Red Deer (1-888-2824825) • Goes live March 16, 2009 • South excluding Red Deer (1-800-6611700) • Goes live March 16th, 2009 THANK YOU!