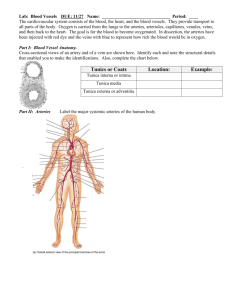
Tunica media
advertisement

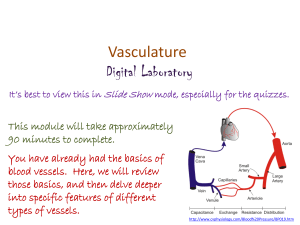
Chapter 23 Blood Vessels Blood Vessel Tunics • Walls of blood vessels have three layers, or tunics 1. Tunica externa (adventitia) – anchor BV to an organ • Larger blood vessels require own blood supply – vasa vasorum in tunica externa 2. Tunica media – smooth muscle • • Sympathetic input vasoconstriction Parasympathetic input vasodilation 3. Tunica intima (interna) – endothelium (simple squamous ET lining) • Continuous with endocardium Blood Vessel Tunics Microscopic Comparison of Arteries and Veins Types of Arteries • Three types of arteries: 1. Elastic arteries • • Largest arteries, close to heart Thick tunica media w/ elastic fibers 2. Muscular arteries • • Medium diameter Proportionally thicker tunica media 3. Arterioles –smallest arteries • • Thin tunica media (< 6 layers) Connect to capillaries Capillaries • Capillaries – Diameter slightly larger than erythrocyte • Tunica intima only – Allows for rapid diffusion • Form capillary beds – Blood flow regulated by precapillary sphincters – Thoroughfare channel bypasses bed • Site of metabolic exchange Types of Capillaries 1. Continuous – most common – continuous and complete endothelium (no physical holes) 2. Fenestrated – endothelial cells possess small “holes” – allow fluid exchange between blood and interstitial fluid • eg. kidneys 3. Sinusoid – large gaps between endothelial cells – promotes transport of large molecules and cells to and from blood • eg. Liver and spleen Veins • Drain capillaries – return blood to heart • Pressure much lower than in arteries – Walls much thinner – Very little muscle in tunica media • At rest, veins hold about 60% of body’s blood – function as blood reservoirs Venules • Smallest veins • Postcapillary venules smallest – Diapedesis occurs here • Venules merge to form veins Veins • Skeletal muscle pump moves blood toward heart – Contraction of muscles • Blood pressure too low to overcome gravity – valves prevent backflow and pooling of blood in limbs – formed from tunica intima Varicose Veins Venous Return from the Abdomen • Special system of circulation - hepatic portal system • Drains blood from GI organs and shunts blood to liver – Allows for filtering of ingested substances Fetal-Placental Circulation Fetal circulation bypasses the developing lungs, kidneys, and digestive tract All nutritional, respiratory, and excretory needs are met by the placenta The exchange occurs via capillaries- mom’s and baby’s blood don’t mix. ttp://www.ethal.org.my/opencms/opencms/ethal/Images/MedGeneralImages/Placenta.gif Fetal-Placental Circulation • Fetal system has structures that are modified or cease to exist after birth • Fetal circulatory pathway: – Oxygenated blood from placenta umbilical vein ductus venosus (bypasses liver) inferior vena cava right atrium foramen ovale (shunt to LA) left ventricle aorta – Some blood from RA RV pulmonary trunk ductus arteriosus (shunt to aorta) – Aorta body umbilical arteries (now deoxygenated) placenta nutrient and gas exchange Fetal-Placental Circulation • Postnatal changes – Umbilical vessels constrict and cease function – Ductus venosus becomes ligamentum venosum – Foramen ovale becomes fossa ovalis • Failure to close at birth = patent foramen ovale – Ductus arteriosus becomes ligamentum arteriosum • Failure to close at birth = patent ductus arteriosus