Malignant Mesothelioma Audit
advertisement

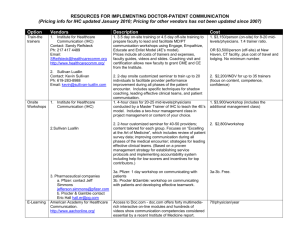
April 2014 Dr J King Dr K Syred 90% mesotheliomas are linked to asbestos exposure May be eligible for compensation 3 yr survival rate 8% Subtype related to prognosis and different treatment options ◦ Epithelioid 1yr survival 52% ◦ Sarcomatoid 1 yr survival 13% Correlation of tissue diagnosis with clinical and radiology IHC: ◦ Panel 1: TTF-1, CEA, calretinin, CK5, D240, WT-1, MOC31 ◦ Panel 2: MNF116, CD15, CK7, CK20 Ihc Reactive Malignant -/+ + Strong membranous Desmin + - p53 - + EMA Identify practice within our department ◦ ◦ ◦ ◦ Typing Assess what ihc has been performed Determine any improvements in diagnosis Report quality Reviewed mesothelioma reports in the last 9 months (1/1/14 – 30/9/14) Identify further work done Possibly devise an improved panel of markers make diagnosis more efficient and cost saving ‘6.4 Pathological Histological type should be stated (epithelioid, biphasic, sarcomatoid (desmoplastic variant if present). Given the need for ancillary investigations to make the diagnosis, the immunohistochemistry panel used should be documented, this being at least two ‘mesothelium-associated’ markers and two ‘epithelium-associated’ markers for epithelioid and biphasic tumours (discussed in section 5). For sarcomatoid variants, due to the wide differential diagnosis, the full repertoire of antibodies used should be listed.’ ‘For pleural mesothelioma-like tumours with an epithelial component, it is recommended that immunolabelling for both calretinin and TTF-1 is routinely carried out.’ ‘As with biopsies, cytological findings should be correlated with the clinical and imaging findings to establish whether the available cytological material is sufficient to render a specific diagnosis or a clinically relevant differential diagnosis. If a pleural cytology specimen is positive or suspicious for malignancy, and there is no other specimen, then material should undergo the same ancillary investigations as for biopsies in terms of the differential diagnosis, which ideally is via a cell pellet for histology as this allows preservation of residual material. Identification of an epithelial phenotype will allow a definitive diagnosis of metastatic carcinoma. Identification of a mesothelial phenotype will allow further management decisions in terms of a definitive diagnosis of mesothelioma or further sampling, dependent on the clinical scenario’ 1. 2. 3. 4. All diagnoses of mesothelioma should be typed. Where immunohistochemistry is performed, there should be a panel including 2 mesothelial and 2 epithelial markers. If an epithelioid subtype, caltretinin and TTF-1 should be performed Immunohistochemistry should be performed on tissue rather than pleural fluid when available. Search on i-lab ◦ ◦ ◦ ◦ M-90503 M-90513 M-90523 M-90533 – – – – mesothelioma, NOS fibrous mesothelioma, NOS epithelioid mesothelioma, NOS biphasic mesothelioma, NOS 1/1/14 – 30/9/14 From the list each report looked up on i-lab Data in-putted into spread sheet Lab no What procedure was done to obtain a diagnosis Any previous relevant investigations Any immunohistochemistry performed on the procedure and if so what was ordered (the SPLI function was used to identify the immunohistochemical stains performed as not all of them were mentioned in the report. Where mentioned in the report, the result (positive or negative) was recorded). It was noted if there was pleural fluid taken at the same time as any biopsy. If there was mention of a pleural fluid on the biopsy form Diagnosis of mesothelioma if pleural or peritoneal in during the time period stated above. Previous results e.g. any previous pleural fluids sampled in previous years were also included in this audit. Outside cases for review at the MDT eg. from Truro. Cases that are coded incorrectly. LN biopsy for metastatic malignant mesothelioma PM histology as not all of the PMs would have been picked Total 31 biopsies performed ◦ 3 excluded 1outside case 2 adenocarcinomas coded incorrectly Remaining 28 ◦ 26 pleural bx - 20 had cytology at the same time ◦ 2 omental bx ◦ 27 had ihc 1 did not as it was being performed on the fluid ◦ 1 had ihc on both bx and fluid Accompanying cytology ◦ 8/20 (36%) malignant or suspicious of malignancy ◦ 12/20 no malignant cells seen ◦ 6 cytology forms mentioned bx taken 7 cases bx only taken ◦ 1 recurrent case with prev diagnosis 3 yrs ago ◦ 1 had 2 previous pleural fluids – blood only and nmcs ◦ 5 did not have any previous procedure 2 cases diagnosed on pleural fluid alone 24/28 (86%) mesotheliomas diagnosed on tissue were subtyped. Type No Epithelioid malignancy 2 Epithelioid malignant mesothelioma 17 Epithelioid and sarcomatous malignant mesothelioma 1 Biphasic malignant mesothelioma 3 Malignant mesothelioma 3 Recurrent malignant mesothelioma 1 Sarcomatoid malignant mesothelioma 1 13/29 cytology cases were suspicious/ malignant. only 7 were classed as mesothelioma and only 2 were subtyped. 2/13 = 15% Report No Favour malignancy / malignancy strongly suspected 4 Atypical epithelioid cells highly suspicious of malignancy 1 Malignant 1 Favour / suggestive / suspicious of mesothelioma 4 Mesothelioma 1 Epithelioid meosthelioma 2 biopsy 27 Accompanying cytology 2 Cytology alone 2 Previous cytology 4 Total 35 39 different immuno-stains were ordered Total of 286 ihc orders Average = 8 per case Mucin stains = 10 0 ABDPAS DPAS s100 CD34 CD31 Hepar 1 PSA ER CDX 2 CK20 TTF-1 p63 thrombomod… pankeratin Cam5.2 CEA desmin BerEp4 100 MOC31 p53 D240 CK7 WT-1 calretinin MNF116 EMA CK5 vimentin CK19 Ae1/3 % number of ihc and special stains positive in malignant mesothelioma 90 80 70 60 50 40 30 20 10 vimentin CK19 Ae1/3 CK5 EMA MNF116 calretinin WT-1 CK7 D240 p53 MOC31 BerEp4 desmin CEA ABDPAS DPAS s100 CD34 CD31 Hepar 1 PSA ER CDX 2 CK20 TTF-1 p63 thrombomodulin pankeratin Cam5.2 % number of ihc and special stains negative in malignant mesothelioma 100 90 80 70 60 50 40 30 20 10 0 Meso vs adeno panels Ihc Total Pos bx Pos cytol Neg bx Neg cytol Panel 1 TTF-1 24 0 0 19 4 CEA 18 1 0 14 3 MOC-31 24 5 3 12 3 Calretini n 33 20 7 3 0 CK5 26 19 5 1 0 D240 7 3 1 3 0 WT1 26 18 2 3 0 CKMNF1 16 12 10 0 1 0 CD15 0 0 0 0 0 CK7 9 5 1 2 0 CK20 8 0 0 5 1 Panel 2 Mesothelial markers % positive CK5 96% (27/28) Calretinin 90% (29/32) WT-1 88% (22/25) Epithelial markers % positive CEA 6% (1/18) BerEp4 29% (7/24) MOC31 35% (8/23) TTF1 0% (0/23) 30/35 (86%) had 2 epithelial and 2 meso markers Remaining 5: ◦ One had reactive panel ◦ 4 had both an epithelial and mesothelial marker, some with 2 of one but not 2 of both 23 of mesotheliomas typed as epithelioid 15/23 (65%) had both calretinin and TTF-1 performed One had reactive panel The remaining did not have TTF-1 2 were omental bx and may not need TTF-1 Ihc performed on 27 of the biopsies 1 did not have ihc as it was requested on the cytology (commented on in the report) Only 1 patient had ihc on both biopsy and cytology Standard 1: 86% tissue and 15% cytology subtyped Standard 2: 86% had 2 mesothelial and 2 epithelial markers Standard 3: 65% epithelioid mesotheliomas had calretinin and TTF-1 Standard 4: 1 had ihc on fluid rather than bx and 1 had ihc on both New mesothelioma IHC panel ◦ CK5 ◦ Calretinin ◦ WT-1 CEA BerEp4 Moc31 TTF-1 Proforma to guide reporting biopsies and cytology ◦ Subtype ◦ List of ihc http://www.hscic.gov.uk/media/15038/Meso theliomaaudit/pdf/EMBARGOEDTO120914_NLCA_Mes o_Report_final.pdf Standards and datasets for reporting cancers. The dataset for the histological reporting of mesothelioma. RCPath guidelines