Assessment of Digestive and GI Function
advertisement

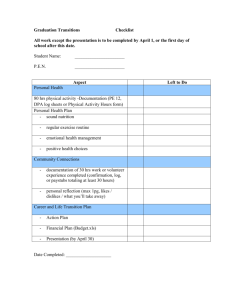
Assessment of Digestive and GI Function Connie K. Cupples, MS, MSN, RN Union University Outcome 1 • Review the structure and function of the organs of the GI tract. • A. Draw abdomen depicting organs in the four quadrants. • B. Identify function of each of the organs of digestion. Abdomen Function of Organs • • • • Mouth Stomach Small Intestine Colon Outcome 2 • Explain the processes involved in the digestion, absorption, and elimination of food products. A. Identify major digestive enzymes, sources, and digestive actions. refer to pg. 943 table 34-1 Action of enzymes that digest CHO, protein, and fat Outcome 3 • Describe assessment paramaters and techniques used when evaluating the GI tract. • A. Draw a torso and shade common sites of referred abdominal pain. • B. Discuss the order of the examination of the abdomen and give the rationale. Sites of Referred Abdominal Pain Health History • Focus on symptoms common to GI dysfunction: Pain Indigestion Intestinal gas Change in bowel habits Change in stool characteristics Physical Assessment • Inspect mouth and contents • Supine with knees flexed slightly • Order of assessment: inspection auscultation palpation percussion Rationale for order of GI Assessment? Abdomen - Ascites Abdomen-Obese Abdomen - Hernia Outcome 4 • Describe preparation, education, and follow-up care for patients undergoing the following diagnostic testing of the GI tract. • A. Discuss how the nurse would prepare and educate patients for GI tests, including post procedure interventions. Stool Tests • Collect on random basis except specimen where quantitative study is performed (fecal fat and urobilinogen) • Refrigerate quantitative specimen (24-72 hr. collections) • Special diet required for some tests • Fecal occult blood tests (foods & meds may alter results. Abdominal Ultrasonography • Noninvasive means of imaging abdominal organs and structures. • NPO for 8-12 hrs. • Fat-free meal at supper if GB studies are done • Schedule barium studies after test if ordered as well Upper GI X-ray Studies X-ray imaging after contrast media injested. Low residue diet X several days prior NPO after MN Laxative prep Discourage smoking day of test Hold all meds on day of test Monitor post test for 3 days to get rid of barium (fluids, laxatives, enemas) Lower GI X-ray Studies • Visualization of lower GI tract after instillation of barium • Bowel prep to cleanse lower bowel • Low-residue diet 1-2 days prior • C/L diet for supper, laxative HS, NPO after MN • Cleansing enemas until clear in a.m. • Post procedure elimination of barium CT • Cross-sectional images of abdominal organs and structures • NPO 6-8 hrs. before test • Question about contrast dye allergies • Schedule barium studies after CT scan if ordered MRI • Noninvasive technique to supplement ultrasonography and CT scanning • NPO 6-8 hrs. prior to test • Remove all jewelry & other metals • Explain that procedure lasts 30-90 minutes • Explain type of equipment used (pt. may experience claustrophobia & hear knocking sound) Esophagogastroduodenoscopy • Visualization of upper GI tract with fiberoptic lenses. • NPO 6-12 hrs. • Pt. may gargle with local anesthetic • Versed given IV – monitor pt. per conscious sedation protocol • Atropine may be given to dry secretions • Position on left side during procedure Nursing Interventions Post EGD • Keep NPO until return of gag reflex • Simms position until awake, then semifowlers • Observe for s/s of perforation (pain, bleeding, unusual difficulty swallowing, temp) • Monitor for changes in P & BP • Instruct not to drive for 10-12 hrs. post EGD Colonsocopy • Direct visual inspection of the colon using flexible fiberoptic colonoscope. • Colon preparation a must • C/L diet at noon day before • Laxatives the night before • Use of preparation such as Golytely to lavage the bowel over 3-4 hrs. until returns are clear Nursing Interventions post Colonoscopy • Monitor according to conscious sedation guidelines • Observe for s/s of bowel perforation (abdominal pain, distention, rectal bleeding, temp) • Provide written instructions due to amnesic effect of meds Colonoscopy Gastic Analysis, Gastic Acid Stimulation test & pH Monitoring • Determines secretory activity of gastic mucosa and gastric retention. • NPO 8-12 hrs. • Hold meds that affect gastic secretion • Smoking not allowed day of test • Insert small NG tube • Aspirate entire contents of stomach q 15 minutes for 1 hr. Gastic Acid Stimulation • • • • Med given to stimulate gastric secretion Inform pt. that flushing may occur Monitor P & BP q 15 min. Collect gastic specimen q 15 minutes for 1 hr. pH Monitoring • • • • NPO 6 hrs. before test Hold meds 24-36 hrs. Probe inserted through nose Connected to external recording device