Critical Appraisal of Articles About Diagnostic Tests
advertisement
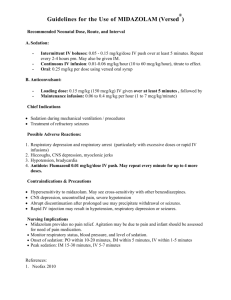
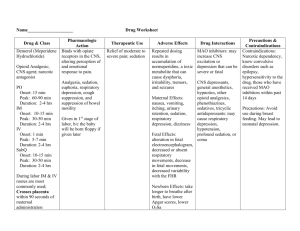
CRITICAL APPRAISAL OF DIAGNOSTIC ARTICLE 10/5/2009 1 Does End Tidal CO2 Monitoring During Emergency Department Procedural Sedation and Analgesia With Propofol Decrease the Incidence of Hypoxic Events? Randomized, Controlled Trial Annals of Emergency Medicine Article in Press, 2009 10/5/2009 2 Learning Objectives Introduction Discussion of the article Critical appraisal of the article Important calculations Overview on LR 10/5/2009 3 Introduction Procedural sedation & analgesia for management of acute procedural pain & anxiety in the (ED) is part of core competency in emergency medicine. A.C.E.P & A.S.A recommend continuous monitoring of PR & rhythm, RR, BP, & pulse oximetry during moderate and deep sedation 10/5/2009 4 Introduction Use of real-time capnography as adjunct to current procedural sedation safety and monitoring practice is under increasing scrutiny. Capnography noninvasively measures the partial pressure of CO2 in exhaled breath & is tightly correlated with arterial CO2 in patients with normal lung function 10/5/2009 5 Introduction Minute ventilation is depressed by sedatives by reducing respiratory rate or tidal volume. Respiratory depression may produce hypercapnia (RR > VT ) or hypocapnia (VT > RR ) 10/5/2009 6 Introduction There is now compelling evidence that capnography identifies respiratory depression well before the onset of hypoxia. This modality should allow physicians to intervene to improve ventilatory status. 10/5/2009 7 Importance Although pulse oximetry, PR, and BP monitoring are considered routine practice during ED procedural sedation & analgesia, capnography is not. If the addition of capnography helps physicians reduces hypoxia, then perhaps it should also be routine. 10/5/2009 8 Goal of Study determine whether physician use of realtime capnography is associated with a 15% decrease in the incidence of hypoxia compared with standard monitoring alone during ED procedural sedation with propofol 10/5/2009 9 Materials & Methods 10/5/2009 10 Study Design prospective, randomized controlled trial conducted from November 2006 to February 2008. 10/5/2009 11 Setting & Selection of Participants Study was conducted at Albert Einstein Medical Center, a 600-bed teaching hospital located in Philadelphia, with an annual ED census of 75,000 patients. Enrolled consecutive (24 hours a day, 7 days a week) adults >18 years & selected for propofol sedation in accordance with their usual practice 10/5/2009 12 Setting & Selection of Participants Exclusion critiria: * severe chronic obstructive pulmonary disease; * chronic oxygen requirements; * hemodynamic instability; * respiratory distress; * pregnancy; *Inability to provide informed consent; * allergy to propofol, morphine, or fentanyl (or other components of its formulation); * or if, in judgment of the attending emergency physician, procedural sedation could compromise patient safety. Informed consent was obtained from each subject. 10/5/2009 13 Setting & Selection of Participants Pts randomly assigned to study group (standard monitoring and capnography) or control group (standard monitoring and blinded capnography) by research associates using computer-generated randomization list. Research associates & treating physicians were blinded to the randomization choice until after enrollment. 10/5/2009 14 Setting & Selection of Participants Inaddition to standard electronic monitoring, they attached a Capnostream 20 monitor, using a nasal-oral CO2 cannula capable of delivering compressed gasses, with an oral sampling port to accommodate mouth breathers 10/5/2009 15 Setting & Selection of Participants Capnostream 20 monitor displays oximetry and CO2 waveform and calculates ETCO2. All patients had capnography; for the blinded (control) group, the monitor screen was adjusted to permit visualization only by the research associate. 10/5/2009 16 Setting & Selection of Participants All patients received supplemental oxygen at 3 L/minute by nasal cannula. If the treating physician wished to deliver additional oxygen during the sedation, a nonrebreather mask connected to wall oxygen at 15 L/minute was placed over the cannula. All patients received 0.5 g/kg of fentanyl or 0.05 mg/kg of morphine for analgesia no fewer than 30 minutes before administration of propofol for sedation. 10/5/2009 17 Setting & Selection of Participants They started with propofol 1 mg/kg, administering additional boluses of 0.5 mg/kg until desired level of sedation was achieved. Patients closely monitored from the initiation of sedation until they were back to their baseline alertness and ready for discharge. 10/5/2009 18 Data Collection and Processing Data were collected by trained research associates, physicians who had participated in previous sedation studies & had no duties other than patient enrollment and data recording. They were trained in procedural sedation & analgesia, study protocol and its definitions, all monitoring devices, and signs of respiratory depression. 10/5/2009 19 Data Collection and Processing They recorded age, sex, medical history, Rx, allergies, types of procedures performed, vital signs, & sedation and procedure times on a standardized data collection instrument. The patient’s level of alertness was assessed at baseline, 90 s after preprocedure drug administration, & before discharge, using a modified Ramsay scale 10/5/2009 20 Data Collection and Processing Before the study, physicians & nurses trained in identification of respiratory depression with capnography Treating physicians were instructed to perform procedural sedation and analgesia according to standard protocol Any intervention for an adverse event should be based on their judgment and clinical expertise with or without capnography, depending on randomization arm. 10/5/2009 21 Data Collection and Processing Capnostream 20 records data electronically every 5 seconds during course of each sedation, Research associates used electronic marking and time stamping to record specific events such as drug administration, beginning and end of procedure, and point of readiness for discharge 10/5/2009 22 Data Collection and Processing They noted time and nature of any intervention for respiratory depression or hypoxia, such as verbal or physical stimulation, airway realignment, use of additional oxygen, and the use of airway adjuncts, assisted ventilation, or intubation. Research associates manually recorded other sedation-associated adverse events, including hypotension, bradycardia, arrhythmia, vomiting, prolonged ED stay, or admission 10/5/2009 23 Outcome Measures Electronic data from each sedation were downloaded from the monitor into a Microsoft Excel 2000 database & were checked for any discrepancies, with handwritten notations taken by the research associates. printed time evaluation graph of the patient’s sedation was then produced 10/5/2009 24 Outcome Measures 10/5/2009 25 Outcome Measures Before study blinding was broken, 3 investigators evaluated each graph to code the presence or absence of hypoxia & respiratory depression. Hypoxia was defined a priori as an SpO2 level of less than 93% for 15 seconds or greater. Respiratory depression was defined a priori as an ETCO2 level of 50 mm Hg or greater, an absolute increase or decrease from baseline of 10% or greater, or a loss of waveform for 15 seconds or greater 10/5/2009 26 Outcome Measures Grafs disqualified if they had greater than 35% data loss, unless all 3 evaluators agreed that there was unequivocal evidence of hypoxia or respiratory depression. Lost data were typically due to patient movement (ie, dislodgement of the cannula) or blood pressure cuff insufflation. 10/5/2009 27 Primary Data Analysis Data analyzed descriptively & using χ2, with P<.05 considered significant. All analyses were with SPSS version 10. Previous research has reported rates of hypoxia during ED propofol sedation ranging from 15% to 30%. To identify a 15% decrease in hypoxia from a 20% presumed baseline, they calculated that they would need 72 pts in each arm (assuming a 1-tailed analysis, a power of 80%, and an α of 5%). 10/5/2009 28 RESULTS 10/5/2009 29 Characteristics of Study Subjects 10/5/2009 30 Characteristics of Study Subjects 10/5/2009 31 Main Results 10/5/2009 32 Main Results majority of patients who developed respiratory depression had an ETCO2 change greater than 10% from baseline loss of waveform was most likely to lead to hypoxia. 10/5/2009 33 Main Results • With capnography there were more physician interventions to improve respiratory status, 24 of 68 (35%) versus 14 of 64 (22%; difference 13%; 95% CI –2% to 27%) 10/5/2009 34 Limitations They had a higher-than-expected disqualification rate, leaving slightly less than calculated 72 patients per group for analysis. However, they found a significant difference in their main outcome, and thus the study was not underpowered 10/5/2009 35 Limitations The observed rate of hypoxia (32.5%) was higher than that observed in most other studies of propofol for ED procedural sedation. A rate of hypoxia more consistent with previous studies may have produced a smaller, nonsignificant difference between groups 10/5/2009 36 Limitations possibly that the continuous electronic data collection using the Capnostream 20 influenced the rate of hypoxia because it would detect episodes that might otherwise be missed through recording only at spaced intervals or through human inattention or error. 10/5/2009 37 Limitations unlikely that any device error contributed to the higher-than-expected rates of hypoxia and respiratory depression It is possible that, if the clinicians had used greater amounts of supplemental oxygen, there would have been less overall hypoxia 10/5/2009 38 Limitations They chose a priori an SpO2 of 93% as baseline level for hypoxia because they believe that most physicians will pay close attention and potentially intervene at this level. A lower threshold would have resulted in less overall hypoxia. 10/5/2009 39 Discussion Rate of hypoxic events decreased by using capnography in conjunction with standard monitoring. (17%) Capnographic respiratory depression occurred before the onset of hypoxia and was temporally linked to subsequent hypoxic events. 10/5/2009 40 Discussion every patient who developed hypoxia had a corresponding ETCO2 change. the increased sensitivity of the nearcontinuous electronic data capture with the Capnostream 20 allowed to measure this effect. 10/5/2009 41 Discussion Capnography can provide early warning of ventilatory abnormalities, alerting physicians to respiratory depression before the onset of a hypoxic event. Using capnography in this study, emergency physicians improved pt safety by decreasing rate of hypoxic events ass. with procedural sedation & analgesia 10/5/2009 42 Discussion a number of patients had respiratory depression & hypoxia & treating physician did not intervene, with the episodes resolving spontaneously. If every incidence of respiratory depression had led to an intervention, it is possible that there would have been less hypoxia 10/5/2009 43 10/5/2009 44 1. Are the results in the study valid ? 10/5/2009 45 Primary Guide Was there an independent, blind comparison with a reference standard ? Did the pt sample include an appropriate spectrum of pts to whom the diagnostic test will be applied in the clinical practice ? 10/5/2009 46 Secondary guide Did the results of the test being evaluated influence the decision to perform the reference standard ? Were the methods for performing the test described in sufficient detail to permit replication ? 10/5/2009 47 What are the results? Are LR for the test results presented or data neccessery for their calculation provided ? 10/5/2009 48 R.D + R.D totals 10/5/2009 Hypoxia + 17 a 0 c 17 a+c Hypoxia 22 b 29 d 51 b+d totals 39 a+b 29 c+d 68 a+b+c+d 49 Results Sensitivity = a /a+c (TP among diseased) = 17 / 17 = 1 = 100% Specificity = d /b+d (TN among non diseased) = 29 / 51 = 0.57 = 57% 10/5/2009 50 Results PPV = a /a+b (TP among all Positives) = 17 / 39 = 0.44 = 44% NPV= d /c+d (TN among all Negatives) = 29 / 29 = 1 = 100% LH+ = (sens) / (1 - spec ) = 100 / 43 = 2.3 LR- = (1-sens) / (spec) =0 10/5/2009 51 Results Prevalence = (a+c) / (a+b+c+d) = 17 / 68 = 25 % Pre-test odds = prevalence / (1-prevalence) = 25 / 75 = 0.33 Post-test odds = pre-test odds * LR for (+) = 0.33 X 2.3 = 0.79 for (-) = 0.0.33 X 0 = 0 Post-test Probability = post-test odds / (post-test odds + 1) = 0.43 = 44 % 10/5/2009 52 10/5/2009 53 10/5/2009 54 Will the results help me in caring for my patients ? 10/5/2009 55 Will the reproducibility of the test results & its interpretation be satisfactory in my setting ? Are the results applicable to my patients ? Will the results change my management ? Will patients be better off as a result of the test ? 10/5/2009 56 10/5/2009 57 Definition (LR) is the likelihood that a given test result would be expected in a patient with the target disorder compared to the likelihood that that same result would be expected in a patient without the target disorder 10/5/2009 58 LH ratio for a positive result (LR+) tells you how much the odds of the disease increase when a test is positive. LH ratio for a negative result (LR-) tells you how much the odds of the disease decrease when a test is negative. 10/5/2009 59 Depending on article or source, a single LR might be presented without reference to “positive” or “negative” 10/5/2009 60 LR = 1 means the post-test probability is exactly the same as the pre-test probability LR > 1 increases the probability that the target disorder is present LR < 1 decreases the probability that the target disorder is present 10/5/2009 61 10/5/2009 62 Applications LR is used to assess how good a diagnostic test is and to help in selecting an appropriate diagnostic test(s) or sequence of tests. They have advantages over sensitivity and specificity because: they are less likely to change with the prevalence of the disorder, they can be calculated for several levels of the symptom/sign or test, they can be used to combine the results of multiple diagnostic test can be used to calculate post-test probability for a target disorder 10/5/2009 63