Best Practices at JHPIEGO
advertisement
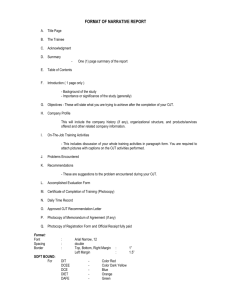
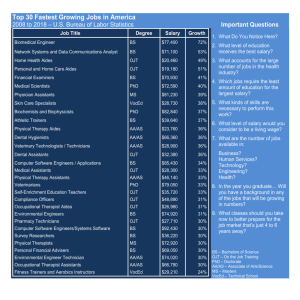
Applying TRH Best Practices in the Field Ron Magarick The Training in Reproductive Health Project (TRH) at JHPIEGO 29 November 2001 1 Overview: Training in Reproductive Health The TRH Project works globally to establish integrated (pre- and inservice) education and training systems to improve the performance of reproductive health professionals. . . 2 Selected TRH Best Practices • Strengthening preservice education and training • Improving provider performance through implementing competency-based training approaches using: – Anatomic models – Structured on-the-job training • And one more Surprise Best Practice 3 Best Practice: Strengthening Preservice Education and Training 4 Reasons to Strengthen Preservice Education and Training for All Health Professionals • Prepares students to become skilled FP/RH providers immediately after graduation • Students start off with “correct” information, attitudes and behaviors • RH skills perceived as part of basic package of skills • Faculty/preceptors become advocates for RH services • Can reach more providers than inservice training • Reduces reliance on inservice training by providing graduates with basic skills (IP, pelvic exam, counseling) 5 Essential Elements in Preservice Education and Training • Linkages between the classroom and clinical practice established and strengthened • Standardized RH curriculum developed • Clinical knowledge/skills strengthened and training skills of faculty/tutors/clinical preceptors updated • Clinical practice sites standardized • Training materials developed and made available to faculty, trainers and students 6 JHPIEGO’s Preservice Education and Training Program in the Philippines • Decade-long program (1987-1998) – Strengthen preservice nursing and midwifery education for FP/RH (strengthen curriculum, trainers, clinical training sites) – 27 nursing and midwifery schools • Program evaluation (February-March 2001) – Study Sample:16 schools (8 nursing, 8 midwifery) 7 Philippines: Summary of Findings 3 years later: • Policy: FP/RH questions incorporated in licensure examinations • Programmatic: Strengthened nursing and midwifery schools continue to implement competency-based FP/RH preservice education • Sustainability: Schools maintaining strengthened program • Trained faculty available • Implementation of FP/RH curricular components continues • Functioning clinical training sites available • School faculty used as resources for programs at other schools and in other clinical areas (e.g., HIV/AIDS) • Impact: Graduates better prepared for service delivery Graduates From Strengthened Schools Performed Better on Licensure Examinations Nursing Licensure Examination Passing Rates: Philippines 100 90 Nursing: National Rate Percentage 80 Nursing: Rate for 4 Program Schools 70 60 50 40 30 20 10 0 1998 1999 Year 9 Best Practice: Competency-based Training Using Anatomic Models 10 Why Use Anatomic Models? • Clients are not harmed or inconvenienced if a mistake is made • Difficult tasks, or parts of a procedure, can be practiced repeatedly • Practice of a sequence of steps or skills can be repeated at any time and as often as needed • Several participants can practice simultaneously • Practice is not limited to the clinical situation, or to a time when clients are available Why Use Anatomic Models? • Promotes learning by doing • Uses a humanistic training approach (i.e., uses anatomic models to ensure competency before working with clients) 12 Competency-based Learning Packages Chulalongkorn University: Using Anatomic Models Can Increase Training Efficiency IUD Insertion: Number of Clients Needed to Achieve Competency 100 90 80 70 60 50 40 30 20 10 0 2-week course with models 6-week traditional course 1st 3rd 5th 8th Client Number Source: Ajello et al, 1994. 16th Humanistic Approach Conclusion • Clinical training is possible even when the client caseload is low because fewer cases are needed for participants to attain skill competency • Training time is reduced, resulting in: – Lower costs for training – Less disruption of services due to provider absence 16 Best Practice: Competency-based Training in Postabortion Care Using Structured On-the-Job Training 17 The PAC/OJT, Self-Directed Learning Package • The postabortion care/structured on-the-job training (PAC/OJT) approach – Reduces the need for group-based courses – Increases training flexibility – Supports decentralized training systems 18 PAC/OJT Learning Package Addresses the Need for More Flexible Training • Main advantages – Enables the training of individual or a small number of trainees without putting undue burden on trainers or training site – Is much more flexible, and requires less logistic support than traditional group-based training Core Group Prepared as PAC/OJT Trainers in Zambia • Core group of 14 service providers from 3 model clinical training sites prepared as trainers – IP, FP etc. skills updated and PAC clinical skills standardized to establish model services – Introduced to the PAC/OJT package – Trained in clinical training skills using ModCAL, a selfpaced computer-assisted learning approach – Oriented to trainer’s role in the PAC/OJT package – Received supportive supervision visits to initiate training 20 PAC/OJT Results in Zambia • Three teams have begun OJT for staff within their own sites (12 physicians and nurses currently being trained at Kitwe, Ndola and University Teaching Hospital) • National action plan – to establish PAC services in 100 sites nationwide – based on implementing the self-directed/structured OJT approach • 16 to 24 new service providers are expected to receive training as OJT trainers in the coming year Surprise Best Practice 22 Establishment of the Regional Centre for Quality of Health Care Institute of Public Health, Faculty of Medicine, Makerere University, Kampala, Uganda 23 RCQHC Mission The RCQHC was established to provide leadership in building regional capacity to improve quality of health care by promoting better practices through networking, strategic partnerships, education and training. REGIONAL CENTRE FOR QUALITY OF HEALTH KAMPALA, UGANDA KAMPALA, UGANDA 24 Regional Centre for Quality of Health Care (RCQHC) • Based at Makerere University and affiliated with Makerere’s Institute of Public Health • Opened February 2000 • Supported by a consortium of USAID CAs • Staffed by leading African clinicians and trainers – – – – – Reproductive Health Advisor Maternal Health Advisor Malaria Advisor HIV/AIDS Advisor Nutrition Advisor Centre Accomplishments Worked to develop and pretest short courses (RH, nutrition, HIV/AIDS, malaria) and develop a diploma course in QoC • Provided technical assistance to MOHs within the region in curriculum and job aid development (e.g nutrition, MNH, RH) • Organized a State of the Art meeting on Improving Quality of Care in the region (230 participants attended) • Provided TA to many NGOs in the region 26 Centre Accomplishment: Strengthening Technical Skills in the Region .