Clinical Case 3
advertisement

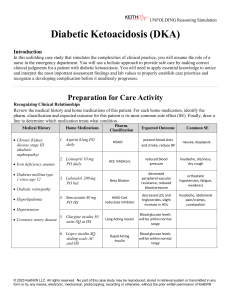
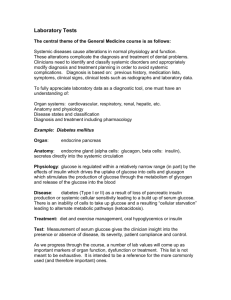
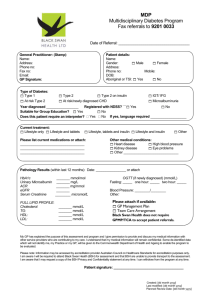
Clinical Case 3 • A 14 year old girl was brought to her GP’s office, complaining of: – – – – – weight loss, dry mouth, lethargy, easy fatigability and difficulty in catching the breath; • The symptoms were noticed by the parents about 10 days before the visit • However, the patient herself had noted an increased frequency of urination (polyuria) and increased thirst (polydipsia) about 8–10 weeks prior • A urine analysis using reagent strips revealed positive glucose and ketones respectively • Her temperature was 39°C and a chest examination revealed some congestion • The patient was immediately admitted to hospital for management • Clinical examination revealed: – – – – – a dehydration, fruity odour to the breath, tachycardia (120 beats/min) and dry mouth, lips and tongue The respiratory rate was 30/min and her blood pressure was 110/70 mmHg Laboratory Investigating • Laboratory data indicated that: – – – – – – – – – – her plasma glucose level was 470 mg/dl (70-110 mg/dl) serum acetone was positive arterial blood pH was 7.18 (7.35–7.45) with a bicarbonate level of 17 mmol/l (21–28 mmol/L) Other serum values determined at this time were Na+ 130 (136–145 mmol/L) K+ 5.8 (3.5–5.0 mmol/L) Cl– 92, (96–106 mmol/L) and glycosylated haemoglobin 13.1% (< 6.8%) blood islet cell antibodies were positive What is the most likely diagnosis in this patient? What are the causes of her observed symptoms? • This is a classical presentation of diabetic ketoacidosis in Type I diabetes patients • The common symptoms of diabetes mellitus are: – polyuria (increased urine volume and frequency) – polydipsia (increased thirst) – and polyphagia (increased appetite) • Polyuria is secondary to the osmotic diuresis (caused by excess filtered glucose in the urine) which then triggers increased thirst • Diabetic ketoacidosis is a serious acute complication that requires prompt attention – It is usually precipitated in Type I diabetes patients by a stressful stimulus (e.g. an infection, surgery or acute illness) – or by omitting several insulin injections • The characteristic sweet smell to the breath is due to excretion of acetone (ketone body) formed by condensation of excess acetyl CoA in the liver • appearance of other ketone bodies in the blood (acetoacetate and 3-hydroxybutyrate) decreases blood pH (metabolic acidosis) which stimulates respiration (hyperventilation) What would be the most appropriate treatment while in hospital, and the recommended therapy on discharge? • Following a diagnosis of diabetic ketoacidosis, intravenous fluid replacement and correction of hyperglycaemia/ ketonaemia is crucial for effective hospital management • A precipitating cause such as an infection should also be sought and treated with appropriate antibiotics if necessary • The patient was started on intravenous fluid (normal saline) and soluble insulin infusion (0.2 units/kg followed by 0.1 units/kg per hour) to correct for the underlying dehydration and metabolic abnormalities • In the next 14 hours, the blood glucose was stabilized at 140 mg/dl and the patient rehydrated • Serum electrolytes returned to normal – – – – bicarbonate level increased to 22 mmol/l and arterial blood pH showed normalization to 7.35 Insulin infusion was continued until next morning when ketones were no longer present in the diluted serum – The patient was switched to subcutaneous insulin administered twice daily – She was instructed in home blood glucose monitoring methods and discharged on stable doses of insulin three days later