Myasthenia Gravis
advertisement
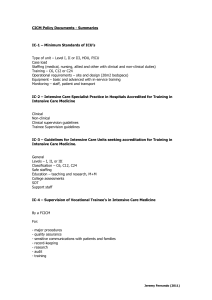
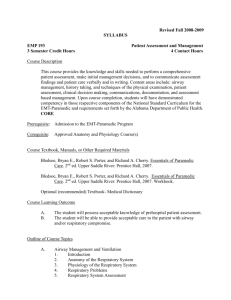
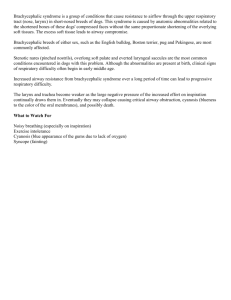
Myasthenia Gravis 21/2/11 FANZCA Part II Notes PY Mindmaps - autoimmune disruption of post-synaptic acetylcholine receptors @ NMJ up to 80% of functional receptors loss typically young woman may have thymus hyperplasia prevalence = 14.2 cases per 100,000 HISTORY - mild ptosis -> bulbar palsy and respiratory failure - most marked after prolonged exertion - severity of MG (duration, functional capacity, doses of medications) - dose of steroid and duration - may be on immunosuppressive agents, plasmapheresis or immunoglobulin infusion - bulbar symptoms - upper airway muscle weakness can produce a myasthenic crisis (airway collapse and obstruction + inability to swallow secretions) - chewing fatigue - significant other cardio/respiratory disease – heart failure, COPD, restrictive lung disease, recurrent aspiration pneumonia EXAMINATION - swallow functional capacity effectiveness of cough jaw closure often weak and cannot be maintained against resistance airway assessment focused RESP and CVS examination evidence of proximal myopathy and strength Reasons to present to ICU and requiring MV - upper airway obstruction inability to clear secretions pneumonia post surgical procedures (including thymetomy resection) tapering of immunomodulatory therapy pregnancy with disease exacerbation INVESTIGATIONS Diagnostic - edrophonium test (tensilon test) Jeremy Fernando (2011) - electrophysiological studies - EMG - Ach receptor and muscle specific receptor tyrosine kinase antibody testing Respiratory assessment - spirometry PEFR CXR ABG MANAGEMENT ICU Management Resuscitate - admit to ICU if VC < 25mL/kg, weak cough, not clearing secretions - intubate if indicated (airway protection, fatigue, hypercapnic respiratory failure) - physio Specific Therapies - anticholinesterase inhibitors: pyridostigmine, rivastigmine - plasma exchange - IVIG - corticosteroids (treatment resistant MG crises) - restart oral medications as soon as possible (may need IV neostigmine (30mg pyridostigmine:1mg neostigmine) or hydrocortisone if not able to tolerate PO medications) - incentive spirometry - introduction to physiotherapy - GORD/aspiration prophylaxis: H2 antagonists, Na+ citrate, metoclopramide, appropriate starvation Underlying Cause - thymectomy - good analgesia Intraoperative - avoid muscle relaxation if possible (may not be given major abdominal surgery) - if required use small titrated doses of NDNMB (10mg atracurium IV boluses) – very sensitive - plasmapheresis depletes plasma choline esterase levels -> prolonged action of sux, miv, remi + ester based LA’s - sux can be used (dose 1.5mg/kg) - keep warm - use PNS - intubation - MRSI if indicated Jeremy Fernando (2011) - controlled ventilation - volatile maintenance - good analgesia - intraoperative hydrocortisone/dexamethasone if indicated - avoid reversal if possible (increased risk of cholinergic crisis) -> if need to reverse use standard doses - extubate once wide awake and obey commands (able to lift head off pillow for 5 seconds) - N/G tube may be required so can have regular medication - discussion with neurology about patient degree of optimisation required for surgery - plan for post-operative ventilation if required (ICU) - plan for analgesic technique as indicated Predictors of Post operative Ventilation - major body cavity surgery duration of disease (> 6 years) history of chronic respiratory disease dose requirements of >750mg/day preoperative VC of <3L Drugs exacerbating MG - neuromuscular blocking drugs antibiotics: aminoglycosides, macrolides CVS drugs: beta-blockers, Ca2+ channel blockers, procainamide, quinidine corticosteroids Mg iodinated contrast d-penicillamine opioids: morphine and pethidine Jeremy Fernando (2011)