Timby: Fundamental Nursing Skills and Concepts
advertisement

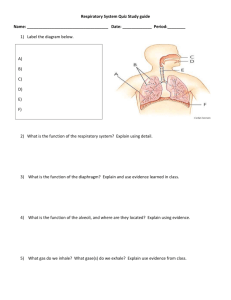
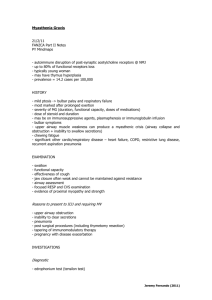
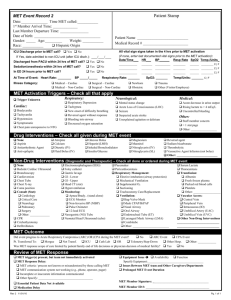
Pulmonary Nursing Chapter 21 Oxygenation Oxygenation • Oxygen: measures approximately 21% in the Earth’s atmosphere • Each cell of the human body uses oxygen to metabolize nutrients and produce energy • Without oxygen, cell death occurs rapidly Anatomy and Physiology of Breathing • Inspiration and expiration • Ventilation: movement of air in and out of lungs; facilitates respiration • Respiration: exchange of oxygen and carbon dioxide Anatomy and Physiology of Breathing (cont’d) • External and internal respiration • External respiration takes place at most distal point in airway: between the alveolar-capillary membranes • Internal respiration occurs at the cellular level between hemoglobin and body cells How Your Lungs Work Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 5 Assessing Oxygenation • Physical assessment • Monitoring the client’s respiratory rate • Observing breathing pattern and effort • Checking chest symmetry • Auscultating lung sounds Patient Assessment • If patient becomes restless – this can be an early indication that the patient’s oxygenation status is compromised Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 7 Assessing Oxygenation (cont’d) • Arterial blood gases measure: • Partial pressure of oxygen dissolved in plasma (PaCO2) • Percentage of hemoglobin saturated with oxygen (SaO2) • The pH of blood • Level of bicarbonate (HCO3) Arterial Blood Gases Arterial Blood Gases Disadvantges • The procedure is invasive and painful • Careful monitoring by nurse to prevent complications after arterial puncture Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 10 Why Do an Aterial Blood Gas (ABG)? • Arteries have greater oxygen content than veins and responsible for carrying 02 to all cells. • ABGs are ordered to assess the client in acute respiratory distress or to evalute the progress of a patient receiving medical treatment Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 11 Assessing Oxygenation • Pulse oximetry • Composed of a sensor and a microprocessor • Noninvasive, transcutaneous technique for periodically or continuously monitoring the oxygen saturation of blood Pulse Oximetry • The SPO2 range for a patient who is adequately oxygenated would be • 95% - 100% Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 13 Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 14 Promoting Oxygenation • Positioning: high Fowler’s position – first step raise the head of the bed to promote breathing • Breathing techniques • Deep breathing – inhale as much air as possible, hold breath briefly- then exhale slowly • Incentive spirometry – deep inhalation with device to reach a goal level, hold breath briefly – remove mouthpiece and exhale normally • Pursed-lip breathing –inhale thru nose slowly , purse lips, contract abdomen, exhale through pursed lips slowly Promoting Oxygenation Diaphragmatic breathing 16 Oxygen Therapy • Oxygen sources • Wall outlet – hospitals, rehab • Portable tanks – before using “crack” the tank to remove any dust and debris from the outlet • Liquid oxygen unit • Oxygen concentrator – portable, used in LTC Pulmonary Nursing Chapter 36 Airway Management The Airway • The respiratory system • The importance of a clear airway Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 20 The Airway and Related Structures • Structures that protect the airway from inhaled substances • Epiglottis – acts as a “lid”that closes during swallowing directs fluid and food towards esophagus rather than respiratory tract • Tracheal cartilage – keeps airway open • Mucous membrane – lines respiratory passages –traps particulate matter • Cilia – collects debris that collects in the lower airway upwards Gerontologic Considerations Respiratory celia becomes less efficient with age, pre-disposing older adults to a high incidence of pneumonia Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 23 The Airway (cont’d) • Definition of sputum: Mucus raised to the level of the upper airways Natural Airway Management • Liquefying secretions • Encouraging adequate hydration • Inhalation therapy • Mobilizing secretions • Chest physiotherapy (page 813 –Fundamentals) • Postural drainage; Percussion • Vibration Aerosol Therapy Lung Segments and Corresponding Postural Drainage Positions Performing Postural Drainage Performing Percussion Natural Airway Management (cont’d) • Suctioning secretions • Nasopharyngeal suctioning • Nasotracheal suctioning • Oropharyngeal suctioning • Oral suctioning Variations in Suction Pressure Natural Airway Management (cont’d) • Suctioning secretions (cont’d) • Oropharyngeal suctioning • Oral suctioning Yankeur-Tip Suction Device for Oral Suctioning Artificial Airway Management • Oral airway • Tracheostomy • Tracheostomy tube • Tracheostomy suctioning • Tracheostomy care A Cuffed Tracheostomy Tube General Gerontologic Considerations • Pathologic pulmonary changes in older adults • Age-related changes affecting the older adult’s respiratory system • Pneumonia in older adults • Cough in older adults General Gerontologic Considerations (cont’d) • Respiratory secretions in older adults • Dysphagia in older adults • Cardiac dysrhythmias in older adults Skills for Respiratory Disorders • Oxygen Therapy • Goal of oxygen therapy is to prevent or relieve hypoxia. • Any patient with impaired tissue oxygenation can benefit from controlled oxygen administration. • Oxygen is not a substitute for other treatments and should be used only when indicated. • Oxygen should be treated as a drug. • Oxygen is expensive and can have dangerous side effects. • The dosage or concentration of oxygen should be ordered and continuously monitored. Skills for Respiratory Disorders • Oxygen Therapy (continued) • Oxygen is a colorless, odorless, and tasteless gas that will not burn or explode. • If combined with other factors, such as an electrical spark or fire, it will support combustion and ignite. • Oxygen therapy is frequently initiated by a respiratory therapist, who is a health care professional licensed to deliver treatment that will improve a patient’s ventilation and oxygenation needs. • The signs and symptoms manifested by patients who might require oxygen will vary according to the degree of oxygen deficiency. Oxygen Therapy (cont’d) • Equipment used in oxygen administration • Flowmeter – enables the nurse to regulate the quantity of oxygen delivered • Oxygen analyzer • Humidifier Oxygen Therapy -Common Delivery Devices •Nasal cannula – 2 to 5ML - low flow/low concentration of oxygen/with higher flow can cause the nasal mucosa to dry •Masks o Simple mask o Partial rebreather mask –monitor bag if collapses during inspiration call respiratory therapist o Non-rebreather mask o Venturi mask -higher flow rate 41 Oxygen Therapy (cont’d) • Common delivery devices (cont’d) • Face tent • Tracheostomy collar • T-piece • Additional delivery devices • Nasal catheter Administering Oxygen Safely Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 44 Comparison of Oxygen Delivery Devices Device Common Range Uses Nasal cannula 2-6 L/min Lower admin/can be drying to mucosa Simple mask 5-8 L/min Higher concentrations than nasal cannula, requires humidification Partial rebreather 6-10 L/min Required min of 6L/min increase amt of 02 with lower liter flows – monitor that bag is inflated at all times Nonrebreather 6-10 L/min Delivers highest fraction of inspired O2 with a mask (risk oxygen toxicity) Venturi 4- 8 L/min Delivers exact amount of prescribed oxygen Face tent 8-12 L/min Inconsistent fraction of inspired 02, comfortable for clients with facial trauma Oxygen Therapy (cont’d) • Additional delivery devices (cont’d) • Oxygen tent • CPAP mask – keeps the aveoli partially inflated even during expiration (nighttime use for sleep apnea) • Transtracheal oxygen • Oxygen hazards • Fire potential • Oxygen toxicity Skills for Respiratory Disorders • Oxygen Therapy (continued) • Transtracheal oxygen delivery • A newer method of oxygen delivery is the transtracheal catheter, which is inserted directly into the trachea between the second and third tracheal cartilages. • Delivery does not interfere with drinking, eating, or talking. • Oxygen is delivered throughout the respiratory cycle. • It is recommended for patients with heart failure or chronic obstructive pulmonary disease. • The transtracheal opening should be inspected and cleaned regularly. Transtracheal Catheter A transtracheal catheter may be inserted into the trachea between 2nd and 3rd tracheal cartilages. Skills for Respiratory Disorders • Oxygen Therapy (continued) • Care of the tracheostomy • A tracheostomy is an artificial opening made by a surgical incision into the trachea. • It is performed to provide the patient with a patent airway. • After the surgical procedure is performed, the physician inserts a tracheostomy tube and secures it in place with cotton tape around the patient’s neck. • Sterile gauze is placed around the opening under the flange of the outer tube for skin protection. Skills for Respiratory Disorders • Oxygen Therapy (continued) • Care of the patient with a tracheostomy collar and T-piece/tube • This requires constant humidification to the airway. • The T-piece/tube is a T-shaped device with a 15 mm connection with large-lumen tubing. • A tracheostomy collar is a curved device with an adjustable strap that fits around the patient’s neck; an exhalation port remains open at all times and another connects to large-bore tubing. A, Trach tube (fenestrated) with inner cannula removed and cap in place to allow speech. B, Trach tube with obturator for insertion and syringe for inflation of cuff. T-piece/tube. Tracheostomy collar. • Hyperbaric oxygen therapy (HBOT) • Delivery of 100% oxygen at 3 times the normal atmospheric pressure within an airtight chamber • Helpful for significant burn injuries, gangrene because it provides 15 times the amount of oxygen to tissues when compared to breathing room air Nursing Implications • Nursing diagnoses: hypoxemia or hypoxia • Ineffective breathing pattern • Impaired gas exchange • Anxiety • Risk for injury (related to oxygen hazards) General Gerontologic Considerations • Reduced gas exchange and efficiency in ventilation; major age-related changes occur in the respiratory system • Respiratory muscles become weaker and the chest wall becomes stiffer as a result of calcification of the intercostal cartilage General Gerontologic Considerations (cont’d) • Diminished cough and gag reflexes, increased use of accessory muscles for breathing, increased mouth breathing, snoring • Inactive, debilitated, or chronically ill clients or smokers are at a higher risk for respiratory infections and compromised respiratory function Antitussives • Antitussives act in one of 3 ways: • Depress the cough center in the brain • narcotic and opioids; codeine, hydrocodone • Anesthetize stretch receptors in the respiratory tract • Nonopioids; diphenhydramine, dextromethorphan • Soothe irritated areas in the throat • Uses: • Relief of overactive or nonproductive cough 59 Antitussives (cont.) • Adverse Reactions • Constipation, drowsiness, dry mouth, nausea, postural hypotension • Drug Interactions • Opioids have addictive effects with other CNS depressants; use reduced dose • Increase analgesic effect of ASA 60 Decongestants • Decongestants – encourage sinus drainage, improves nasal air passage and reduces the feeling of nasal stuffiness • Directly affect alpha receptors of blood vessels in the nasal mucosa, causing vasoconstriction • Uses: relieve nasal congestion from allergies and upper respiratory infections • Adverse reactions – nervousness, nausea, dizziness • Drug interactions – will interact with MAO inhibitors, tricyclic antidepressants, antihistamines, caution with htn patients 61 Expectorants • Expectorants (Guaifenesein, Mucinex, Robitussin • Decrease the thickness of respiratory secretions, thereby facilitating expectoration • Uses: treat productive cough, assist with thick mucus • Adverse reactions - GI upset, dizziness, headache • Drug interactions – No interactions noted with Guaifenesein, etc. 62 Topical Intranasal Steroids – (Flonase, Nasonex, Nasacort AQ) • Action • Anti-inflammatory effect to reduce nasal congestion • Uses • Treatment of allergic, mechanical, or chemically induced local nasal inflammation or nasal polyps when usual treatment has failed to work • Adverse reactions • Asthma, headache, lightheadedness, loss of sense of smell, nasal irritation and dryness, nausea, nosebleeds, perforation of nasal septum, altered sense of taste and smell 63 Asthma • Asthma is a condition that involves increased inflammation, swelling, and mucus production that lead to bronchiolar constriction. The person is able to breathe air into the lungs but has difficulty breathing out. Wheezing results because the person works to force air out through narrowed, mucusfilled passages during expiration. • The four classes of asthma severity include mild intermittent, mild persistent, moderate persistent, and severe persistent. 64 COPD • COPD is a chronic, disabling disorder that causes destruction of alveolar walls. This destruction creates unequal areas of ventilation and perfusion in the body, and oxygen and carbon dioxide exchange is impaired. Patients experience difficulty in expiration. 65 Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 66 Asthma and COPD Medications • Prophylactic treatment (prevention) • Cromolyn sodium (used to manage bronchial asthma) • Nedocromil sodium • Actions: • Slows down destruction of sensitized mast cells; also may provide hyposensitization (decrease in allergic response) 67 Asthma and COPD Medications (cont.) • Bronchodilators • Sympathomimetics aka adrenergic stimulants (Albuterol) • Relax smooth muscle of bronchi (dilate) • Vasoconstriction of blood vessels in body (decreases mucosal and sub mucosal edema) • Increase the rate and force of heart contraction • Uses: • Relief of symptoms of bronchospasm in acute or chronic asthma, bronchitis, and COPD 68 Asthma and COPD Medications • Xanthines (Aminophylline, Theophylline) • Relax smooth muscle in the bronchi and blood vessels in the lungs • Directly act on the kidney to produce an increase in urine production • CNS effects • Uses • Adjunctive therapy for bronchospasm in acute and chronic bronchial asthma, bronchitis, emphysema • Treatment of neonatal apnea • Acute pulmonary edema 69 Asthma and COPD Medications • Leukotriene Receptor Inhibitors (Singulair, Accolate) • Reduce symptoms of asthma by blocking receptors for cysteinyl leukotrienes C4, D4, and E4 • Uses • Treat acute or chronic asthma in patients unable to take inhaled glucocorticoids 70 Asthma and COPD Medications • Corticosteroids - Block reaction to allergens and reduce airway hyper responsiveness • Inhibit cytokine production, protein activation, and inflammatory cell migration and activation ( works on the inflammatory response) • Uses • Inhaled long-term asthma control (Pulmicort, Flovent, AeroBid) • Systemic (Prednisolone) often used to get quick control of the disease when beginning long-term therapy or to speed recovery from severe episodes 71 Administering Medications to Mucous Membranes • Absorption • Easily absorbed • Easily reaches therapeutic levels • Different mucous membranes have different drug sensivitivies • Blood supply under mucous membranes varies • Technique • Use aseptic or clean technique • Wear gloves 72 • Nose • Act locally to treat minor congestion or infection • Spray absorbs quicker than drops • Nasonex, Flonase, Afrin • Respiratory • Nebulizers/Aerosols • Medication diluted according to instructions and delivered using oxygen • Breath slowly and deeply until medication gone • Clean between uses • Metered-dose inhalers • Deliver specific amounts of corticosteroids/bronchodilators to nasal/lung tissue Pulmonary Edema Pulmonary edema is an abnormal buildup of fluid in the lungs. This buildup of fluid leads to shortness of breath. 74 Nutrition • Principles of diet therapy for pulmonary edema • Sodium restriction • Fluid restriction • Texture • Nutritional adequacy • Little or no alcohol 75 Copyright © 2013, 2010, 2006, 2003, 2000, 1995, 1991 by Mosby, an imprint of Elsevier Inc. 76