CHAPTER 19
advertisement
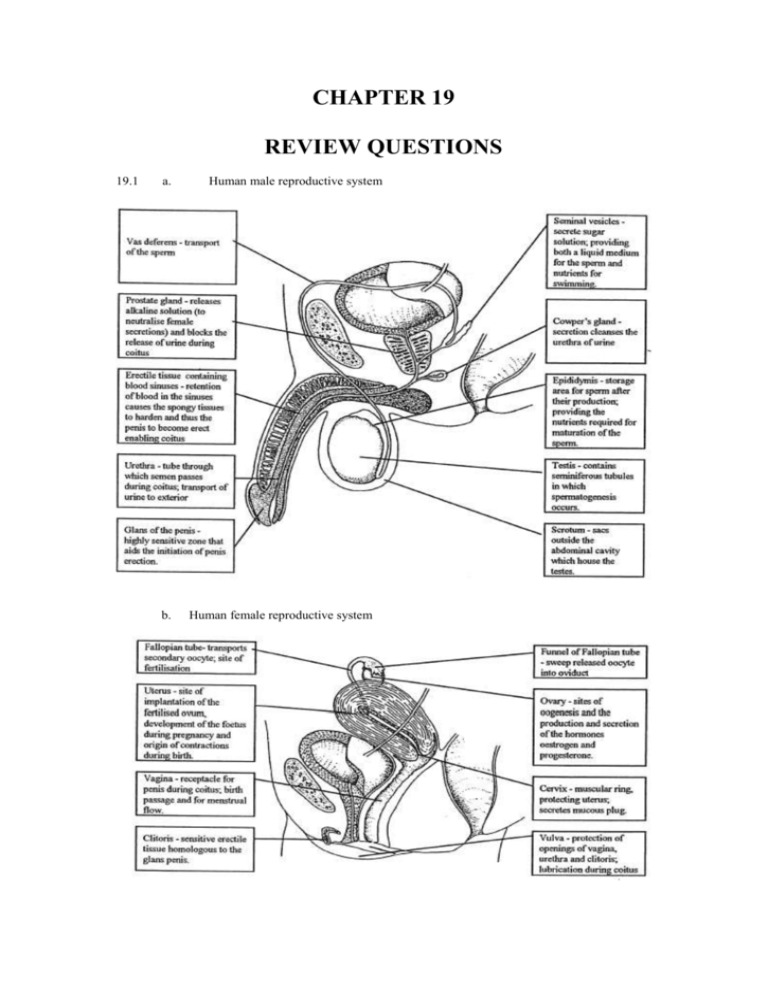
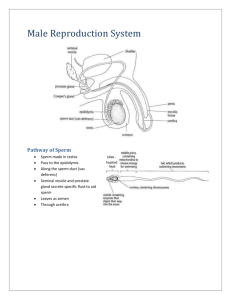
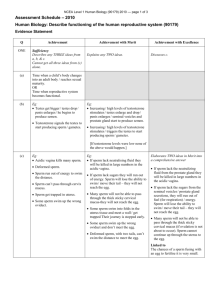
CHAPTER 19 REVIEW QUESTIONS 19.1 a. b. Human male reproductive system Human female reproductive system 19.2 a. b. c. d. 19.3 a. Hormone FSH Site of production Anterior pituitary LH Anterior pituitary Oestrogen Ovary Progesterone Corpus luteum of ovary b. c. d. e. 19.4 B: corpus luteum. D: M, K, L, N, O, J. i. haploid (but each chromosome consists of 2 chromatids) ii. diploid iii. diploid iv. diploid Progesterone: inhibits FSH and produces thickening and increased vascularisation of the uterine wall in preparation for implantation. a. Site of action Stimulates development of ovarian follicles and seminiferous tubules. Stimulates ovulation (Graafian follicle) and converts empty follicle into corpus luteum, stimulating progesterone production; stimulates testosterone production. Initiates and maintains female secondary sexual characteristics; initiates thickening of the uterus; stimulates FSH and LH. Maintains thickening of uterine wall, inhibits FSH. Negative feedback: with increasing progesterone levels there is a decrease in both FSH and LH. Positive feedback: increasing levels of oestrogen are accompanied by an increase in LH. i. Repair: oestrogen. ii. Proliferation of secretory tissue: progesterone. During late foetal development, germ cells undergo repeated mitotic divisions to form diploid primary oocytes that remain in a prophase I stage, surrounded by a layer of cells, the entire structure being called a primary follicle. At puberty, secretion of FSH stimulates one primary follicle to continue suspended meiosis. The follicle cells surrounding the primary oocyte proliferate and form a fluid filled cavity in which the dividing oocyte is suspended. The entire structure is called a Graafian follicle. It moves slowly towards the surface of the ovary, and under the influence of oestrogen and LH, ruptures to release the secondary oocyte in the process of ovulation. If pregnancy occurs the corpus luteum is maintained for a period of about 3 months, and the progesterone secreted (along with ovarian secretions of oestrogen) to maintain the uterine wall. With the development of the placenta that produces oestrogen and progesterone, the corpus luteum breaks down. Presence of progesterone inhibits FSH production. Over the period of gestation the levels of oestrogen increase and progesterone decrease. At a critical balance between these two hormones, the posterior pituitary is stimulated to produce and release oxytocin which initiates parturition through contraction of the uterine muscles. Expulsion of the placenta, and associated drop in oestrogen and progesterone levels, stimulates release of prolactin from the anterior pituitary which acts on the mammary glands to stimulate milk production. b. c. Muscular contractions of the vas deferens carries the sperm from the epididymis to the urethra which traverses the penis. Along its route, a large number of nutritive and fluid substances are added to the sperm, forming semen, from the seminal vesicles, Cowper’s gland and the prostate gland. During coitus, the semen is ejaculated into the vagina, near the cervix. The sperm swim, in the fluid provided in semen, using the sugars for respiration to provide energy for movement, through the cervix and uterus towards the Fallopian tubes. This is aided by muscular contracts of the female tract. Fertilisation occurs in the Fallopian tube. When the sperm reaches the oocyte, acrosomal enzymes digest the surrounding oocyte membranes, allowing entry of the sperm head and middle section. This stimulates the formation of an impenetrable fertilisation membrane around the oocyte, preventing entry of further sperm. The sperm nucleus in the oocyte stimulates completion of meiosis in the secondary oocyte to form the ovum and second polar body. The second polar body degenerates and the nuclei of the sperm and ovum unite to form the diploid zygote. 19.5 Eight days. 19.6 a. b. c. d. Instigate and effect parturition. Bathes embryo, preventing it from dehydrating; aid in buffering against mechanical shock. Connection between the foetus and the placenta through which blood vessels flow. Allows diffusion of materials between the developing young and the mother. 19.7 Production of progesterone which maintains the uterine wall and inhibits FSH. Production of oestrogen that maintains the uterine wall and which later in gestation stimulates release of oxytocin. Provides diffusion pathway for oxygen and nutrients from the mother to the foetus. Provides a diffusion pathway for metabolic wastes from the foetus to the mother. Provides a barrier that limits the transfer of some solutes and blood components from maternal to foetal circulation (e.g. cells of the mothers immune system which might result in rejection of the foetus). 19.8 End of first trimester: human likeness with enlarged head and brain, external genitalia, excretory and respiratory systems are developing; presence of arms and legs which move, and facial expressions. Approximately 56 mm long. End of second trimester: further elaboration of all systems and increased size (112 mm long); face looks ‘human’; head hair appearing; most bones distinct. End third trimester: all systems complete development; body becomes rounded due to fat accumulation; approximately 350 mm long. 19.9 The white blood cells are involved in the immune response. Since the baby has a genetic constitution derived from both the mother and father, it may not have all of the identification tags which the mother’s immune system recognise as ‘self’. If this is the case an antigenantibody reaction could occur within the foetus that could result in developmental anomalies or rejection of the foetus through spontaneous abortion. 19.10 Dizygotic: two ova a released and each is independently fertilised. Monozygotic: developed from a single fertilised egg that separates during early embryonic cleavage into two individual embryos. 19.11 They have exactly the same genetic information so are clones. 19.12 Mirror image twinning occurs when separation of the cells of the blastula occurs between days 8 and 13. The twins develop within the same amnion and chorion and share a single placenta. If separation of the blastula cells occurs it is usually between days 4 and 8 and thus this type of twins is rare. 19.13 Co-joined twins are physically joined at some part of the body. This is because separation of the blastula cells is incomplete after some differentiation of cells, i.e. after day 13 from conception. 19.14 The co-joining often involves sharing of vital organs. 19.15 A karyotype is a display, constructed from micrographs of chromosomes, showing the numbers and types of chromosomes of an individual of a species. 19.16 A sex chromosome is one which carries information determining the gender of the individual. All other chromosomes are termed autosomes. 19.17 a. b. c. d. Deletion: a segment of a chromatid which has broken off during metaphase I has not been replaced by the corresponding segment of the homolog. Duplication: occurs when a broken off segment of a chromatid attaches to the homolog with out a corresponding exchange during meiosis I. Thus half of the daughter cell will have the same information on one chromosome doubled up whilst the other half of the cells will have no record of this information (deletion). Translocation: occurs when a segment of one chromatid joins to a non-homologous chromatid during meiosis I. Non-disjunction: occurs when a pair of homologous chromosomes fail to separate during anaphase I. Thus half the gametes from that division have two of the particular chromosome and half have none. 19.18 An autosomal non-disjunction of chromosome 21 occurs in individuals displaying Down syndrome – these individuals have three of this chromosome. Klinefelter syndrome occurs in individuals with a sex chromosome complement of XXY resulting from non-disjunction of the X chromosome in egg formation. 19.19 In amniocentesis a small sample of amniotic fluid is removed by insertion of a fine syringe through the abdominal , uterine and amniotic walls. In chorionic villus sampling a tiny piece of the chorionic is removed. Since both the amniotic fluid and chorion is genetically identical to the baby (they are extra-embryonic tissues), analysis of the chromosomes and genes of these samples may detect any genetic anomalies in the foetus at an early stage of development. 19.20 The ultrasound shows the position of the foetus and surgical instruments, so that no damage is done to the foetus. 19.21 Cystic fibrosis, Huntington’s chorea, muscular dystrophy, haemophilia, thalassaemia and Down syndrome. 19.22 It can be performed at a much earlier stage of foetal development, if the foetus is afflicted with a genetic disease and the mother opts for medical abortion. The earlier this is done, the less medical and traumatic risk there is for the mother. 19.23 From birth to sexual maturity there is rapid growth. In humans this occurs in two stages , one in early childhood and the other during adolescence. At puberty there is a surge of the sex hormones (testosterone in males and oestrogen in females) which results in the development of the secondary sexual characteristics typical of the gender. During adolescence the body completes its growth and development. Final adult size is normally achieved by age 20. Later in adulthood, many cells may begin to deteriorate and the process may result in negative growth and various forms of senility. 19.24 a. At puberty in the male there is a surge of testosterone which initiates maturation of the primary and secondary sex characteristics: enlargement of penis, testes and accessory glands sperm production facial, underarm and pubic hair develops musculature increases the shoulder bones increase in width b. fat becomes deposited in the abdomen the larynx enlarges and vocal chords thicken, to produce a deeper voice increased body odour resulting from stimulation of sweat glands by androgens behavioural changes associated with preparation for adulthood which include increase in aggressiveness and loudness, mood swings increased growth. Puberty in females is also associated with an increase in sex hormones which stimulate the final development of the reproductive structures and secondary sexual characteristics: enlargement of breasts and hips increased activity of the sweat glands development of pubic and underarm hair deposition of fat around the hips behavioural changes including mood swings, particularly due to increased sensitivity prior to menstruation when progesterone levels are high increased growth. 19.25 Senescence is cell aging, often associated with decreased production of sex hormones as the individual ages which may result in muscle and bone deterioration. Senescence may lead to senility or decreased mental competence due to decreased levels of oxygen to the brain associated with loss of muscle tone which affects blood circulation. 19.26 Oestrogen mimics in the male are believed to cause low sperm counts; in pregnant females they can modify foetal development, particularly sexual development. The behaviour patterns of the genders are also affected, with increasing feminisation in males and increasing male behaviour by females. All of these factors can result in decreased population size.