rhytmcen
advertisement

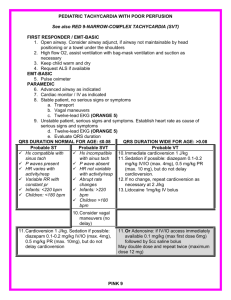
Dysrhythmias and Blocks BKN 1/24/02 How to crack a rhythm What is the atrial rate and what is the source? What is the ventricular rate and what is the source? What is the relationship between the atria and the ventricles? (Who’s in charge here?) Is there conducting system blockade? And after you crack it What is the underlying cause? Is the the rhythm hurting the patient? What should be done? Rules of the road No arrests, you’ve all taken ACLS, you know how to treat VF. Asystole and PEA are dead people “It’s 2 a.m., there’s noone in the place. . .” – PG1 or 2 assigned as senior resident – PG3 assigned assigned as attending No kibbutzing from the crowd until I ok it. Case 1: Dr. Nelson’s Happy New Year 51 y/o M complaining of palpitations Drunk on homemade wine (ETOH = 225) PE unremarkable Intermittent episodes of rapid pulse and pallor with BP 95/60 lasting up to 1/2 minute Rhythm strips follow; not continuous Happy New Year! What to do? At next episode, cardiovert with 50j (YES!) Amiodoarone or Lidocaine Magnesium sulfate 4 gm BAL 5 mg/kg Adenosine 12 mg IVB Leave him alone, we never liked him much anyway and we see a possible end to pimping Happy New Year What’s the rhythm? Is it hurting him? What’s the cause? V tach vs SVT with aberrancy Clinical features Physical EKG Specific QRS patterns Brugada’s Criteria for 4 step quick process – MANY PATIENTS IN VT HAVE NORMAL BP AND MENTATION. DX OF SUSTAINED VT REQUIRES >30 SEC OF RHYTHM Clinical Features Favors V Tach Favors SVT Age > 50 Age<35 Organic Heart Disease None Hx V Tach Hx SVT Physical Exam V Tach SVT Cannon A waves Absent Pulse Variation No variation Variable heart sound No variation EKG V Tach SVT Fusion Beats None AV dissociation P waves precede QRS QRS> .14 sec QRS<.14 sec Extreme LAD (<-30) Normal Axis No response to vagal Vagal slows or stops Specific QRS patterns V tach SVT V1: R, qR. RS V1: RsR’ V6: S, rS, qR V6: qRs Identical to previous Identical to previous VT SVT Concordance of QRS in V1 – V6 Brugada’s criteria: any Yes = VT 1. Absence of RS complex in all precordial? 2. R to S interval >100 ms in one precordial? 3. Atrioventricular Dissociation? 4. Morphology criteria for VT present in both leads V1-2 and V6? Is there anything wrong with. . .? Cardioversion if in sustianed wide complex tachycardia? Go ahead if patient metastable or worse. Be sure you reassure the patient that it doesn’t mean he’s dieing (if he’s not) Adenosine? Probably safe, has a very short 1/2 life Holiday Heart Supraventricular tachycardias (most often Atrial Fibrillation) Transient Ventricular Tachycardia Seen in chronic alcoholics on a binge Alcoholic Heart Disease Holiday Heart Alcoholic Cardiomyopathy Acute intoxication has cardiodepressant, vasodilatory and diuretic effects even in those with a normal heart (keep in mind for that drunk mildly hypotensive trauma victim) In those with coronary disease, >2 oz can decrease exercise tolerance and increase ST depression after angina Treating Dr. Nelson Abstinence will lead to conversion to sinus Do not treat unless hemodynamically unstable Case 2: Aunt Jane ain’t right 76 y/o F noted to be increasingly confused by family over last several days Her Doctor is not available Family doesn’t know details of medical history Patient complains of being weak Aunt Jane’s physical Elderly female, oriented x 1, mod respiratory distress BP 80/p, P 150, T 97 R, RR 24, SaO2 88% RA JVD, Rales in bases ECG follows Case 2: Aunt Jane ain’t right What’s the rhythm? What’s the underlying cause? Is it hurting her? What to do? What’s the rhythm? Atrial rate 180, probably sinus Ventricular rate 150, alternates between ventricles (LBBB pattern, RBBB pattern) Complete AV dissociation Apparent complete heart block Complete rhythm diagnosis: atrial tachycardia, bi- directional V Tach, AV dissociation Aunt Jane’s rhythm problems PAT with AVB and Bidirectional V Tach are both almost pathognomonic of Digitalis toxicity Is it hurting her? Clearly yes, we probably need to treat while waiting for the Fab frags to arrive, be administered and take effect What to do? Cardiovert her? Overdrive pacing? Diurese her? Use antidysrhythmics? Cardiovert? Cardioversion generally considered contraindicated for Dig toxic rhythms. The heart is irritable due to increased catecholamine sensitivity Fear cardioversion to refractory VF, VT and asystole Most of that literature is very old and is talking about cardioverting AF. Applicability to VT unclear. Is Aunt Jane an exception because she’s so sick we don’t think we’ll make her worse? Overdrive Pacing? Transvenous pacing in dig toxicitycarries same dangers as cardioversion (Induces ventricular dysrhymias, mortality 13%) Transthoracic pacing may be safer, but the pacer would need to be capable of higher rates than the intrinsic rhythm Diuresis? Most patients in chronic dig toxicity are already on diuretics and hypokalemic. Hypokalemia worsens Dig toxicity.Must check K and supplement as necessary if going to diurese Antidysrhythmics Most antidysrhythmics are contraindicated in Dig toxicity Magnesium indicated for dig induced tachydysrhythmias. 1-2 gm over 2 minutes then 1-2 gm/hr Lidocaine or phenytoin are considered safest Anti digitalis Fab fragments Expensive Indicated for severe ventricular dysrhythmias, atropine refractory progessive hemodynamically sig bradydysrhythmias, severe hyperkalemia, rapidly progressive dysrhythmias, cardiotoxic coingestants, plant cardiac glycosides + severe dysrhythmias, high levels plus any of the above Case #3: Bloody Awful A 52 yo male presents with weakness, melena, and palpitations. H/O heavy ETOH intake chronically. BP 80-100 P fast and weak, monitor heart rate 205, SaO2 = 78%, patient stuporous, no ETOH odor Heart: very fast Abdomen soft, stool black, NG grossly bloody Bloody awful Initial lab: Glucometer = 500 ABGs =7.25/20/55, BE = -15, Hgb = 7, Wassup? What’s the rhythm? What’s the underlying cause? Do we need more info? Is it hurting him? Wassup? Rhythm Atrial fibrillation with rapid ventricular response Underlying causes: hypovolemic shock, alcoholic heart disease, possible DKA Addl info: CXR borderline cardiomegaly without failure Is it hurting him? In this clinical scenario, of course. Combination of rate, blood loss, base deficit, anemia suggest that cardiac arrest is imminent What to do? Define possible strategies What to do? Cardiovert? (electrically or chemically) Slow Vent Response? Correct hypovolemia, anemia, DKA and hope he gets better from this alone? Cardioversion Pro: rapid return to a rate allowing ventricular filling, adequate cardiac output Con: In presence of chronic AF, atrial thrombus may exist. Cardioversion may lead to arterial embolism (stroke, mesenteric infarct, etc) Do we think this is acute or chronic AF? Acute or chronic? The rate and the clinical scenario suggests acute, but you never really know. How to do it? Electrical or chemical? Electrical or Chemical Electrical is quick and except in the dig toxic is unlikely to have side effects. However, the underlying condition leading to AF is unchanged. The heart may go right back into the rhythm Chemical conversion is slower, but leads to conditions more likely to allow permanent conversion. However the drugs used (class 1a and 3) can all cause major dysrhythmias and cardiodepression. Digoxin is slower but won’t cause cardiodepression Summary of recs (most pts hemodynamically stable) For acute AF in patient without failure or cardiomyopathy: use class 3 agent (Ibutilide has highest success rate and quickest action, but can cause dysrhythmias after single dose) Chronic AF usually with cardiomyopathy: rate control, anticoagulation for 3 weeks (or TEE) followed by electrical cardioversion Slow ventricular rate Calcium channel blockers are preferred for the patient in absence of ventricular dysfunction. Digoxin for the hemodynamically unstable may take longer to have effect. Note reading the studies, it appears that the differentiation between “rate-control” and “cardioversion” is probably not real Correct conditions: always MI, Ischemia, valvular disease, pericarditis, hyperthyroidism, SSS, contusion, holiday, idiopathic, hypertensive heart, cardiomyopathy, cardiac surgery, catecholamine excess, PE, CHF, WPW For this patient It was felt that arrest was imminent and acute AF was most likely, The patient was cardioverted with 200 j. He converted to sinus and within 3 seconds reverted to AF Class 1a, 3, and Ca blockers were rejected because of patient’s probable cardiomyopathy and hypotension/shock For this patient O2 and fluid resuscitation were started Type specific blood was ordered Digoxin 0.5 mg was given IV Within 5 minutes the patient converted spontaneously to sinus tach. Blood and octriatide started, Pt admitted to ICU, GI consulted. Case 4: I fainted (4 p.m.) 14 y/o female brought by mother and teacher. Child reportedly was in Biology lab, dissecting a frog which upset her The biology teacher reports she fell to the ground suddenly, had few jerks of extremities, and awoke, fully concious in about a minute. Child has no memory of falling and had no prodromal sympotoms I fainted Child is awake and alert VS are normal, glucometer is 110, SaO2=98% Complete neuro exam is normal General physical exam is normal Should we quit? If not, what would you like to do? I might quit, but You could easily argue for a b-hcg, bmp, cbc, and a CT/EEG to r/o pregnancy/ectopic, anemia, seizure disorder and subarachnoid bleed An ECG is harder to justify, but this is a cardiology lecture, so: What to do? Is there a problem? What will you recommend? Course Child is admitted to telemetry, Cardiology consult is planned for the AM The code team is called at 2 am as the child has arrested Rhythm strip follows What to do? What’s the rhythm? What’s the immediate treatment? In the short term? In the long term? Would it have been different if the child had been taking erythromicin? Long QT syndrome Adrenergic dependent or pause dependent Both can cause sudden death from Polymorphic V Tach Pause dependent requires slowing of heart, is generally acquired Adrenergic requires tachycardia and is mostly congenital (thus the more dangerous) Causes of long QT: pause dep Class 1a, 3 antidysrhythmics Psych drugs: TCA, phenothiazines Antibiotics: erythromicin, ampicillin, pentamidine Antihistamines: terfenidine, astemizole misc: cocaine, organophosphates, cisapride, Electrolytes disorders: lo K, lo Ca, Lo Mg Severe ischemia Normal heart/ no drugs Causes of Long QT: adrenergic Congenital – Jervell and Lange-Nielsen (deafness, recessive) – Romano-Ward (normal hearing, dominant) – Sporadic (normal hearing, no family tendency) – Mitral Valve Prolapse Acquired – Cerebrovascular disease (particularly SAH) – Autonomic surgery (radical neck, CEA, truncal vagotomy) Immediate treatment for PMVT Cardioversion in same manner as monomorphic VT Intermediate treatment Pause dependent – stop offending medication – Mg infusion – Overdrive pacing or isoproterenol drip to rate of 100 to 120 bpm – correct electrolytes Adrenergic dependent – Beta blockade Long term treatment-refractory cases Adrenergic dependent – left cervicosympathectomy – cardiac pacing with maximum beta blockade – implantable defibrillator Pause dependent – permanent pacer – implantable defibrillator Case 5: Weak and Dizzy 70 y/o women presents with occasional episodes of near syncope PMH: HTN, angina PE: VS nl, CNS nl. CVS: S4, BMP, CBC nl ECG follows What to do Diagnosis treatment Weak and dizzy Sinus arrest, intermittent ventricular escape rhythm, incomplete AV dissociation Treatment: trans thoracic pacing, EPS referral While hooking up the pacer, the following strips are collected Weak and Dizzy What additional diagnoses added? Any additional therapy? Weak and dizzy Brady-tachycardia syndrome, an advanced manifestation of Sick Sinus syndrome May have to use antidysrhythmics to slow rate. This increases block and necessitates a permanent pacer Case 6: My heart is running away 30 y/o m presents with rapid heart beat, dyspnea and weakness. Has had similar episodes in past but no treatment PE: Pulse rapid, weak. BP 60/p, monitor heart rate 220 ECG follows What’s next? Rhythym is Wolfe-Parkinson-White syndrome with Atrial Fibrillation What’s next Cardioversion gives following rhythm change. Now what? WPW with alternating conduction Orthodromic tachycardia when conduction down AV node and reciprocates up Bundle of Kent Antidromic tachycardia when conduction down Bundle of Kent and back up AV node WPW with tachydysrhythmias Antidromic regular tachycardia or any irregular tachycardia, regardless of QRS duration at high risk for V Fib All drugs that block the AV node are contraindicated as they may increase rate of conduction through the accessory pathway, accelerating rate of dysrhythmia leading to V Fib No-Nos No Digitalis, Ca channel Blockers, Beta- blockers, or adenosine Regimen of choice: cardioversion if unstable, procainamide, referral for catheter radioablation of pathway Second line drugs: other 1a and 1c Case 7: I need a doctor for Med Control 56 y/o had a syncopal episode, feels well now, wants to refuse therapy The paramedics fax this ECG, what do you think? Not so fast buddy Patient has First degree AV block, RBBB and intermittent LAHB Consider this a “Partial Trifasicular Blcok” Trifasicular Block When RBBB, LAHB and LPHB present one sees CHB with VER (can be either from right or left ventricle). But there are five fasicles: His bundle, Right Bundle, Left Bundle, Left Anterior, Left Posterior. If incomplete TFB can be difficult to differentiate from surface ECG Refer all patients with BBB, BFB or HB with any degree of AVB for EPS Admit all symptomatic patients with above findings Another example Quickie no 1 83 yo bedridden male found to be less responsive than usual FMS finds in V tach with pulse, under med control gives lido with conversion, during transport BVM ventilated, aspirates. On hospital arrival RSI performed, SaO2 improves from 60% to 95%. % minute later V tach recurs, pt cardioverted. Now what meds? Quickie #1 Pt given lidocaine boluses 100 and 50 while procainamide loading dose prepared While being loaded, qrs changes, here’s the rhythm strip, what’s going on? Quickie #1 Sinus mechanism with wide complex, suggestion of j point elevation. Given the clinical situation (elderly, bedridden). Patient may be hypothermic. Check a temp, If temp below 94 no more carediodepressant antidysrhythmics. Warm the patient (passive or active internal, not active external) Quickie #2 73 y/o male, no symptoms What’s the ECG diagnosis? Quickic #2 Alternating RBBB and LBBB. What looks like a second P on half the beats is really the initial deflection of a RBBB Dig toxic rhythm? Needs EPS? Quickie #3 58 y/o female feels weak No PMH, doesn’t like Doctors Glucometer 450 ECG follows: findings? Probable cause? RX? Quickie #3 ECG findings: Diffuse Intraventricular block (RBBB with LAHB?), flattened p waves. Beginning to look like a sine wave Probable cause: Hyperkalemia sec to renal failure Immediate Rx: CaCl2 10 ml slow push, Insulin 10 units (don’t need D50 since hyperglycemic), Kayexalate Quickie #4 58 y/o in 1 vehicle accident on Saturday Night, smells of ETOH, BP 80/p, patient comatose: PE, FAST, Xrays, Head CT What are the ECG findings? What should you do to confirm the probable diagnosis? If confirmed, what should be done now? Quickie #4 ECG findings: Atrial flutter-fib advanced AV block, diffuse intraventricular block, PVCs, Osborne waves Take a rectal temp Do nothing but passive rewarming, hypothermia <90 f explains all clinical and ECG findings Causes of Diffuse Intraventricular Block MI Severe Hypertensive Heart Disease Cardiomyopathy Hyperkalemia Elderly (senile fibroelastosis?) Hypothermia Quickie #5 48 y/o male feels dizzy and weak. BP 90/p ECG findings? Probable cause? Rx? Quickie #5 ECG findings: Multifocal atrial tachycardia, aberrant conduction Cor pulmonale with hypoxia, prescribed beta agonists or methylxanthines may be contributing, may be dig toxic Correct hypoxia, withdraw offending agents, electrical cardioveriosn unlikely to be successful until underlying condition treated Rate control, if needed by Ca channel blockers, Mg second line Dig toxicity treated in usual manner Quickie #6 47 y/o male with idiopathic cardiomyopathy What’s the rhythm? Quickie #6 Wide complex tachycardia, confirmed as V tach by AV dissociation by p waves before the 4th and 13th QRS and after the 5th Quickie #7 80 y/o F, confused, BP 80/p, pulse 167 ECG diagnosis? What can you do? Quickie #7 Dx: Pacemaker mediated tachycardia and malpositioned electrode (RBBB pattern suggests anode in Left Ventricle Try to convert to fixed rate output 70 bpm with magnet Overdrive it with transthoracic and try to slow it Open the pocket and disconnect the wires or cut them Find out where the tip is: Left ventricle? Pulmonary outflow track? Pericardial sac? Summary: immediate therapy If it’s too slow, pace it If it’s too fast, cardiovert it Correct underlying problems: ischemia, electrolytes, drug toxicities, etc All antidysrhythmics are poisons, some are useful poisons Understand special cases: Dig toxicity, WPW with antidromic conduction, PMVT Summary: long term Everybody with a significant dysrhythmia deserves a EPS consult. – Most recurrent, hemodynamically important SVTs should be treated with catheter radioablation – Significant bradycardias, not responding to Bblocker withdrawal need a pacemaker – V Tach and fib get mapping and ventriculotomy or drugs plus defibrillator