Nursing Case Management - Clinical Practicum Scholarly Paper
advertisement
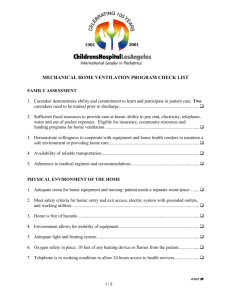
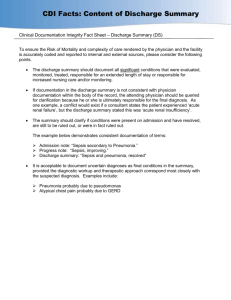
Nursing Case Management Advanced Role for the Professional Nurse “I reckon being ill as one of the great pleasures of life, provided one is not too ill and is not obliged to work till one is better”. ~Samuel Butler, The Way of All Flesh, 1903 Lecture Content • Introduction to Case Management Concepts • Basic Concepts in Case Management Episodic Care Tertiary and Long Term Care Continuum of Care Primary Care, Prevention and Disease Management • The Case Management Process Comparison for Similarities with The Nursing Process Lecture Content page 2 • The Case Management Process Phase 1: Case Screening and Selection Phase 2: Assessment Phase 3: Development and Coordination of Treatment and Discharge Planning Phase 4: Outcomes Case Management-Continuously monitoring, reassessing and revising the plan. Phase 5: Executing the Discharge Plan Phase 6: Outcomes Management: Were the goals achieved? Lecture Content Conclusion page 3 • Resources for Case Managers Development of Resource Manual Internet Resources Certification Degree Programs Introduction to Case Management Concepts • The challenge of condensing a master degree program into a single slide presentation has been overwhelming, but necessary. Health care providers who can rise to meet the needs of the patient, provide quality driven care and remain fiscally responsible to the health care industry will be our most valuable health care resource as more baby boomers past the golden age of sixty-five. Case management is not a new concept. Lillian Wald, as a public health nurse provided home services and case finding in the 1900s. Social workers and psychiatric nurses also provide early continuum of care principles as they followed their patients after discharge to facilitate long-term community-based care (Cresia & Parker, 2001). As the demand for the role increased, the need to formalize a description of a case manager challenged nursing and health care leaders. Although several very comprehensive definitions exist, perhaps the most concise was put forth by the Case Management Society of America (CMSA). “ Case management is a collaborative process which assess, plans, implements, coordinates, monitors, evaluates options and services to meet an individual’s health needs through communication and available resources to promote quality cost-effective outcomes”. (1995) Who Can Be a Case Manager? Sounds a lot like the nursing process doesn’t it? Many of the first case manager’s however were social workers who had extensive understanding of the community-based resources available. Who would be a case manager was largely driven by the organization’s focus of needed services. If an organization was focused only on getting the patient discharged, social workers were heavily utilized. When organizations placed a stronger emphasis on outcomes management (controlling the entire process), they hired nurses, generally BSN or MSN prepared. Many of the certification and fellowship organization’s today still recognized professions other than nursing among their ranks. http://www.aihcp.org/ You will find that in long-term care facilities, Physical Therapists and Respiratory Therapists are utilized and often certified as case managers because of the focus of service. Although we recognize and acknowledge that other disciplines perform the role of case managers, for the remainder of this lecture, we will assume the role is being performed by a nurse. During the next week, check out your organization. Do you have case managers? What is their job description? Are they nurses, social worker’s or other licensed professionals? Are the case manager’s at your organization required to be certified? What is the minimum academic degree that your organization requires for you to be employed as a case manager? Role and Job Responsibility The job roles and responsibilities can be diverse for the nurse case manager and she or he must be able to wear many hats. By law, as nurses, we are required to advocate for our Patients. This advocacy role also holds true when we work as case managers. As case managers, we act as an interface for the patient between the organization, insurance companies and sometimes even the family. In creating and implementing the individual plan of care, we may utilize many resources to help effect the desired outcome. On the next slide, I provide a list of just some of the departments, facilities, programs, services and interdisciplinary team members that you will utilize a resources to achieve your outcomes and empower the patient and family to maintain wellness. This List is intended to be representative, not all encompassing. The resources you would utilize will be unique to your patient population, geographic location, Socioeconomic base, practice loci and organizational directives. Case Management Wheel Inpatient Diagnostics Hemodialysis Acute Care Nurses Home Health Care Doctors Diab Nurse Educ Pulmonary Rehab Nurse Case Manager/ Patient-Family Social Services Community and Hosp Educators Other Case Managers Hospice OT/PT/Speech Inpatient Rehab Pharmacy Durable Medical Equip Case Management Wheel Inpatient Diagnostics Acute Care Nurses Hemodialysis Home Health Care Doctors Diab Nurse Educ Pulmonary Rehab Nurse Case Manager/ Patient-Family Social Services Community and Hosp Educators Hospice Other Case Managers Inpatient Rehab OT/PT/Speech Pharmacy Durable Medical Equip 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Inpatient Diagnostics Acute Care Nurses Doctors (Multidisciplinary Pulmonary Rehab Community and Hospital Educators Other Case Managers OT/PT/Speech Therapies Durable Medical Equipment (DME) Pharmacy Inpatient Rehab Outpatient Rehab Substance Abuse Rehab Hospice Social Services Diabetic Educator Nurse Home Health Care Hemodialysis Unit Following the case management process, very similar to the nursing process, the case manager determines which resources he will utilize to facilitate the patient’s course through episodic or continuum of care needs. The decisions the case manager makes will have a direct impact on the length of hospital stay for the patient. *A delay in identifying the correct needs and the patient ends up with a longer length of stay (LOS). A longer hospital stay increases the patients risk for acquiring a nosocomial infection and that risk goes up as the acuity of service goes up. (the area of highest risk then is ICU, MICU, CICU, PICU, etc…) also increasing morbidity and mortality. *An incomplete or not well designed discharge plan because the initial assessment was incomplete, and the patient is readmitted to the hospital for failed home plan. This can include failure to arrange for DME, home care services, home meds such as IV meds, home O2, adequate personal assistance at home, safe home environment. *Failure to include the patient in the plan every step of the way will usually get you a plan that falls flat on its face the day of discharge. If the patient-family is not in agreement, then you don’t have a plan. *You always have to be willing to think outside of the box. *You sometimes are wrong. What follows is an experience a colleague had with a very complicated case. She is the consummate professional, but it is an example that even when you cover all of your tracks and are as thorough as possible,. you can still miss important things. Ms. X had had a very long and complicated hospital course after abdominal surgery. After weeks on a vent, peritonitis, multiple parachute dressing changes, sepsis, cardiac arrest, she finally was a few days from going home. Her devoted husband, always near Her side, was excited about having her home and assured everyone at the hospital That all was ready for his wife’s homecoming. The case manager had made provisions For home care, home IV antibiotics, PT/OT and Meals-On-Wheels. The day before discharge, the local paper ran an article on the shameful degree of poverty with the elderly in the community. Right there on the front page was her patient’s home, complete with no running water, no electricity or sewer hook-up and missing windows, and boards on the front porch. The home looked like it was waiting for the wrecking ball. How could she have possibly thought about sending the patient home to that? But she didn’t know! The patient and husband presented their home just as you or I would and, they finally admitted they were simply too ashamed to admit to the conditions they were living in. The challenges and rewards of being a case management are great for whoever decides to take them on. Whether you are a nurse, social worker or physical therapist, your ability to provide a comprehensive assessment and a holistic plan will determine the success of your patient outcomes. The fiscal challenge of keeping our aging health care administration system afloat with our aging population becomes a challenge for each of us. The winners will be those providers and patients who can collaboratively work to manage health. Individual health is closely linked to community health – the health of the community in which people live, work, and play. Likewise, community health is profoundly affected by the collective beliefs, attitudes, and behaviors of everyone who lives in the community. --- Healthy People 2010: Understanding and Improving Health Basic Concepts in Case Management • When talking about managing care through a case management model, generally we are referring to managing the patient’s utilization of health care resources either through single “episodes” of illness or managing the patient’s health across the “continuum of care”. Continuum of care management can also be used to manage patients with chronic disease states such as CHF, COPD and DIABETES or long term extended care facility requirements. Episodic Case Management • Episodic case management refers to managing a single episode of illness with a patient. Episodic case management is great for the individual who is involved in a minor accident requiring hospitalization, a single episode of pneumonia in a non-smoker, cholecystectomy requiring a drain and home care. For patient’s who are likely to require recurrent hospitalization, or who suffer from a chronic disease state, a case manager can become a coach to guide the patient through states of wellness/illness across time. Thus the patient/case manager team form an integrated unit that are striving toward the same goals. The patient maintains continuity with the same case manager and the case manager is able to manage more cases because she is not constantly building a “new wheel”. Episodic Case Management • Episodic case management generally will occur in an acute or tertiary care setting. • It may occur in an urgent care setting if coordination of community services are required before the patient is discharged home. • Unfortunately, many patients with chronic disease states are case managed under the episodic style. They lose continuity with a single case manager, care is fragmented, long term goals are difficult to set and almost impossible to achieve and there is a loss of coordination of services. Rather than rely on the case manager to assist with needs, the patient comes to the hospital for coordination of home needs and services. What you end up creating is a cycle that never really allows the patient to move forward, frustrating the patient, physician, providers and the insurance company. Continuum of Care • Provides for the management of health across a continuum. I should clarify, the entire health care system, as we currently know it, is based on the management of disease. Health care of the future will be based on the management of health and disease states will be considered poor outcomes. Providers who command the concepts of case management now will be ahead of the proverbial curve and be in a position to provide the best coordination of services to their patient population. Apply the Principles • Consider the following scenario: • Mr M is a 67year old white male with coronary artery disease. He was recently hospitalized for the first time with CHF. Under episodic case management, his case manager arranged for a home care nurse to visit and the insurance company agreed to provide 3 home visits since this was a first time diagnosis for CHF. Although the floor initiated his teaching, the dietician did not see him before discharge (3 day LOS) and his teaching was incomplete. Home care continued to build on what the hospital started, but the insurance company would not authorize more than 3 visits, so the teaching stopped with the last visit. Mr. M. was interested in learning about his disease and was a willing student, but became angry because his services were cut off before he completed his “training”. He was unable to start the cardiac rehab group until he had his follow-up visit with the cardiologist in 3 weeks. Frustrated, he threw his books and handouts in the cupboard and decided he’d had enough. Two weeks later he ended up back in the ER in acute CHF, not knowing how it could have happened. • Let’s consider the same scenario under a continuum of care case management style. Mr. M presented to the ER with his first episode of CHF. He met his nurse case manager, Josh, and Josh described a program that would team them up and help him learn about his disease. His case manager told him about signs and symptoms to watch for, initiated an intake assessment, and assured him he would follow-up with him in the morning. After meeting with Mr. M, Josh placed a call to the reviewer at the insurance company. Josh relayed that Mr. M. was admitted with his first episode of CHF. He also included that Mr. M. was recently widowed, was suffering from depression/grief adjustment and his only child lived in South America. Anticipating that Mr. M. would need an extended support system, Josh negotiated for vigilance monitoring with the home care service. A scale/BP monitor and EKG monitor would be placed in the home on the initial visit when Mr. M. would be taught how to use it. A video would be supplied, as well as a hotline number available 24/7 for any questions he might have. Social services were consulted to see Mr. M. during his inpatient stay, and Josh contacted the dietician directly to discuss Mr. M. and assure that he would be seen before discharge. The next morning, Josh stopped in to see Mr. M on his morning rounds. Mr. M was feeling better and had a lot of questions about CHF. Recognizing a teachable moment, Josh took the opportunity to educate Mr. M about CHF and, recognizing when his interest began to wan, asked a few more intake questions. Josh shared his ideas about the discharge plan and acknowledged that he recognized the symptoms of depression in Mr. M. “It must be very difficult adjustment for you”. “I know this will be a hard time for you to learn new information about your disease, but you and I will be working together on this”. Josh described the case management program he worked in and that Mr. M would be his patient into the future. “You can call me and leave me a message anytime, I will follow-up with you and we will figure out what needs to be done”. Mr. M left the hospital on the 3rd hospital day, feeling encouraged that he really had a solid support system in place to help him out. The cardiologist visit was scheduled for 2 weeks after discharge and the initial appointment to start cardiac rehab was set up for the day after the office visit. Josh planned to follow-up monthly with Mr. M to see how he was managing his disease. When Mr. M was hospitalized 3 months later with a cholecystitis, Josh was there to coordinate his care and monitor his CHF. The Case Management Process • Just as the nursing process is designed to follow a sequence of steps, the case management process follows a logical sequence of steps from case selection through Outcomes Management. The Phases will be reviewed and consideration will be given to critical pathways, care maps and algorithms. Phase 1 • Case Selection Shortages are evident in all aspects of health care. Universal case management is not necessary. Cases are selected on high cost (> $50,000) and high risk (LOS greater than 5 days). These are arbitrary numbers and each institute will determine there guidelines for inclusion into the case selection process. Other considerations: complex medical problems, multiple comorbidities, complex discharge needs or complex social issues, lives alone, older than 65 years, Medicare, Medicaid or uninsured, readmission within 15 days of discharge, type of admission (multi-system trauma for example) and diagnostic related group (DRG). Mental and behavioral triggers • In addition to the previous list, here are a list of mental illnesses, behavioral and substance abuse problems that warrant evaluation. Intentional or unintentional overdose, eating disorders, alcohol or drug abuse, chronic mental illness, Alzheimer’s dementia, medication noncompliance, Munchausen syndrome or Munchausen syndrome by proxy. * Munchausen syndrome (and by proxy) is a mental illness where people, usually women or mothers, produce symptoms of illness to assume the sick role. In children, mother’s make their children ill so they receive attention as a secondary gain, or recognition for what great care they provide. Socioeconomic Indicators • Homelessness, poor living environment, no known social or family support, admission from and extended care facility (ECF) or shelter, single parent, someone who is dependent of ADLs, repeated admissions to acute care, frequent visits to the emergency room and disruptive or obstructive behavior by a family member or significant other. Phase 2 • Assessment/Problem Identification • An in-depth assessment performed on admission will save valuable time later on and identify the correct resources for the correct patient. I have provided a comprehensive list, but again you would adapt this list to reflect this needs specific to the population you serve. Elements of Phase 2 • • • • • • • • Patient History and Demographics Current Medical Status Nutritional Assessment Medication Assessment Financial Assessment Psychosocial Assessment Cultural and Religious Diversity Functional Assessment Environmental Factors Patient History and Demographics • Age, race, marital status, family physician, contact names and numbers, Durable Power of Attorney, ethnic group, languages spoken, religion, children and ages, employment and family responsibilities at home (caregiver for elderly parent). • Disease, accidents, injuries, surgeries, hospitalizations, obstetric procedures and mental illness. • Complicating factors • Noncompliance issues • Medications and therapies, including CAPPs Current Medical Status • Determine health goals and health concerns. • Based on the setting where you are seeing the patients, determine if there are drains, tubes, wound vacs, PICC lines. • Current diet. • Bowel and bladder continence. • Skin conditions, especially potential areas for decubitus ulcers. • Assess the patients understanding of his/her current medical status. Nutritional Assessment • Inadequate or inappropriate food intake. • Financial issues. (I met a patient once, who, after paying her rent had $18 left per month for food). • Social Isolation • Dental/mouth assessment • Ability and disability • Weight loss or gain • Acute and chronic disease states Medication Assessment • • • • • • • • • • • • • • Review all allergies Assess if the patient is taking the meds as prescribed. Assess transportation to pick up meds. Assess insurance coverage for medication. Assess for adverse reactions. Assess for adverse reaction to common foods. Assess and arrange for lab monitoring if applicable. Is the medication dosing regimen as simple as possible? Is the medication dosage at the lowest possible therapeutic dose? Are the medication containers accessible? Does the patient know the names and purposes for his medications? Does the patient know the adverse reactions that he needs to notify the doctor of ? Does the patient know the correct route to take the medication? Review for polypharmacy Multiple meds, from multiple doctors from multiple pharmacies. Financial Assessment • Does the patient have adequate, inadequate or no health insurance? • Is the patient eligible for social security disability, social security income, Medicare, Medicaid? • Can the patient afford his copays? • Can the patient meet his basic financial obligations? • If the patient must go home with high-tech equipment, can he afford the increase utility expense? Psychosocial Assessment • • • • • • • • • Who lives with the patient? Who does the patient identify as her support system? What hobbies or activities does the patient engage in daily? Is the patient homebound? Has the patient experienced a recent trauma or loss? Is the patient cognitively impaired? Are the caregivers at home burned out? How functional was the patient prior to this admission? Is the patient living in temporary housing, such as a motel or hotel? Cultural and Religious Diversity • Assess for meaning of gestures, body posture, eye contact • Respect for cultural traditions • Religious and spiritual beliefs affecting care • Cultural and religious conflicts within the individual and between family members. • Unique dietary considerations. • Special considerations for the daily care routine. • Language barriers – Use of AT&T language line or other translator services Functional Assessment • ADL Assessment • The home environment – – – – – – – Self-care Sanitation Electricity Running Water Safe Stairs Working Telephone Basic equipment and furniture needs are met. Phase 3 • During Phase 3, the case manager develops the plan of care. There is a coordination of acute treatment plans and the discharge planning process begins to take shape. Many institutions utilize critical pathways, care maps or treatment algorithms to keep all the “stakeholders” or team players on the same page. Let’s talk about the use of critical pathways. Critical Pathways • In the 1980’s and 1990’s critical pathways or care maps gained widespread favor in acute care settings. The use of diagnosis specific pathways allowed for timely coordination of consults and care, and an expectation of a “normal” acute care course. All team members could work from the same sheet, much like an orchestra, keeping services and outcomes closely coordinated. Examples of diagnostic groups that benefit from pathway management include open heart procedures, acute coronary syndrome, congestive heart failure, diabetes, COPD, open cholecystectomy and C-Section. Agencies generally created pathways for their high cost/high risk population patients (we discussed this population earlier) to help control cost. Today, usage of pathways, care maps or algorithms are largely dependent on the perceived benefit or not used because of perceived disadvantages. Let’s consider a few of the benefits and disadvantages. Pathway Benefits • Set up to plan diagnostic testing, activity, diet, consults, transfer from high acuity unit to lower acuity unit, care is coordinated in timely fashion • Pathways can be used as a multidisciplinary charting note • The entire plan, for all providers, is readily available to all providers • Variances in the plan can be tracked easily (outcomes management) and include deviations in expected care or delay/missed diagnosis. – As an example: Mr. M is expected to have his foley dc’d on Day 2. It wasn’t dc’d till Day 3. The case manager can follow-up to find out what the “variance” was from the plan. Remember, the longer a foley is in, the greater the risk for a UTI. The case manager discovered that Mr. M had problems with CHF on Day 2, requiring diuresis. On further analysis, the real variance was caused by too much fluid given after the first 24 hours after surgery when the patient began to eat. Pathway Disadvantages • If a patient progresses faster than the plan allows for ( this is especially true if the plan is set up as Day1, Day2, Day3) many providers won’t move the plan along faster. • There may be redundancy in documentation increasing the likelihood for charting discrepancy • Inadequate feedback mechanisms to team players on their performance with pathways, maps and algorithms • Pathways requires revision to keep abreast of standards of care • Each patient being unique is not a reason to not use a pathway. Patients will generally follow the same course of recovery in the same amount of time. Rarely is the pathway delayed because of a patient variance. Usually the causes are system variance, staff variance, physician variance, process variance. Phase 3 Plan of Care • In the absence of pathways, maps or algorithms, the case manager puts into place a plan of care for the patient based on the initial assessment. Think back to the case management wheel. The case manager may consult or contact anyone of these services to provide the appropriate care the patient either for the hospital admission, or in anticipation of the discharge needs. Generally working autonomously, the orders are written, discussed with the patient, family and physician. A patient with CHF would need a dietary consult, a new onset diabetic would need to see the diabetic educator, a patient going home with a JP drain will need a home care visit. A patient having had a mastectomy might need a referral to clinical social work, home care and community resources for Reach to Recovery. Phase 4 • Depending on the severity of illness and the intensity of service, the patient will be followed until discharge. This may require daily visits or even more frequent trips and phone calls to coordinate services. How is the patient doing? Are the lab values improving? Is the wound healing? Can they ambulate better? Did the sister arrive from Kansas to take care of her brother? Will the insurance cover the cost of home care visits? These are just a few of the aspects of care the case manager monitors daily on the patients in his caseload. He always has to be anticipating discharge and the discharge plan. If the sister doesn’t get here from Kansas, the patient won’t be able to go home, but will need short term placement in a rehab unit. The referral will need to be sent, the PT/OT evals completed, the Rehab unit coordinator will need to assess the patient and the insurance company will need to approve the admission to rehab. Sometimes this has to be done with less than 24 hours notice. If rehab is denied, then the case manager needs to coordinate home care services or short term nursing home placement. Occasionally it can get pretty harried at discharge time, but the case manager needs to keep her cool and continue to coordinate and negotiate services for the patient. Phase 5 • The actual discharge usually falls together without too much difficulty. Within 24 hours of discharge the nurse case manager verifies the coordination of any post discharge services, such as home care, home social work, home hospice, home respiratory care, home O2, home DME and Meals on Wheels. • All scripts are written and placed with the chart. • Resources are identified if the patient does not have prescription coverage. (at our hospital we provide 1 month of indigent prescriptions free at discharge). • Discharge instructions are reviewed with the patients. • Referrals to outpatient community educators are written. • Direction and community resources for alcohol and substance rehab are provided when appropriate. • For inpatient rehab, long-term vent placement or nursing home placement, ambulance transportation is arranged for, the appropriate records are copied for transfer with the patient and the family is notified. • All morning diagnostics and any pending diagnostics are reviewed with the attending before discharge. Phase 6 • Outcomes Management • One of the most important steps in the case management process is the evaluation of the entire process. What were the results and consequences of the care provided? or not provided? An honest evaluation of case outcomes allow for policy and procedure changes in the case of poor outcomes, or employee/unit recognition in the case of excellent outcomes. • Let’s think back on the example of Mr. M and his episode of CHF requiring his foley to stay in an extra day. The real variance was IV fluid that continued after he started eating. A quality group met, which included Mr. M’s case manager and cardiologist. From that group, a new policy was created. – All patient’s admitted with CHF would have their IV heplocked. – Patient’s admitted with CHF and ordered to have IV fluid (to replace K+ or Magnesium, etc), would automatically have fluid restriction of 1500cc q 24hours. – The case manager would track patients admitted with CHF over the next 6 months and the group would reconvene to see if the policy change and new standing orders resolved the problems. Resources for Case Managers • • One of the most valuable tools a case manager can possess is his little black book. Developing a solid working relationship with community resources will greatly enhance the success of the case manager. Building your resources might include a Resource Manual: – – – – – – – – – – – – – – Local Pharmacies DME Companies Home Health Care Agencies Drug Vendors Long Term Vent Facilities Hospice Organizations Community Educators Public Health Organizations Mental Health Services Alcohol Treatment Programs Indigent Health Clinics Indigent Well-Baby Clinics Indigent Public Transportation Dialysis Clinics Resources for Case Managers page 2 • Internet Resources/Certification and Degrees • http://getinfo.kaplan.edu/Microsite_B/index.as px?ProspectID=B96EC3B53C91458E8D9F2E2 7AE9F0CE8 • http://gradstudies.carlow.edu/casemanage_certi ficate.html • http://www.allnursingschools.com/schools/ID1 24/ Conclusion • This presentation provides a glimpse into the role and profession of case management. The real challenge for each of us in the decades to follow will be balancing the provision of quality, health care for patients with disease, while assisting society toward managing their own health: to change our mindsets from fixing diseases states to promoting health and wellness. References • Cresia, J.L., Parker, B. (2001). The bridge to professional nursing practice. 3rd ed Mosby; St. Louis. • Powell, S.K. (2000). Advanced case management: Outcomes and beyond. Lippincott; Philadelphia. • Powell, S.K. (2000). Case management: A practical guide to success in managed care. Lippincott; Philadelphia. • Powell, S.K. (1996). Nursing case management: A practical guide to success in managed care. LippincottRaven; Philadelphia.