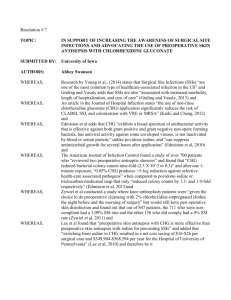
Evidence Based Practice Regarding Chlorhexidine Use to Prevent
advertisement

Presented by: Cindy Magirl Eric Nelson Tennille Sassano Jennifer Vicarie What does the literature say about the use of Chlorhexidine in the prevention of surgical site infections (SSI’s)? • It is estimated that between 750,000 and 1 million SSIs occur in the United States each year (Edmiston et al., 2010). • SSIs remains a substantial cause of post-operative morbidity and increased health care costs (Riley et al., 2012). • SSIs result in 3.7 million additional hospital days and $845 million spent nationally. (Zinn et al., 2010) The aim is to evaluate the effectiveness of evidence-based prevention and control strategies to reduce rates of SSIs. Patient (intrinsic) • • • • • • • • • • • Procedural (extrinsic) Age Diabetes (metabolic disease) Perioperative hyperglycemia Tobacco use Concurrent infection (distant) Obesity Malnutrition Immunocompromise Low preoperative serum albumin level Corticosteroid use Prolonged hospitalization before surgery • Prior radiation to surgical field tissue • Staphylococcus aureus colonization • Lack of preoperative shower • Site shaving the night before surgery • Extended operative time • Flawed skin antisepsis • Flawed surgical prophylaxis • Effects of the OR environment (eg, hypothermia) • Break in aseptic technique • Hypothermia or hypoxia • Perioperative blood transfusion • Surgical technique • Hemostasis • Tissue trauma Edmiston et al., 2010 • 1978 – study showed that application of CHG to the skin surface resulted in a greater microbial log reduction and it persisted several hours after application compared with povidone iodine • 1988 – documentation shows that repeat application of CHG 4% was superior to a single shower in reducing staphylococcal skin contamination Edmiston et al., 2010 PRE-INTERVENTION GROUP • 727 patients • Self bathing of povidone iodine night prior to surgery • After 3 months, 3.19% infection rate POST-INTERVENTION GROUP • 737 patients • Self bathing of CHG 2% impregnated polyester cloths night prior to surgery and staff assisted bath on admission to hospital • After 3 months, 1.59% infection rate Edmiston et al., 2010 Overall the evidence is strong in supporting the use of CHG. In the journal article, the authors identify some weakness within the studies they included. For example, in one of the studies the author lists several problematic issues involving study design, implementation, and analysis. Another weakness of this literature review is several studies were included and because of this, there was a lot of pertinent information left out in order to summarize the amount of information. • Observational study conducted to determine LTCS SSI rates and impact of infection control interventions from Oct. 2005-Dec. 2008 • Included use of 2% Chlorhexidine gluconate (CHG) for surgical skin prep and no rinse CHG cloths • Four study periods Riley et. al, 2012 Baseline Period (October, 2005 - March, 2006) SSI rate retrospective identification for comparison Riley et al., 2012 Outbreak Period (April, 2006 – October, 2006) • Obstetrics and gynecology (OBGYN) clinicians noticed an increase in post-LTCS patients returning with SSI in 2006 • Focused on identifying critical control points and analyzing hazards by directly observing LTCS procedures • Labor and delivery (L&D) operating room (OR) walks • Self administered employee survey • • • • • • • Limited personnel traffic during surgery Improved surgical hand scrub Modified surgical skin preparation Changed the timing of antimicrobial prophylaxis Revised L&D OR policies Performed SSI prevention in-services Completed employee competency training Intervention One Period (November, 2006 – September, 2007) • Focused on changing practice and fully implementing all recommendations from outbreak period • Fully implemented recommendations based on the CDC’s SSI prevention guidelines Intervention Two Period (October, 2007 - December, 2008) • Chloroprep, a combination of 2% CHG and 70% isopropyl alcohol (IPA) replaced povidone-iodine for surgical skin prep • Implementation of preoperative CHG skin cleansing program • Scheduled – patient performed night before surgery • Unscheduled – nurse performed as part of pre-surgery prep • Moved into new hospital building • Changed administration time of antibiotic • Nurses in OBGYN clinics educated patients about SSI prevention Evidence in itself was strong based on the reduction of SSIs during the study. However, there were also several limitations to the study: • Implementation of multiple interventions at the same time. Which intervention was successful? • Cost analysis was not studied in depth. • Although patients were instructed to contact their physician for signs and symptoms of infection, no official follow-up was coordinated. • The authors conducted an article review to evaluate if there is a superior intra-operative prep available for open abdominal and general surgery procedures. • The authors concluded that there is no one prep that is superior in all situations. Zinn et al., 2010 • • • • • Povidone-iodine Advantages Excellent gram-positive activity Good gram-negative activity Broad spectrum Moderate rapidly of action Long established as an effective agent • • • • • Chlorhexidine Advantages Excellent gram-positive activity Good gram-negative activity Broad spectrum Moderate rapidly of action Excellent persistent and residual activity Zinn et al., 2010 Povidone- iodine Disadvantages • Minimal persistence and residual activity • Decreased effectiveness in the presence of blood and organic material • Lack of recent empirical evidence Chlorhexidine Disadvantages • Contraindicated for use on eyes, ears, brain and spinal tissue, genitalia, mucus membranes • Inactivity in the presence of saline solution • Drying effect on the skin Zinn et al., 2010 • Only 29 studies were involved in this literature review • Each prep agent has specific advantages and disadvantages. • The study reviewed several prep agents because of the considerations for patient allergies, natural flora, surgical site, and surgeon preference. • The study did not include any research of ChloraPrep • The researchers stated that they did not find adequate information to prove one prep agent used exclusively. • The article was easy to read however lacked specific information or statistical evidence; leaving a lot of unanswered questions. • This was a case controlled study of 29,862 patients over a 3 year period • Only orthopedic, cardiac, neurological, and vascular cases were in the study Thompson & Houston, 2012 • To determine if a regimen of 2% chlorhexidine for 5 days preop along with intra-nasal mupiricin decreases MRSA surgical site infections Thompson & Houston, 2012 • • • • Cardiac 92% decrease Orthopedic 43% decrease Neurology 100% decrease Vascular 52% decrease • Total MRSA SSI reductions from 2006-2008 Thompson & Houston, 2012 • Pre-operative bathing with 2% chlorhexidine and use of mupiricin ointment may be beneficial in reducing MRSA SSI’s • We currently use a variety of products • • • • ChloraPrep w/ tint 4% chlorhexidine solution ChloraPrep SEPP 2% chlorhexidine cloths • Use of chlorhexidine intra-op skin prep when not contraindicated • Appropriate education to patients and staff about use and application • Pre-operative chlorhexidine bathing • Ongoing follow up on post operative infection rate • Edminster, C.E. Jr, Okoli, O., Graham, M.B., Sinski, S., & Seabrook, G.(2010). Evidence for using chlorhexidine gluconate preoperative cleansing to reduce risk of surgical site infection. Association of Perioperative Registered Nurses Journal, 92(5), 509-518. • Riley, M., Suda, D., Tabsh, K., Flood, A., & Pegues, D.(2011). Reduction of surgical site infections in low transverse cesarean section at a university hospital. American Journal of Infection Control, doi:10.1016/j.ajic.2011.12.011 • Thompson, P., Houston, S. (2012). Decreasing methicillin-resistant staphylococcus aureus surgical site infections with chlorhexidine and mupirocin. American journal of infection control, 9(3). • Zinn, J., Jenkins, J., Swofford, V., Harrelson, B., & McCarter, S.(2010). Intraoperative patient skin prep agents: Is there a difference? Association of Perioperative Registered Nurses Journal, 92(6), 662-671. doi:10.1016/j.aorn.2010.07.016 • CMPA Good Practices Guide. 2012. [Surgical Preparation]. Retrieved from http://www.cmpa-acpm.ca • Mayo Healthcare Pty. Ltd. n.d. Interventional Hygiene. Retrieved from http://www.mayohealthcare.com.au/products/Resp_intvH ygiene_skinPrep.htm