Therapeutic Hypothermia - IHLF - Illinois Heart & Lung Foundation
advertisement

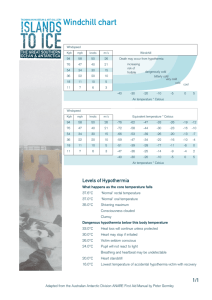
Therapeutic Hypothermia John S. Burr, MD, FCCP Illinois Heart and Lung Associates Advocate Medical Group Therapeutic Hypothermia • No relevant disclosures Therapeutic Hypothermia • Mild hypothermia by definition • Also known as Targeted Temperature Management (TTM) • What we originally knew about hypothermia came from cases of accidental hypothermia • Mammalian diving reflex is an example of prolonged brain survival in hypothermia Accidental Hypothermia • Unintentional decline in core temperature below 35°C Mild Hypothermia 90-95 F 32.2-35 C Moderate Hypothermia 82.4-90 F 28-32.2 C Severe Hypothermia <82.4 F <28 C • Mild Hypothermia is used therapeutically to decrease risk, increase benefits Danzl D and Pozos R. NEJM, 1994;331:1756-1760 Accidental Hypothermia Danzl D and Pozos R. N Engl J Med 1994;331:1756-1760 Therapeutic Hypothermia • Post Cardiac Arrest: VF/VT • • • • • • • Ischemic and Hemorrhagic Stroke Traumatic Brain Injury Spinal Cord Injury Acute Liver Failure: cerebral edema Newborn hypoxic / ischemic encephalopathy Limiting infarct size in MI in non arrest patient Miscellaneous: CO poisoning, hanging, near drowning, choking. Therapeutic Hypothermia • Randomized trials supporting therapeutic hypothermia in cardiac arrest – Bernard, SA et al., NEJM, Vol 346, No. 8, pp 557563, Feb 21, 2002. Australian Study (smaller) – Holzer, M et al., NEJM, Vol. 346, No. 8, pp 549556, Feb 21, 2002. Austrian Study (larger) Therapeutic Hypothermia • Melbourne, Australia- Bernard, et al. – N=77 patient recruited with strict inclusion criteria over 33 months. Men>18, Women>50, VF arrest, coma from other than circulatory arrest excluded – Persistent shock after resuscitation excluded – Cold packs to head/chest to cool within 2 hours from arrest and maintained for 12 hours – 49% Hypothermia and 26% Normothermia group with good neurological outcome. NEJM, Vol. 346, No. 8, 557-563 Therapeutic Hypothermia • Melbourne, Australia- Bernard, et al. – Differences in sex between groups: 58% male in Hypothermia and 79% male in Normothermia – Bystander CPR: 49% Hypothermia 71% Normothermia (might skew to diminish effect) – Lidocaine IV used in all and SG catheter – No mortality difference in this study, just improved neurological outcome NEJM, Vol. 346, No. 8, 557-563 Therapeutic Hypothermia NEJM, Vol. 346, No. 8, 557-563 Therapeutic Hypothermia • Vienna, Austria- Holzer et. al. – N=275, recruitment criteria more strict, recruitment time period not mentioned – 92% screened not eligible: generalizable? – VF/pulseless VT, Witnessed arrest, Down < 15 min – ROSC (return of spontaneous circulation) < 1 hour – Age 18-75, excluded: pregnancy, TM < 30 C, preexisting coma prior to arrest, hypotension, rearrest after EMS arrival, response to verbal commands (GCS too high), pre-existing coag. NEJM, Vol. 346, No. 8, p 549-556 Therapeutic Hypothermia • Vienna, Austria- Holzer et. al. – Cooling different: cold air mattress • Time average to target temp 8 hours • 19/136 patients target not reached (14%) – Hypothermia 75/136 (55%) good neuro outcome – Normothermia 54/137 (39%) good outcome – Mortality (H) 41% vs (N) 55% • There is consensus based on aspects of both trials to guide patient selection for therapeutic hypothermia NEJM, Vol. 346, No. 8, p 549-556 Therapeutic Hypothermia • Both studies ROSC < 60 min- average 20-25 • Australian study cooled at beginning with cold packs to head and torso • Austrian trial ROSC to cooling 105 minutes with IQR (65-192) • Similar target temperature, 12 hr vs 24 hr • VF/VT arrest with reasonable parameters for ROSC and reduced presenting mental status Therapeutic Hypothermia • Miracle Max (Billy Crystal) summarizes: • Efforts at cerebral salvage- appropriate patient Therapeutic Hypothermia • Who to cool? – Adults resuscitated with ROSC from witnessed arrest of presumed cardiac etiology – Initial rhythm VF/pulseless VT – May also benefit but more study needed: ROSC from other initial rhythms: asystole, PEA, ?resuscitation from in-hospital cardiac arrest – Patients who do not have absolute criteria for avoiding hypothermia Therapeutic Hypothermia • Who NOT to Cool: Absolute – Patients with TM temp <30 C (all dead) – Patients who already have coma prior to arrest – Patients with Glascow coma score > 7 (mostly alive with relatively preserved neurological function) – Terminally ill or have advanced malignancy – Obviously DNR excluded Therapeutic Hypothermia Therapeutic Hypothermia • Who NOT to Cool: Relative – > 15 min to initiation of BLS – Time to ROSC of > 60 minutes – Time from arrest to initiation of cooling > 6 hrs – Hemodynamic instability SBP > 90 without pressor – Intracranial pathology until assessment/imaging – Inappropriate for ICU: multi-organ dysfunction, severe sepsis, comorbidity decreasing survival – Traumatic full arrest: coagulopathy, hemorrhage Therapeutic Hypothermia • Who NOT to Cool: Relative – – – – – – – – Pregnancy: risks/benefits discussed with OB Extremes of age Bleeding ongoing or inherited coagulopathy Surgery < 48 hrs before or major trauma to spleen or liver Sepsis is reason for arrest QT prolongation Prolonged hypoxemia, SaO2 < 85% for > 15 minutes after ROSC Thrombocytopenia < 50K, initial asystole, coma (med) Therapeutic Hypothermia • Physiologic changes during hypothermia – Brain injury during arrest and salvage by cooling – Cardiovascular effects – Respiratory effects – Renal effects – Musculoskeletal – Immune system and infection – Endocrine/Metabolic/Hematologic Therapeutic Hypothermia • After BLS and ACLS to ROSC: BE COOL Therapeutic Hypothermia Therapeutic Hypothermia • By multiple mechanisms proposed above, cooling prevents spread of already existing anoxic/ischemic neural injury, limiting damage and thereby treat post-resuscitation disease • Current target of 33 C, mild hypothermia, has less risk than severe hypothermia of causing other systemic side effects • The temperature of benefit may be 36 C ? NEJM 2013; 369: 2197-2206 Therapeutic Hypothermia Overall goal of post-resuscitation cooling Therapeutic Hypothermia • Cardiovascular effects: – Decreased HR and increased BP (increased SVR) – Cardiac output decreased (SV decreased, diuresis) – CVP maintained by venocontriction – Increased SvO2 despite CO due to decreased peripheral oxygen extraction from cellular respiration. Myocardial O2 extraction also so myocardial oxygenation improves despite decreased coronary blood flow Therapeutic Hypothermia • Electrical changes during decreased temp: – Increased PR, QRS, QTc but Osborn waves rare at mild hypothermia. AF, VF, Asystole more common when <30 C but most common <28 C Therapeutic Hypothermia • Respiratory Effects – Decreased RR and Minute Ventilation (but on ventilator is whatever you set) – Increased serum gas solubility for O2/CO2 so if ABG not temp corrected overestimate PaCO2 by about 10 mm and O2 by about 20 mm Hg (shoot for PaO2 85-100 mm Hg if not temp corrected) – Left shift of O2/Hemoglobin dissociation so less O2 delivery but again, less cellular respiration unless shivering starts to increase metabolism Therapeutic Hypothermia • Renal and electrolyte changes – Volume loss due to cold diuresis: venocontriction then increased ANP, decreased ADH leading to polyuria. Also decreased concentration capability from decreased ion pump activity in Loop of Henle – Decreased serum levels of electrolytes: K, Mg, P • Increased urine flow with renal tubular dysfunction • Intracellular movement of K, Mg, P – Electrolytes move back out during re-warming Therapeutic Hypothermia • Musculoskeletal effects: – Shivering leads to increased oxygen consumption which lead to increased temperature, increased work of breathing, HR, increased myocardial O2 demand – Antagonizes efforts to maintain cooling so must be controlled by counter-warming or pharmacy including sedation with or without paralytics Therapeutic Hypothermia • Immune and infectious problems: – Immune/inflammatory suppression two-edged sword in that cerebral complication reduced while increased susceptibility to infection – Increased pneumonia risk with cooling >> 24 hrs – Increased wound infection with decreased WBC function, skin vasoconstriction, and pressure and irritation from cooling pad contact Therapeutic Hypothermia • Endocrine/Metabolic considerations: – Decreased metabolic rate 8% per degree C – Drug levels increased due to decreased hepatic clearance ( enzyme function, blood and bile flow) – Hyperglycemia from decreased insulin sensitivity and secretion • Hematologic: – Hct (concentration), Plt function, coag function, but the risk of spontaneous bleeding is low Therapeutic Hypothermia • Selection of candidate: evidence covered as above: out of hospital arrest VF/VT with GCS 7 or less and no contraindications • Physiologic consideration in hypothermia, most importantly brain salvage, covered • We will now turn toward practical considerations in implementing hypothermia as therapy in ICU Therapeutic Hypothermia • Team Approach to management – MD: ER, Cardiology, Neurology, Critical Care – Nursing: ER, Cath Lab, CC nurses, clinical nurse specialists/educators, nurse managers – Respiratory Therapy – Pharmacy and Laboratory support – Pre-hospital care by EMS personnel Therapeutic Hypothermia • Pre-hospital attempts to cool in the field: ice bags (in Australian study), iced saline, cool air evaporative cooling: no convincing evidence (yet) that superior to cooling on ER arrival Reindeer nasal cooling Post arrest cool dry air Circulation. 2010;122:737-742 Therapeutic Hypothermia • General Care on Arrival: – Communication between ER, Cardiology/Cath Lab, Critical Care – Head CT, 12 Lead EKG, Labs: CBC/BMP/Troponin, Lactate, coags – If STEMI, cath lab if deemed appropriate – Three phased hypothermia protocol: complex longitudinal care so ICU bundle/caremap Therapeutic Hypothermia • Initiation of Cooling – Patient assessment for protocol and start in ED or cath lab. If not comatose, decide if appropriate. • Maintenance – Decrease and maintain temperature at goal with ongoing supportive care: manage shivering • Re-Warming – 24 hours after cooling initiated with slow controlled rise in temperature and monitoring Therapeutic Hypothermia Numerous methods to maintain hypothermia: surface and catheter based common Polderman, KH, Intensive Care Medicine, 2004 Therapeutic Hypothermia Core Cooling Therapeutic Hypothermia Blanket Cooler Therapeutic Hypothermia Surface Cooling Therapeutic Hypothermia Overview of Process Therapeutic Hypothermia • Equipment as above and– Arterial line important with hemodynamic change – Central line for drug and pressor delivery. Australian study used PA catheters but most studies did not uniformly insert – Temperature monitoring by PA cath, esophageal probe, caution with bladder temp only if patient oliguric/anuric, rectal temp – Sedation, Treat shivering, paralysis vs skin counter-warming, EEG if available Therapeutic Hypothermia • Continuous assessment – Metabolic disturbances, arrhythmias, Glucose level, Sedation and Pain level, Shivering, Seizure, Skin Breakdown, Infection/fever, Bleeding – Temperature by core method with back up – IVF to replace diuretic losses, sedation and analgesia, NM blocker vs counter-warming – Vasopressor may be needed MAP >80 preferred for CPP – IV insulin if needed for hyperglycemia Therapeutic Hypothermia • Sedation deeper if NM blockade, consider BIS monitoring although accuracy based on evidence is questioned at < 35 C • The importance of shivering is the increased metabolic heat production slows/impairs target temp acquisition • Shivering early signs decreased SvO2, increased RR, facial tensing, noise on EKG, palpable muscle fasciculation of face or chest Therapeutic Hypothermia • Shivering: – Optimize sedation and analgesia – Bair Hugger Device for counter warming can decrease shivering – Paralytic IVP if above ineffective – Paralytic infusion only if above ineffective – Deep sedation for paralysis if needed and periodic assessment of TOF (train of four) which is assessed prior and during infusion Therapeutic Hypothermia • Fever can be commonly secondary to aspiration pneumonia/itis from arrest • Cultures, WBC with diff, empiric coverage for source • Add Tylenol to antibiotics to prevent hyperthermia from undoing your hard work Therapeutic Hypothermia • Skin breakdown is higher risk with peripheral vasoconstriction and pressure from cooling pads if used • Every 2 hours with turning do skin survey • Care in applying cooling device on areas of fragile skin or wound Therapeutic Hypothermia • Slow re-warming starts 24 hours after the onset of the cooling phase (not when TT reached) • Rewarming should proceed no faster than 0.25 C or 0.5 F per hour averaged over 4 hrs • Goal 36.5 to 37 C with temperature (clamping) maintained normo-thermic for 48 hours. Therapeutic Hypothermia • While cool replace K, Mg, P to LLN as needed and discontinue replacement while rewarming • If using paralytic, discontinue when 36 C • Watch for hypotension secondary to peripheral vasodilation and replace intravascular volume with additional crystalloid as need Therapeutic Hypothermia • Careful selection of appropriate candidate • Mindfulness of physiologic changes of hypothermia • Reach goal temperature as soon as possible and maintain 24 h with slow rewarming • Shivering and Fever need to be controlled to help protect the brain • After arrest, hypothermia allows more people to go back to independent living with good cognitive function Case of VF Arrest • 53 yo female went to work with vague CP • Arrest near cafeteria at work, AED delivered shock, intubated in field, CPR for PEA (but no epinephrine given), given versed for agitation then placed on propofol drip in ER • At the time critical care called patient was unresponsive on propofol drip • Should she be chilled or continue current care? Thank You The Importance of Bedside Assessment