Introduction to ALS
advertisement

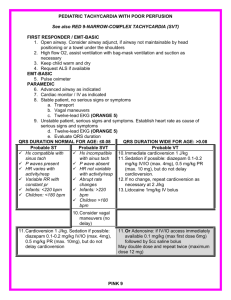
Introduction to ALS Sir Sandford Fleming Outline Work Environment Scope of Practice Training Equipment Procedures How PCP/ACP Combos work What will be expected of you? Work Environment Many services are up to 40% ALS Presents different challenges – – – – – Bags are different Dispatched differently Crew configuration different (>age) Expectations for level of care higher Closer scrutiny Potentially more stress for the crew Combined care (different attendant/driver roles) Work Environment Legislation – Narcotics Check sheets Signatures DMA – – Risk’s/benefit Higher chance something will go much better or much worse Scope of Practice Lots more drugs Lots more heavy things Special airway equipment Special features on monitor – – – Manual defib Cardioversion Pacing (transcutaneous) Scope of Practice Manual Defibrillation, Pacing and Cardioversion Advanced Airway LMA’s , Lited Stylets BTLS, ACLS ,PALS IV Therapy ALS Drugs plus Symptom Relief, Versed, Fentanyl Activated Charcoal CXR Interp Pentaspan Difficult Airway Algorithm Need ETT Attempt #1 -Without sedation(crash) or nasal ETT Attempt #2- Midazolam 0.05 mg/kg Fentanyl 1-1.5 mcg/kg Attempt #3(or RSI Direct) Lidocaine, (atropine) with midazolam and fentanyl (see above) and succinylcholine 1-1.5 mg/kg Backup- Laryngeal Mask Airway, Lighted Stylet, Surgical Airway Training Time lines – roughly 1 year for ALS Didactic –classroom time Clinical –practice in a controlled setting – – – – – OR ER MOP/SOP OBS/PEDS/ICU Other (Burn Unit, HSC IV Team) Preceptorship/Consolidation Where it should all come together With a designated preceptor Gradual transition to full care Equipment Airway– – – Basic airway Laryngoscope plus ETT for Intubation Rescue Devices –advanced airway Lighted stylet LMA – Surgical –Seldinger vs Quik Trach Bougie Procedures Cardioversion Pacing Sedation Vagal and CSM Manual Defibrillation IV Bolus and IV medication Other routes (PR,IN,IM,ETT,IO) Intubation Advanced airway Needle decompression IO Thrombolytics VAD Central access Airway CONTROL THE AIRWAY Airway Management Decision Process (Judge how aggressive you need to be.) -Time/Distance -Personnel -Equipment -Other Considerations? CONTROL THE AIRWAY “Evaluate for signs of difficult intubation” (this may help in your decision as well) -Obesity -Small body habitus -Small jaw -Large teeth -Burns -Trauma -Anaphylaxis -Stridor CONTROL THE AIRWAY The PCP vs. ACP airway decision may not be based on one single factor, but rather based on an overall assessment of many factors. CONTROL THE AIRWAY Pre-Intubation -Prepare Equipment -Hyper-oxygenate CONTROL THE AIRWAY Orotracheal Intubation Procedure Sweep Left and Look CONTROL THE AIRWAY Find Your Landmarks Backward, Upward, Right Pressure (B.U.R.P.) CONTROL THE AIRWAY Find Your Landmarks CONTROL THE AIRWAY Find Your Landmarks It may not be perfect! CONTROL THE AIRWAY Find Your Landmarks CONTROL THE AIRWAY Readjusting with Cricoid Pressure CONTROL THE AIRWAY Common Provider Mistakes *Making a difficult intubation more difficult *Rushing *Poor equipment preparation *Suction (lack there of) CONTROL THE AIRWAY What is your back-up plan today? prolonged BVM… another provider… a smaller tube… better lighting… additional suctioning… CONTROL THE AIRWAY Helpful Adjuncts Gum Elastic Bougie CONTROL THE AIRWAY Helpful Adjuncts Lighted Stylette CONTROL THE AIRWAY Nasotracheal Intubation Indications: “Patient still breathing but in respiratory failure and in whom oral intubation is impossible or difficult.” CONTROL THE AIRWAY Nasotracheal Intubation Contraindications: -Apnea -Resistance in the nares -Blood clotting or anticoagulation problems -Basilar Skull Fx (?) STEP 4. CONTROL THE AIRWAY Nasotracheal Intubation Technique: -Prepare patient and nostril -Prepare tube -Insert on inspiration -Take your time Complications: -Bleeding . CONFIRM THE AIRWAY Intubation Confirmation Good, Better, Best Traditional Technology Based • Direct Visualization • ETCO2 (monitor) • EDD (bulb) • Lung Sounds • Colormetric (cap) • Tube Condensation • Pulse Ox change SECURE THE AIRWAY Secure Your Tube Good, Better, Best Tape Improvised devices Commercial devices Immobilization (?) ALTERNATIVES TO ETI Laryngeal Mask Airway Developed in 1981 at the Royal London Hospital By Dr Archie Brain STEP 7. ALTERNATIVES TO ETI Laryngeal Mask Airway Indications: -When definitive airway management cannot be obtained. (ETT) Not a substitute for definitive airway management ALTERNATIVES TO ETI Laryngeal Mask Airway Contraindication/Limitations: -Obesity -Non-secure -Size based -Not a med route ALTERNATIVES TO ETI Laryngeal Mask Airway Weight Based Sizing <5kg = Size 1 5-10 kg = Size 2 20-30 kg = Size 2.5 Small Adult= Size 3 Average Adult = Size 4 Large Adult = Size 5 ALTERNATIVES TO ETI Laryngeal Mask Airway Average Adult Woman = 4 Average Adult Male = 5 *If in doubt, check the LMA ALTERNATIVES TO ETI Laryngeal Mask Airway Procedure: -Hyper oxygenate -Check cuff -Lubricate posterior cuff -Head in neutral or slightly flexed position -Insert following hard palate (use index finger to guide) -Stop when met with resistance -Let go and inflate cuff (visualize “pop”) -Confirm and secure ALTERNATIVES TO ETI Laryngeal Mask Airway Air volume is variable depending on cuff size and individual patient anatomy General Guideline: Size 1 = 4 ml Size 2 = 10 ml Size 2.5 = 14 ml Size 3 = 20 ml Size 4 = 30 ml Size 5 = 40 ml ALTERNATIVES TO ETI Laryngeal Mask Airway Common Provider Problems: -Failure to seat properly -Sizing difficulties -Aspiration King Airway King Airway Why – – – Unconscious / unresponsive patients without gag reflex Blind insertion technique Alternative to E.T.T. Known Issues – – – – Obtaining proper seal / placement Is NOT a medication route for Endotracheal drugs Multiple sizes, based on height, also multiple cuff volumes Contraindications Responsive patients with an intact gag reflex. Patients with known esophageal disease. Patients who have ingested caustic substances. User Tip The key to insertion is to get the distal tip of King Airway around the corner in the posterior pharynx, under the base of the tongue. Experience has indicated that the lateral approach, in conjunction with a chin lift, facilitates the placement of the King Airway. Alternatively, a laryngoscope or tongue depressor can be used to lift the tongue anteriorly to allow easy advancement of the airway into place. Insertion #1 Insertion #2 Insertion #3 As the King Airway is advanced around the corner in the posterior pharynx, it is important that the tip of the device be maintained at the midline. If the tip is placed or deflected laterally, it may enter into the piriform fossa and the tube will appear to bounce back upon full insertion and release. Keeping the tip at the midline assures that the distal tip is properly placed in the upper esophagus. Insertion #4 Insertion #5 Air Volume Required for Cuff Inflation: – Size #3: 55 ml – Size #4: 70 ml – Size #5: 80 ml Insertion #6 Attach Bag While gently bagging, simultaneously withdraw the King Airway until ventilation is easy and free-flowing. Can the King tube device be used for PPV? Yes, in unresponsive non breathing pts Is there an optimal head position for insertion? – Sniffing position, but the head can be in neutral position. – For obese patient’s, elevation of the shoulders & upper back should be considered. How long can the King tube be left in place? – Up to 8 hours. For longer procedures it is important to monitor& limit cuff pressure to 60 cm H20 or less. If my patient needs to be on a mechanical ventilator, do I need to replace the tube? – Due to the King tube’s improved ventilatory seal, it is less frequent that the tube needs to be exchanged compared to other supraglottic airways. Can a laryngoscope be used? – Yes, but it is not routinely used. It may be used by the inexperienced user, or difficult airway. What volume of pressure is needed to properly inflate the cuffs? – The least amount needed to create a seal at the desired ventilatory pressures. Each tube size is different What reference point for the centimeter depth markings on the tubes? – The cm markings indicate the distance from the distal ventilatory opening. The markings serve as a visual reference after placement and can be used to document insertion depth. SURGICAL AIRWAYS Indications -Obstruction -Facial Trauma -Intubation or other alternatives impossible -Trismus (clenching) ->8 years old (for open procedures) LAST RESORT! SURGICAL AIRWAYS -Vertical Incision over membrane -Pierce membrane in horizontal plane -Open and spread to insert 4.0 or 5.0 tube -Secure tube in place and ventilate SURGICAL AIRWAYS Needle Cricothyrotomy Needle Procedure: -Identify Cricothyroid membrane -Pierce at 45° angle -Place catheter or styllette -Advance dilator per manufacturer’s recommendation SURGICAL AIRWAYS Commercial Needle Cricothyrotomy Devices Quick Trach Pertrach WHY AN ALGORITHM? 1. Step by step process in order 2. Start simple and work up 3. Alternatives 4. Be sure 5. Get it done Procedure for Intubation Preoxygenate with 100% (may not need to bag) Prepare equipment (SLOPES-M) Hyperextend –Sniffing position Insert larygoscope into R sweep tongue to left Look for view Insert ETT to 1-3 cm beyond cords Withdraw largy Remove stylet inflate cuff with 5-8 cc air Auscultate neck, chest x 4 Secure ETT Document cm marking and reevaluate often How you can help as PCP (PRN) Prepare equipment Preoxygenate patient BURP (backwards upwards and to the right pressure-thyroid cartilege mvmt) Cric pressure Remove styet when asked Inflate balloon Secure ETT Ventilate patient Cricoid pressure Only when asked to Know your landmarks Burp –backwards upwards and to the right (pressure) Monitor/Defibrillator LP 12/Zoll has pacing Cardioversion 12 lead NIBP SpO2 ETCo2 (mainstream) detection Manual defibrillation Symptomatic Patients get treated electrically Chest pain Shortness of breath Pulmonary edema Hypotension Diaphoresis Decreased LOA Vagal Manuvers/CSM For stable patients with signs of clinically significant tachy rhythms CSM “Fake” the baroreceptors into thinking BP is too high so slows HR down Vagal manuvers- increase ITP to see if can stimulate a vagal response Patients <70 or with no bruits in carotid arteries Synchronized Cardioversion Unstable tachydysrhythmias Pad placement Synchronize the monitor Sedation, anaelgisics, amnestics Symptomatic Tachyarrhythmias •Chest pain •Hypotension •Syncope •Diaphoresis •Shortness of breath •Pulmonary edema •Altered LOC Signs & symptoms Experience and judgment What Does the “SYNC” Button Do? Tags the R waves Timing – refractory periods Do NOT want to cardiovert at this time! Iatrogenic R on T - Cardioversion Cardiac arrest Always double check Automatic ‘sync’ shutoff Advanced Care Directive - VT with Pulse ATTEMPT PATCH IMMEDIATELY O2 via NRB mask / Intubate PRN IV access Bolus 500 cc NS Lidocaine 1.5 mg/Kg IV Synchronized cardioversion Monophasic 100J Synchronized cardioversion Monophasic 200J Advanced Care Directive - VT with Pulse Patient Symptomatic? Sedate PRN ATTEMPT TO PATCH Synchronized cardioversion Monophasic 200J or Synchronized cardioversion Monophasic 360J PATCH IF RETURN OF NORMAL RHYTHM Atrial Flutter Atrial Fibrillation Synchronized cardioversion 50J Synchronized cardioversion 100J Synchronized cardioversion 100J Synchronized cardioversion 200J REATTEMPT TO PATCH REATTEMPT TO PATCH Synchronized cardioversion 200J Synchronized cardioversion 300J Synchronized cardioversion 300J Synchronized cardioversion 360J Synchronized cardioversion 360J Considerations Inform bystanders Skin irritation/burns Arching of current Adjust ECG size EVERYONE CLEAR! Transcutaneous Pacing Symptomatic bradycardias Over-ride pacing Quickly available Standby pacing Sedation, analgesics, amnestics Contraindications Severe hypothermia Cardiac arrest > 20 minutes Open chest wounds Flail chest Procedure for Pacing Explain to patient O2 & IV therapy Sedate – BHP Pad placement Turn “pacer” on Set HR between 6080 Increase mA capture Add 10 mA - safe zone Defibrillation-Manual ALS algorithm for Vfib/Vtach pulseless CPR Defibrillate Monophasic 200,300,360 J or Biphasic INTUBATE / IV ACCESS 1.0 mg Epi (1:10,000) IV or 2.0 mg Epi ETT repeat q 3-5 minutes Defibrillate Monophasic 360 J x3 or Biphasic 200J x3 1.5 mg/Kg LIDOCAINE IV or 3.0 mg/Kg ETT Defibrillate Monophasic 360 J x3 or Biphasic 200J x3 Remember in manual mode, the machine will shock regardless of what the rhythm on the monitor is! Drugs Carried by ALS NTG ASA Ventolin (MDI,ETT,Neb) Glucagon Epinephrine 1:1000,1:10000 Atropine Lidocaine (preload and spray Lasix Adenosine Dopamine Midazolam Diazepam Fentanyl Morphine D50W Na Bicarbonate Otrivin Gravol Treating patients -Differences Can give NTG if no prior use Increased selection of things to do Also increased responsibility Increased accountability Increased $$$ too!