Urinary System
advertisement
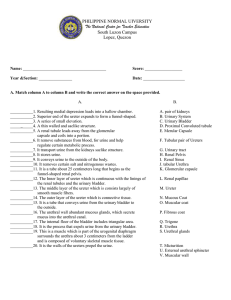
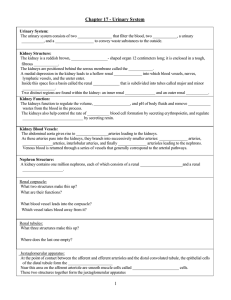
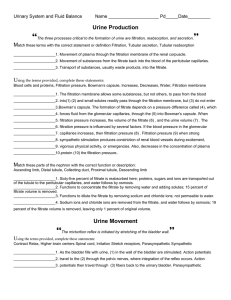
Urinary System By: Blake Rossman, David Barin, & Gabe Watkins Functions of the Urinary System The urinary system removes certain salts and nitrogenous wastes. Helps maintain water and electrolyte concentrations Regulate certain metabolic processes by having Tubular ureters Saclike urinary bladder Tubular urethra Functions and Locations of the Kidney Kidneys Reddish-brown, bean-shaped organ with a smooth surface Lie on either side of the vertebral column Positioned retroperitoneally Behind the parietal peritoneum and deep muscles in the back Connective tissue and masses of adipose tissue surround the kidneys Functions and Locations of the Kidney Functions and Locations of the Kidney Primary role is to maintain homeostasis. Regulates the composition, volume and pH of the extracellular fluid. Other important functions Secrete erythropoietin Have a role in the activation of vitaminD Secrete enzyme renin Functions and Locations Renal Blood Vessels Renal Arteries Basic blood supply to the kidneys Arise from the aorta Functions and Locations of Nephrons Kidney has about 1 million nephrons. Each nephron consists of a renal corpuscle Renal tubule Renal Corpuscle is made of glomerulus Help filter fluids, the first step in urine formation Renal Tubule Fluid flows through on its way out of the body Functions and Locations of Nephrons Urine Formation Glomerular filtration Filtration of plasma by the Glomerular capillaries Filtered fluid is reabsorbed in the bloodstream Colloid osmotic pressure of the plasma Tubular reabsorption Moves substances from the tubular fluid back to the blood Tubular secretion The reverse process, moves substances from the blood within the peritubular capillary into the renal tubule Urine Formation Continued Amount filtered at the glomerulus -Amount reabsorbed by the tubule + Amount secreted by the tubule = Amount excreted in the urine Urine Formation Urine Formation Glomerular Filtration Similar to filtration at the arteriolar ends of other capillaries. Mostly water and the same components as blood plasma Filtration Pressure Hydrostatic pressure of blood forces substances through the glomerular capillary wall Net filtration pressure is the net pressure forcing substances out of the glomerulus Normally positive Favoring filtration at the glomerulus Urine elimination Urine forms in the Nephrons >Passes through collecting ducts in renal papillae > calyces of kidneys > renal pelvis > ureter conveys it to the urinary bladder > urethra excretes urine Functions and Locations of Major Organs Ureters Help for urine elimination About a 25cm tube that extends downward behind the parietal peritoneum and runs parallel to the vertebral column. There are 3 layers. The inner (mucous coat), middle layer (muscular coat), and outer layer (fibrous coat) The muscular walls of the ureters propel the urine Functions and Locations of Major Organs Urinary Bladder Stores urine and forces it into the urethra It is within the pelvic cavity, behind the symphysis pubis and beneath the parietal peritoneum The internal floor of the bladder includes a triangular are called the trigone Posteriorly at the base of the trigone, the openings are of the ureters. Has 4 layers which are mucous coat, sub-mucous coat, muscular coat, & serous coat. Can hold as much as 600 milliliters of urine before stimulating pain receptors Urinary Bladder Micturition Micturition is urination or the process that expels urine from the urinary bladder Detrusor, abdominal wall and pelvic floor muscles contract Stretch receptors stimulates triggering the micturition reflex Distension of the bladder wall as it fills with urine Micturition reflex center is in the spinal cord External sphincter is composed of skeletal muscle Under Conscious control Diseases Cystitis- Inflammation of the urinary bladder More common in women because urethral pathway is shorter; Ureteritis- Inflammation of the ureter Glomerulonephritis- the glomerular capillaries are inflamed and become more permeable to proteins Automatic bladder- damage to the spinal cord above the sacral region destroys voluntary control of urination Thank You