Platelets = thrombocytes
advertisement

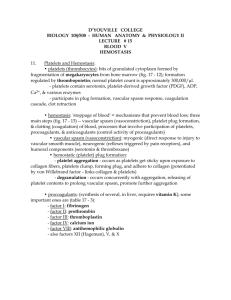
Platelets = thrombocytes Thrombopoiesis = Platelet formation * requires thrombopoietin (from liver) *occurs in the myeloid tissue *myeloid stem cell megakaryocytethousands of platelets(cell fragments) *”lifespan” = 10 days(no nucleus, not even complete cells Hemostasis – stoppage of bleeding • Hemostasis occurs in three stages: I) Vascular spasm- nature of vessels , due to pain and smooth muscle response - enhanced by serotonin and thromboxane A2 released from platelets II. Platelet plug formation – platelets aggregate and form a plug. Why? -enhanced by ADP and thromboxane A2 III. Blood coagulation – very complex, involves many plasma proteins, most synthesized in the liver. Vitamin K is found to be vital to this process. A) Intrinsic pathway- can happen in test tubes or unbroken vessels. Slower. Triggered by damaged endothelial cells (lining of blood vessels) A’) Extrinsic pathway – Faster. Triggered by damaged cells outside of bloodstream. Prothrombin (pp) ----------prothrombin activator/ Ca++-----------------------Thrombin (enz) Fibrinogen (pp) --------thrombin--------------------------Fibrin (mesh) Clot dissolution I. Fibrinolysis – dissolving (lysing)the fibrin A) An inactive plasma protein (pp), plasminogen, gets built into each clot. It is eventually activated by healing tissues to become an active enzyme called plasmin. This enzyme helps to dissolve the fibrin. Thrombosis Thrombosis is clotting in an unbroken vessel. The clot is called a thrombus. If it dislodges and travels to another part of the body, it is then called an embolus. An example in pulmonary embolism. Other substances….. • A) prostacyclin (from wbc’s) - inhibits thromboxane A2 and platelet adhesion • B) heparin (from wbc’s) – blocks thrombin • C) aspirin – blocks thromboxane A2 and prevents platelet aggregation Hemophilia X – linked , recessive. Results in a lack of one or more clotting factors involved in hemostasis. Who is most susceptible? MALES one X chromosome