in the Emergency Department Acetaminophen and Salicylate
advertisement

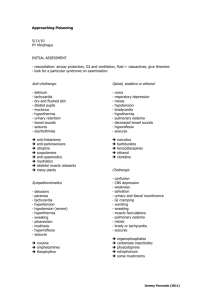
in the Emergency Department Acetaminophen and Salicylate Ingestions Thomas J. Sugarman, MD, FACEP December 2007 Outline • • • • Overview of the poisoned patient Charcoal vs. gastric emptying Acetaminophen ingestions Salicylate ingestions Scope of Problem • 4-5 million poisonings per year – 2 million reported • Death is rare--0.04% of reported poisonings • 60% of poisonings in children < 6 years old – Iron ingestion most common cause of death • 87% of fatalities occur in adults, – Analgesic (salicylate/acetaminophen) and antidepressants most common--50% of deaths Patient Characteristics • • • • • Intentional vs. Unintentional Chronic vs. Acute Adult vs. Pediatric Unclear presentation Toxidromes--characteristic constellation of signs and symptoms History • Time of Ingestion • Quantity • Substance – Over the counter medicines • Hints – Examine pill bottles – Search patient and clothing – Talk to family, friends, witnesses, ambulance personnel Exam • Characteristic odor – Wintergreen--methyl salicylate • • • • • Vital Signs including accurate temperature Mental Status Skin signs Ability to protect airway Pupils Assess for Other Conditions • Suicidal potential • Trauma Tests • Glucose check – Possible salicylate ingestions--especially children – Altered sensorium, including alcohol intoxication • EKG or monitor – Tachycardia or bradycardia – All patients with altered sensorium and possible overdose Tests • • • • • Pulse oximetry Toxicology screen generally not helpful Electrolytes CPK Urine – Crystals – Heme positive may suggest rhabdomyolysis Drug Levels • Acetaminophen – Order as screening exam unless sure not acetaminophen ingestion • Salicylate – Controversial if needed as a screen • Toxicology screen generally not useful – Not sensitive – Slow--does not effect clinical decision making Approach to the Poisoned Patient • • • • • • • Treat the patient, not the toxin Supportive care Prevent absorption Enhance elimination Specific antidotes Consult poison control or Poisindex www.emedicine.com Supportive Care • ABC’s--basic life support • Glucose, thiamine • Prevent aspiration – Left lateral decubitus position – Readily available suction • Treat other conditions – Seizures – Hypoxia – Hypotension – Dysrhythmia Gut Decontamination • Options – – – – – Syrup of ipecac Gastric lavage Charcoal Charcoal + gastric lavage Whole bowel irrigation • Generally charcoal alone is preferred Syrup of Ipecac • Advantages – Given at home – Tastes good so easy to get kids to take – Causes vomiting within 30-60 minutes • Disadvantages – Vomiting with risk of aspiration – May increase absorption in small bowel – Interferes with oral medications • N-acetyl cysteine • Charcoal Syrup of Ipecac • Contraindications – Caustic ingestions, hydrocarbons – Altered mental status or potential for AMS • Coma • Seizures – Infants < 6 months old • Dosage (follow with water) – Adults 30cc – 6 mos-5 years 10cc – 1-5 years 15cc Gastric lavage • Advantages – Can be done in uncooperative patient • Disadvantages – Aspiration – Stomach or esophageal perforation – Risk of complications increases in uncooperative patient Gastric lavage • Left lateral decubitus position with head down to decrease risk of aspiration • Must use large tube 30-40 French in adult – Pills are bigger than small holes in NG tube • Consider intubation • Nothing in literature suggests using lavage to “teach a lesson” – Cruel, dangerous – Unethical without medical indication Charcoal • Advantages – Works immediately – Can be given by small bore NG tube in uncooperative patient • Disadvantages – – – – Aspiration Makes intubation difficult Constipation Interferes with oral drugs except n-acetyl cysteine Charcoal • Dosage – 1 gram/kg (50-100 grams in adult) – 10 grams charcoal/1 mg drug • Use without cathartic–or for first dose only – Magnesium Citrate 4ml/kg (one bottle for adults) – Sorbitol (70%) 1 gram/kg (50-150 ml) – Mag Sulfate (10%) 250 mg/kg (15-30 g) • Use nasal-gastric tube if patient will not drink Charcoal • Charcoal ineffective for – Heavy Metals – Alcohols – Hydrocarbons – Small ions (Li, Fe, K) – Caustics – Solvents • Repeated dose charcoal – Theophylline – Carbamazepine – Tricyclics – Barbiturates – Phenytoin – Aspirin Charcoal vs. Gastric Emptying • Charcoal – Decreased drug absorption – Works in small intestine • Gastric emptying is generally not helpful except – – – – Within first hour in obtunded patients Ingestions with delayed gastric emptying Ingestions that slow motility Massive ingestions Charcoal vs. Gastric Emptying • Kulig 1985--592 patients – Lavage/ipecac + charcoal vs. Charcoal only – Only difference was in obtunded patients seen in first hour – 2 complications • Pond 1995--876 patients – Similar designs – No differences between groups • Conclusion do not empty stomach routinely Charcoal vs. Gastric Emptying • Most of the time charcoal alone is best choice • In asymptomatic, late presenting patients, no decontamination is a reasonable option Whole Bowel Irrigation • Polyethylene glycol by NG/oral until rectal effluent is clear – 25 ml/kg/hour children –1.5-2 l/hr adults • Indications – – – – Drugs not absorbed by charcoal Sustained release or enteric coated pills Aspirin concretions Body packers Acetaminophen • 70 minutes to peak level • 4 hour peak with delayed gastric emptying • Glucuronide and sulfate conjugation to non toxic metabolites • p450 metabolizes it to NAPQI--toxic • NAPQI is metabolized by glutathione dependent reaction • Glutathione depletion toxicity Acetaminophen OD Presentation • Few signs and symptoms early • Stage I: 7-14 hours post ingestion – Anorexia, nausea, vomiting, diaphoresis • Stage II: 24-48 hours post ingestion – Stage I symptoms improve – Right upper quadrant pain, hepatomegaly, elevated transaminases and prothrombin time – Renal damage in up to 25% Acetaminophen OD Presentation • Stage III: 3-5 days post ingestion – Hepatic failure – Death Or • Stage IV: 3-5 days post ingestion – Hepatic regeneration Acetaminophen Range of Toxicity • • • • >150 mg/kg ingested > 7 grams ingested in adult Alcoholics at greater risk Rumack-Matthew nomagram – 4 hour level > 150 ug/ml – Only valid for single acute ingestion – Extended release needs later levels and trends Acetaminophen OD--Antidote • N-acetylcysteine (NAC), Mucomyst – Increases glutathione • 100% effective if given in first 8 hours • Decreasing effectiveness for next 16 hours N-acetyl cysteine dosing • Oral dose – Load 140 mg/kg – Maintenance 70 mg/kg for 17 doses – Do not need to adjust dose for charcoal • Dilute 1:3 if given orally, or use NG – Repeat dose if vomit within 1 hour – Can use anti-emetics – Does not effect acetaminophen levels N-acetylcysteine IV dosing • Acute within 8 hours—21 hour treatment – Load 150 mg/kg over 1 hour (250 ml D5W) – 50 mg/kg over 4 hours (500 ml D5W) – 100 mg/kg over next 16 hours (1 liter D5W) OR • Late or chronic presentation—48 hour – Load 140 mg/kg over 1 hour (500 ml D5W) – 70 mg/kg over 1 hour (250 ml D5W) give 12 doses Acetaminophen Ingestion Approach • 4 hour level on all overdose patients – May be asymptomatic until hepatic damage – Repeat level if below but near toxic range • Use charcoal if early • Start NAC within 8 hours of ingestion or as soon as possible • Continue if in toxic range • Alcoholics at higher risk, treat at lower levels Acetaminophen Ingestion Approach • Supportive care • Consider co-ingestions, extended release capsules, and chronic ingestion • Caution with: – Pregnant patients consider IV NAC – Chronic ingestion or extended release – Alcoholics Salicylate Toxicity Sources of Salicylate • Aspirin • Oil of Wintergreen (methyl salicylate) – 1 teaspoon can be fatal for a child • Over the counter preparations • Topical preparations Salicylate Physiology • Rapidly absorbed from stomach – Peak levels in 2-4 hours – Enteric has delayed absorption • Concretions may form in overdose – Concretions cause delayed absorption • Renal excretion • In overdoses, excretion slows with 1/2 life up to 15-30 hours Salicylate Physiology Acid-Base Disturbances • HyperventilationRespiratory Alkalosis – Respiratory acidosis may develop late if severe • Oxidative phosphorylation becomes uncoupledMetabolic Acidosis • Young children tend to have metabolic acidosis • Adults tend to have respiratory alkalosis Salicylate Physiology • Salicylate is highly protein bound – Decreased protein binding if acidotic • Hypoglycemia, especially in children • Hypokalemia very common – K+ from early alkalosis • Cerebral and/or Pulmonary Edema – Increased capillary permeability Salicylate OD Presentation Mild • Tinnitus • Hearing disturbance • Mild hyperventilation Moderate • • • • • • Severe hyperventilation Lethargy Nausea/vomiting Anion gap acidosis Dehydration Hypokalemia Salicylate OD Presentation Severe • • • • Hypoglycemia Hyperthermia Pulmonary Edema Severe metabolic acidosis • • • • • Cerebral Edema Coma Seizures GI bleeding Platelet dysfunction Acute Salicylate Range of Toxicity Based on Ingested Amount • < 150 mg/kg • 150 mg/kg mild to moderate • 300-500 mg/kg serious • Above true for single acute ingestion • More serious in elderly and young children Laboratory Evaluation • Ferric Chloride test – 1cc urine + few drops 10% ferric chloride – brown-purple color indicates salicylate • Anion Gap Acidosis • Mixed Respiratory Alkalosis/Metabolic Acidosis • Hypokalemia/Hypoglycemia Salicylate Levels • < 30 mg/dltherapeutic, non toxic • 30-100 mg/dltoxic • >100 mg/dl very severe • Should be checked 4-6 hours post ingestion • Beware of increasing levels from delayed absorption Salicylate Levels • Done Nomagram – – – – – Single acute ingestion Not for enteric aspirin Assumes no concretions Assumes normal renal function Developed for and with Pediatric patients • Limited utility – Make treatment decisions based on other clinical factors GI Decontamination • Repeated Dose Charcoal • Consider lavage if early--remember need big tube • Whole bowel irrigation Hypoglycemia • Check glucose • IV fluid should have glucose Fluid Therapy • • • • Correct dehydration Aim for urine output 2-3 cc/kg/hours Correct hypokalemia Avoid over hydration because of risk of cerebral and pulmonary edema • No forced diuresis Urinary Alkalinization • • • • • Helps excretion Load 1-2 meq/kg Bicarb 1-2 meq/kg Bicarb every 1-2 hours Urine pH 7.5-8.0 Do not cause systemic alkalosis-aim for serum pH ~7.5 • Must correct hypokalemia Dialysis Indications • Renal Failure • Congestive heart failure or pulmonary edema • Unresponsive to other therapy • Levels > 100-120 mg/dl may require dialysis Chronic Ingestions • Common in elderly • 25% mortality • Consider with non cardiogenic pulmonary edema • Done Nomagram irrelevant • Lower threshold for dialysis – Levels > 60 mg/dl Disposition • Medical clearance--non symptomatic, non toxic level 4-6 hours post ingestion – If borderline level consider repeating to rule out delayed absorption • Admit all others to medical bed • Early transfer if dialysis is unavailable and may be required Salicylate Pitfalls • Failure to consider in differential diagnosis – Gap acidosis – AMS in elderly • Topical preparations in children can cause serious toxicity • Failure to be alert for delayed absorption • Beware of hypoglycemia especially in children