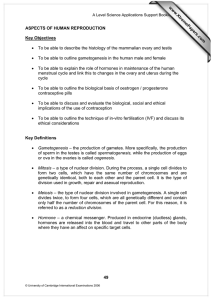
Aspects of Human Reproduction
advertisement
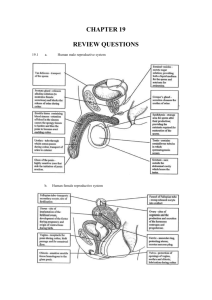
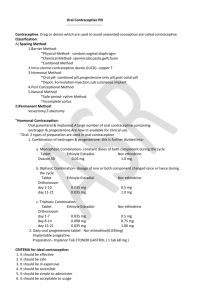
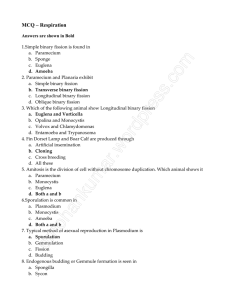
Aspects of Human Reproduction Histology of ovary Histology of testis Gametogenesis • The process of formation of gametes from the germ cells in the testes and ovaries. • The timing of the developmental stages of gametogenesis, and the number of gametes produced are very different in male and female germ cells. • In the male spermatogenesis occurs from puberty to old age, at an average rate of 1.5 million spermatozoa per minute. • In females all oocytes ever to be formed in females are produced during foetal life. • At birth the ovaries contain about 2 million oocytes. • All the oocytes go into meiotic arrest when they reach the first meiotic division during foetal life. • The primary oocytes remain in prophase of the first meiotic division until the time of puberty, when they are gradually released to complete meiosis at regular intervals known as the ovarian cycle. • On the average only one oocyte matures during each cycle, which occurs at approximately monthly intervals, so that the total amount of oocytes to be ovulated is about 500 oocytes in a lifetime. Spermatogenesis • It occurs in the seminiferous tubules of the testes. • The process begins at the outer edge in the germinal epithelium and moves in towards the lumen. • The beginning cells are called spermatogonia and they divide by mitosis. Some develop into primary spermatocytes which divide by meiosis. The first division produces secondary spermatocytes which are haploid. Spermatogonia • The second division forms spermatids which are also haploid. barrier) The tails sticks into the lumen. The spermatozoa head is attached to a Sertoli cell which nourishes and protects the cell Oogenesis • Occurs in the ovary while the girl is still an embryo. • Germinal epithelial cells divide by mitosis to form diploid oogonia. Some start to divide by meiosis and are called primary oocytes. At puberty some divide into two haploid cells. One large one (secondary oocyte) and a small one (polar body) • The secondary oocyte divides up until metaphase II. • Only after ovulation does the final stage of meiosis occur and the polar bodies fall away. • The developing oocytes are found inside follicles in the ovary. • The wall of the follicle contains granulosa cells which protect and secrete hormones. Menstrual Cycle • There are a number of hormones involved in the control of the human menstrual cycle. • Two are produced by the ovaries: – Oestrogen (produced by follicle cells) – Progesterone (produced by corpus luteum) • Two are secreted by the anterior pituitary gland: – Luteinising Hormone (LH) – Follicle Stimulating Hormone (FSH) • Oestrogen is secreted at the onset of puberty, causing an increase in the size of the reproductive organs and the development of secondary sexual characteristics. • The main role of oestrogen is to prepare the endometrium (lining of the uterus). • The duration of a normal menstrual cycle is 28 days – day 1 is the first day of menstruation. • The main hormonal changes during the cycle are as follows: • FSH and LH increases slightly during the first few days causing a number of primary follicles to develop. (only one in one ovary continues to develop) • The granulosa cells of the developing follicle secrete oestrogen. • The increase in the level of oestrogen inhibits FSH and LH • The oestrogen causes the endometrium to thicken – by day 12 it is 3 – 4mm thick • Day 12 LH rises very sharply inhibiting oestrogen in granulosa cells and starting secretion of progesterone. • Ovulation day 14 • When egg released, remaining granulosa cells fill up with a yellow substance and is called a corpus luteum or yellow body, • This continues to secrete large amounts of progesterone and small amounts of oestrogen. • The progesterone develops the endometrium, increasing its supply of blood. • Its thickness reaches 5 – 6 mm and it is prepared for implantation, if the egg has been fertilised. • If no fertilisation, the oestrogen and progesterone inhibit FSH and LH from the anterior pituitary gland and the corpus luteum degenerates. • All four hormones fall to a low level and, once the oestrogen and progesterone have dropped far enough, the anterior pituitary again begins to secrete FSH and LH and the cycle begins again. • The fall in oestrogen and progesterone causes the endometrium to break down and menstruation occurs during the next four to seven days of the cycle. The oestrogen/progesterone contraceptive pill • • • • It contains oestrogen and progesterone changes the hormone balance of the body, and ovulation does not take place. The high levels of oestrogen and progesterone inhibit the release of FSH and LH from the anterior pituitary gland. • It also causes the mucus made by the cervix to thicken, forming a ‘mucus plug’ in the cervix – this makes it more difficult for the sperm to get through to the uterus. • It also makes the lining of the uterus thinner With most oral contraceptives, a woman will take the pill for 21 days and then stop for 7. During the 7 days, menstruation takes place. (sometimes a different coloured pill is taken at this time, that has no effect, but it keeps the routine going. Morning After Pill Works for up to 72 hours after intercourse, by preventing embryo from being implanted into the uterus. The biological, social and ethical implications of the use of contraception • Biological implications • methods of contraception which do not involve hormones (e.g. barrier methods etc.) do not have any biological implications. But hormonal ones have many. • Benefits: – Reduces the risk of developing certain ovarian cysts – Reduces the risk of developing cancer of the ovary or uterus – Menstruation is more regular and can relieve premenstrual tension – Reduces the risk of pelvic infection – the mucus plug may prevent bacteria getting into the uterus • Side effects and possible risks: –Some women may develop nausea and head aches –Tiredness and mood changes –Rise in blood pressure –Increased risk of thrombosis. May cause a stroke or a blood clot in the lungs –Small increased risk of breast cancer • Social implications • Contraception means that it is easier to choose when to have or not to have children. • Plan families around careers and other considerations, such as financial circumstances. • Population control can be good and bad. – Some places have too few children to be able to sustain the population in the future. – Other places continue to have problems of overpopulation and the implications that this has for supply of food, water and other resources. • Ethical implications • The benefits: – a woman can decide when and if she will conceive – countries can control their population growth – those at medical or psychological risk if pregnant, can avoid such pregnancy – reduced chance of unplanned pregnancy in sexually active teenagers • artificial contraception seen as morally wrong In vitro fertilisation • In-vitro is Latin for ‘in glass’ • Eggs are fertilised outside the woman’s body. • By controlling ovulation through the administration of hormones, removing eggs from the ovaries and allowing sperm to fertilise them in a fluid medium. ovarian stimulation • Treatment starts on the third day of menstruation. • Hormones stimulate the development of multiple follicles in the ovaries. • About 10 days of injections necessary. • The oocytes are collected using a hollow needle inserted through the vaginal wall and into the developing follicles. • The egg is sucked out. • The sperm are collected on the same day and placed in special medium which only strong motile sperm can swim through. • Each oocyte is placed in a dish and 100 000 sperm are added with a nutrient medium. • If fertilisation does not occur then DNA is injected directly into the oocyte. • Left for 3 days. • Two or three fertilised ones are chosen and implanted into the uterus wall. Ethical issues • The fate of the unused embryos • Embryos can be used as stem cells. • Should we have the power to choose whose sperm is used?