staph ppt 1

Staphylococcus
Kenneth L. Muldrew, MD, MPH
Assistant Professor
Department of Pathology
Medical Director
Clinical Microbiology Laboratory
Molecular Diagnostics Laboratory kenneth.muldrew@utoledo.edu
Office: 383-6444
Staphylococcus
Objectives:
1) Recognize the epidemiology of staphylococcus
2) Describe the pathogenesis, clinical presentation, diagnosis, & treatment of common staphylococcal clinical illnesses
3) Describe the basic microbiology of staphylococcus a) enzymes/toxins b) cell structure c) host defenses d) lab identification
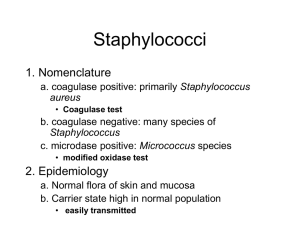
Staphylococci -General
• Two groups: Coagulase negative Staphylococci
(CoNS) & Coagulase positive Staphylococci (CPS)
• Extremely important genus of bacteria that include the dreaded Staphylococcus aureus (S. aureus) and the common less virulent Staphylococcus
epidermidis (S. epidermidis)
• Resistance to methicillin is a worsening problem
(MRSA)
Staphylococci - General
• Members of the family Micrococcaceae
• Gram - positive cocci that produce catalase
• Facultative anaerobes
• CoNS: most are non-hemolytic (γ-hemolysis)
• CPS: β-hemolysis
• Arranged in clusters, look like grapes- due to irregular and incomplete division of daughter cells (Staphyle is Greek for
“bunch of grapes”)
• Clustering is usually seen when gram-stain is performed from an agar colony
• can see clusters, single, paired or chained cocci when gramstain is performed from an agar colony
gram stain-colony
gram stain-pus
Staphylococci - General
• Relatively hardy organisms (not fastidious) and will withstand heat, drying, higher salt concentrations
• Grow readily under aerobic and anaerobic conditions
• Produce catalase (an enzyme that converts
H
2
O
2 into H
2
O and O
2
) this enzyme differentiates them from streptococci
Staphylococci - General
• Medium sized bacteria - @ 1 um/cocci
• agar plates- colonies appear smooth, white or yellow and ± beta hemolysis
• Age of bacteria, phase of growth, culture media can all change the characteristic appearance
• Nonmotile, non-spore forming
• Some strains can also be encapsulated
Staphylococci - General
• Approximately 32 species of Staph - 16 are associated with humans - 4 are important
– S. aureus
– S. epidermidis
– S. saprophyticus
– S. lugdunensis (more virulent than other CoNS; severe endocarditis)
• Other staphylococcus species in humans
– S. capitis, S. warneri, S. hominis, S. haemolyticus, S. caprae, S. pasteuri, S. xylosus, S. cohnii, S. simulans,
S. auricularis, S. schleiferi, S. saccharolyticus
Staphylococci - General
• Staph species are subdivided by their ability to produce coagulase (2 enzymes that bind to prothrombin which results in the conversion of fibrinogen to fibrin) into two major groups
– S aureus produce coagulase (Coagulase Positive
Staphylococci or CPS)
– Most other Staphylococci do not (Coagulase
Negative Staphylococci or CoNS)
Staphylococcus aureus
Staphylococcus aureus
• CPS/Major human pathogen
• Name (aureus) comes from appearance on agar plates (Au- golden grapes)
– yellow coloration comes from production of carotenoids (class of pigments that include the precursors to vitamin A)
– Non-pigmented experimental strains are easier for neutrophils to kill and less likely to form abscesses
– colony morphology affected by many variables
– Beta hemolytic
S. aureus
S. epidermidis
S. aureus: Beta hemolytic
Staphylococcus aureus
• Virulence is controlled by agr (accessory gene regulator)
– AgrA to AgrD and other regulatory systems
• Positive and negative controls on this system by other multi-component gene regulatory systems
• Important cell wall components
– peptidoglycan (common to all GP organisms)
– teichoic acid (common to most GP organisms)
– protein A (most strains of S. aureus)
Peptidoglycan
• Complex polymer - thick layer is found in GP organisms and gives
Gram’s stain characteristics
– backbone of alternating subunits of Nacetylglucosamine and Nacetylmuramic acid
– side chains are linked to muramic acid residues and cross-linked by a glycine bridge
– peptidoglycan confers structure and stability
– target for B-lactam and glycopeptide antibiotics
Peptidoglycan
• Backbone is not species specific
• side chains are species specific
• Causes immune response
– IL-1 production from monocytes
– attracts PMNs
– activates complement
– elicits antibody response
– has some endotoxin-like activity
Teichoic acid
• Phosphate containing polymers
• Two types
– one type linked to cell membrane and one type with ribitol and phosphate linked to the cell wall
• Constitute major surface antigens
• Function in pathogenesis?
Protein A
• 42,000 dalton protein found in most, but not all, strains of S aureus
• Binds to the Fc terminus of the IgG molecules
(except IgG
3
)
• ? Superantigen
• Immunologic tool (eg- monoclonal antibody purification)
Epidemiology
• Colonization with S. aureus begins at birth
– from humans and surrounding fomites
– skin, perineal area, umbilical stump, occasionally
GI tract
• Children and adults colonized in anterior nares
– 30% chronically colonized, 50% intermittently colonized, 20% never colonized
• 1.5% colonized with MRSA
Epidemiology
• Vaginal carriage of S. aureus occurs in 10% of women
• Hospital personnel have high rates of colonization (50%-90%) - reason why unclear
– also, patients with DM, ESRD, IVDA, chronic skin conditions have increased rates of carriage
Epidemiology
• CA – MRSA – community acquired MRSA
– Strain(s) of S. aureus which carry resistance to methicillin and often carry the Panton-Valentine leukocidin (PVL) toxin
• Association of this toxin in CA-MRSA with skin and soft tissue infections and severe necrotizing pneumonia with sepsis
• Prospective study in 2004 of patients with staph infections (infections NOT colonization) found that 59% were CA-MRSA, 98% of those had PVL
Epidemiology
• Risk factors for CA-MRSA
– Skin trauma (eg, "turf burns", lacerations or abrasions)
– Lineman or linebacker position in football
– A higher body mass index
– Cosmetic body shaving
– Physical contact with a person who has a draining lesion or is a carrier of MRSA
– Sharing equipment that is not cleaned or laundered between users
– Prison residence
– Military personnel
– Prior skin infection
– Previous antibiotic use
– Illicit drug use
– Tattoo recipients
Clinical Case 1
A 30-year-old woman was transferred to the hospital with hypotension and respiratory failure. She was well until 4 days before admission, when she slipped and fell and at that time had severe posterior thoracic pain that radiated to the anterior chest and lower back which did not respond to acetaminophen. Physical examination was normal except for tender paraspinal muscles. Radiographs of the chest and thoracic spine were normal, and she was given Ketorlac and sent home. The following day, she went to another hospital because of persistent pain, and was again sent home, this time with oxycodone for pain.
One month prior to admission, she was treated for a small right leg abscess due to methicillin resistant Staphylococcus aureus that was susceptible to clindamycin, vancomycin, tetracycline, and trimethoprim–sulfamethoxazole. On the day of admission to the hospital, a friend found her at home, unresponsive and moaning.
She was agitated and aphasic, but responded to painful stimuli.
Clinical Case 1
•
•
•
•
•
Physical Exam:
Rectal temperature 39.6°C, bp 113/53 mm Hg, pulse 156 bpm, RR 46 , O
2
Sat= 83%
Obtunded, minimally reactive pupils
Skin gray, warm, and clammy, with papular and pustular rash on the face, neck, chest, and abdomen
1 cm healing ulcer on right leg rales in both lungs on inspiration and expiration heart exam was normal
Clinical Case 1
• Labs:
– Hg: 10.6 g/dl (normal=12-16)
– HCT: 31.3% (Normal=36-46)
– WBC 1,500 cells/uL (normal=4,500-11,000)
• Differential: 14% Neutrophils, 3% bands, 72% lymphs, 2% Eosinophils, 9% metamyelocytes
– Plt: 59,000 (normal 150,000-450,000)
– D-dimer: 6,895 ng/ml (normal <500)
– Prothrombin time and APTT elevated
– ABG acidotic
– Renal failure (creatinine 4.84 mg/dl; normal=0.6-1.5)
– Elevated liver enzymes (LDH, AST, ALT) and elevated CK (muscle)
– Urine: blood, protein, increased WBC
Clinical Case 1
Intraparenchymal hemorrhage, edema
Clinical Case 1
• treated with: Ceftriaxone, clindamycin, meropenem, gentamicin, bactrim, doxycycline
• Blood pressure markedly decreased
(73/40 mm Hg), and she required significant fluids and pressors.
She further deteriorated, went into shock, disseminated intravascular coagulation, and died the next day.
• Blood cultures turned positive after death
• Catalase positive
• Coagulase positive
Pulsed Field Gel Electrophoresis (PFGE)
• Based on digestion of high MW DNA with a rare cutting restriction endonuclease (SmaI)
• Electrophoresis using a system of alternating current angles
Normal Gel ≈ 2 hrs
0.050-25 kilobase-pairs
--
PFGE≈ 18 hrs
25-700 kilobase-pairs
+ + + +
++ - - - - -
Pathophysiology
• In order for disease to occur, adherence of organism to host with invasion and bypassing of defenses must occur
– S. aureus is in anterior nares of adults in varying degrees and is found on fomites, occasionally aerosol spread
– several properties of S. aureus increase its ability to adhere to skin/mucous membranes after contact
Adherence
• Three types of adherence
– to mucosal cells/nasal epithelial cells
• teichoic acid (phosphate polymer on cell wall) allows adherence to mucosal cells
– to traumatized or broken skin
• fibrinogen, fibronectin, laminin, thrombospondin, collagen
– to endothelial surfaces
• fibronectin, laminin
Invasion
– initial steps of invasion of host after colonization are incompletely understood
– after bacteremia, S. aureus can invade tissues, binding to thrombin, fibrin, or endothelial cells
• adherent S. aureus is then phagocytized by endothelial cells, macrophages
– Staph then release proteolytic enzymes
– host response activated with macrophage activation, TNF, IL-1, IL-6, IL-8 release
– abscess formation
Toxins and Enzymes
• Severity of disease depends on:
– inoculum size, host immunity, and virulence
• S. aureus secretes enzymes and toxins:
– catalase, coagulase, hyaluronidase, Blactamase, leukocidins, tsst-1 toxin, fibrinolysin, Panton-Valentine leukocidin toxin
Toxins and Enzymes
• H
2
O
2
CATALASE H
2
O + ½O
2
– PMNs use hydrogen peroxide/free oxygen radicals to kill staph
– enzyme production is also used to differentiate staph (+) from strep (-)
Staph
Catalase Test
Strep
Toxins and Enzymes
• Coagulase
– 2 enzymes: (97% of all SA isolates have both)
• Bacterial cell-associated (bound coagulase)
• Extracellular or free coagulase
– converts fibrinogen to fibrin
– activation of the clotting cascade occurs with sepsis
– Fibrin bound to organism prevents phagocytosis
Tube Coagulase:
-rabbit plasma & organism
-free and bound coagulase
-read at 2 hours
-if negative read at 18 hours
Rapid Test: Staphaurex (Latex agglutination): Read at 2 minutes
•
S. aureus bound coagulase binds fibrinogen that is bound to latex beads
•
S. aureus Protein A binds Fc receptor on rabbit IgG that is bound to latex beads
•
Latex beads and S. aureus clump together
Bound Coagulase
Fibrinogen
• Staphaurex
Rabbit IgG
Protein A
Rapid Test Staphaurex (Latex agglutination): Read at 2 minutes
Positive Negative
Toxins and Enzymes
• Hemolysins - proteins which lyse red cells and other cell types
– Panton-Valentin toxin encoded by a mobile phage and regulated by
agr system
• Can transfer easily to other strains
• Not associated with osteomyelitis, endocarditis
• Leukocidin - binds phagocytes and creates pores in membrane
• Hyaluronidase - hydrolyzes hyaluronic acid in connective tissue; May allow spread of staph in tissues
• Fibrinolysin - dissolves fibrin clots
Toxins and Enzymes
• B-lactamases - confer antibiotic resistance
• Exfoliatins - two serine proteases that bind to desmosomes and cause SSSS (staph scalded skin syndrome)
• Cytotoxins - alpha, beta, delta, gamma
– cytolytic activity for a variety of cell types such as smooth muscle cells, sphingomyelin, and erythrocytes
Toxins and Enzymes
• Superantigens:
• Toxic shock syndrome toxin
(TSST-1)
• staph enterotoxins
A- E (SEA-SEE)
Host Defects
• Phagocytosis - major defense
– PMNs and Monocytes/macrophages
• Host defects which predispose to S. aureus
– Chemotaxis defects
• Job’s syndrome
• Chediak-Higashi syndrome
Wiscott-Aldrich syndrome
– PMN killing defects
• chronic granulomatous disease:
– no respiratory burst in phagocytosis (x-linked)
– prone to Staph infections
– life-long antibiotics needed