Gastrointestinal Disorders Chart 4.0
advertisement
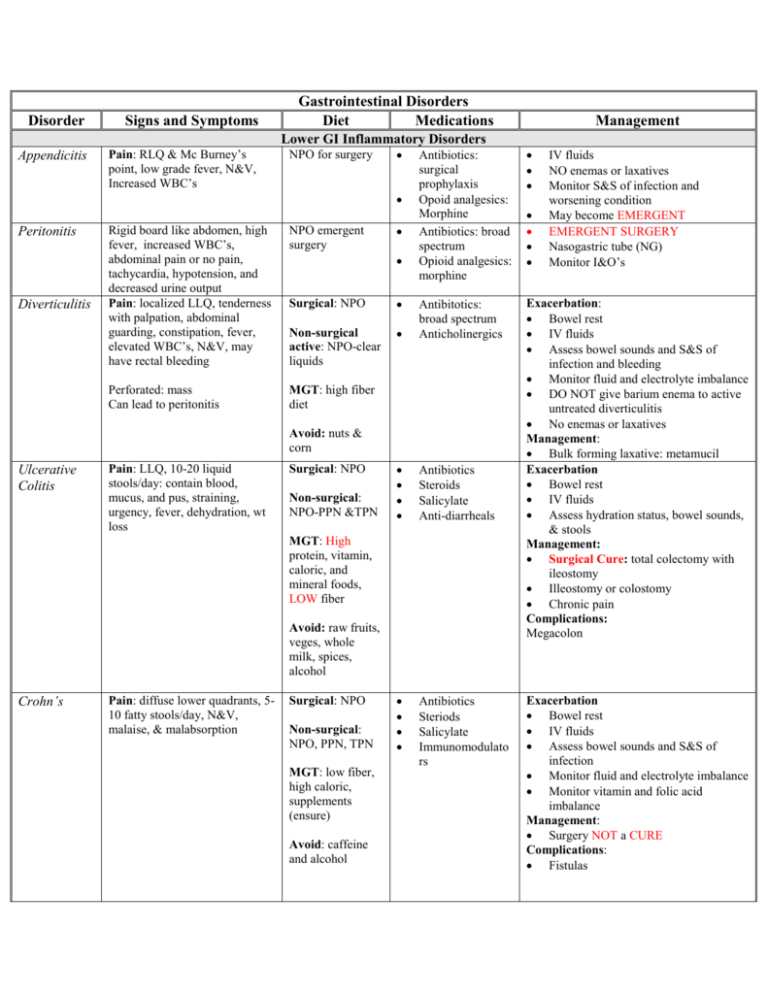
Disorder Signs and Symptoms Appendicitis Pain: RLQ & Mc Burney’s point, low grade fever, N&V, Increased WBC’s Gastrointestinal Disorders Diet Medications Management Lower GI Inflammatory Disorders NPO for surgery Peritonitis Diverticulitis Rigid board like abdomen, high fever, increased WBC’s, abdominal pain or no pain, tachycardia, hypotension, and decreased urine output Pain: localized LLQ, tenderness with palpation, abdominal guarding, constipation, fever, elevated WBC’s, N&V, may have rectal bleeding NPO emergent surgery Perforated: mass Can lead to peritonitis MGT: high fiber diet Antibiotics: surgical prophylaxis Opoid analgesics: Morphine Antibiotics: broad spectrum Opioid analgesics: morphine Exacerbation: Bowel rest IV fluids Assess bowel sounds and S&S of infection and bleeding Monitor fluid and electrolyte imbalance DO NOT give barium enema to active untreated diverticulitis No enemas or laxatives Management: Bulk forming laxative: metamucil Exacerbation Bowel rest IV fluids Assess hydration status, bowel sounds, & stools Management: Surgical Cure: total colectomy with ileostomy Illeostomy or colostomy Chronic pain Complications: Megacolon Surgical: NPO Non-surgical active: NPO-clear liquids Antibitotics: broad spectrum Anticholinergics Antibiotics Steroids Salicylate Anti-diarrheals Antibiotics Steriods Salicylate Immunomodulato rs Avoid: nuts & corn Ulcerative Colitis Pain: LLQ, 10-20 liquid stools/day: contain blood, mucus, and pus, straining, urgency, fever, dehydration, wt loss Surgical: NPO Non-surgical: NPO-PPN &TPN MGT: High protein, vitamin, caloric, and mineral foods, LOW fiber Avoid: raw fruits, veges, whole milk, spices, alcohol Crohn’s Pain: diffuse lower quadrants, 510 fatty stools/day, N&V, malaise, & malabsorption Surgical: NPO Non-surgical: NPO, PPN, TPN MGT: low fiber, high caloric, supplements (ensure) Avoid: caffeine and alcohol IV fluids NO enemas or laxatives Monitor S&S of infection and worsening condition May become EMERGENT EMERGENT SURGERY Nasogastric tube (NG) Monitor I&O’s Exacerbation Bowel rest IV fluids Assess bowel sounds and S&S of infection Monitor fluid and electrolyte imbalance Monitor vitamin and folic acid imbalance Management: Surgery NOT a CURE Complications: Fistulas