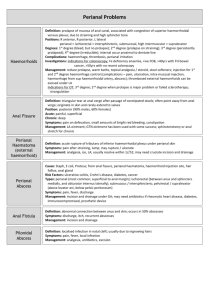
anorectal diseases
advertisement

Common Anorectal Diseases Lecturer: Professor Saleh M. AlSalamah FRCS Professor of Surgery & Consultant General and Laparoscopic Surgeon College of Medicine, King Saud University, Riyadh, KSA. References Clinical Surgery by Michael M. Henry Bailey and Love’s Short Practice of Surgery Essential of General Surgery by Peter F. Lawrence Objectives At the end of this presentation students will be able to: Understand the surgical anatomy of the anal canal. Classification, pathogenesis and management of hemorrhoids. Pathogenesis, presentation and management of anal fissure. Presentation. Classification and management of perianal abscess. Classification and management of anal fistula. Pathogenesis, presentation and management of anal carcinoma. Anorectal Diseases Overview Surgical Anatomy Congenital Abnormalities Examination of the Anus Common Anal Conditions Overview Anal and perianal disorders makeup about 20% of all outpatient Surgical referrals. These conditions are extremely distressing and embarrassing patient often put up with symptoms for long time, before seeking medical care. Common symptoms Anal bleeding Anal pain and discomfort Perianal itching and irritation Something coming down perianal discharge Surgical Anatomy The anal canal 1.5” (4 cm) long and is directed downward and backward from the rectum to end at the anal orifice. The mid of anal canal represents the junction between endoderm and ectoderm Surgical Anatomy The lower ½ is lined by squamous epithelium and the upper ½ by columnar epithelium so carcinoma of the upper ½ is adenocarcinoma. Where as that arising from the lower part is squamous tumour. Surgical Anatomy The blood supply of upper ½ of the anal canal is from the superior rectal vessels. Where as that of the lower ½ is supply of the surrounding anal skin the inferior rectal vessels which derives from the internal pudendal ultimately from the internal iliac vessels. Surgical Anatomy The lymphatic above the mucocutaneous junction drain along the superior rectal vessels to the lumbar lymph nodes, where as below this line drainage is to the inguinal lymph nodes. Surgical Anatomy The nerve supply to the upper ½ via autonomic plexus and the lower ½ is supplied by the somatic inferior rectal nerves terminal branch of the pudendal nerve. So the lower ½ is sensitive to the prick needle. Anal Sphincter The internal anal sphincter of in voluntary muscle, which is the continuation of the circular muscles of the rectum. The external sphincter of the voluntary muscles, which surrounds the internal sphincter and comprises 3 parts (formerly) subcutaneous the lower most portion of the external sphincter superficial part deep part Common Anal Conditions Haemorrhoids Pruritus ani Perianal abscess Anal fissure Anal fistula Rectal prolapse Anal in continence Non malignant strictures Anal neoplasms Congenital Abnormalities High abnormality more serious because it is associated with poor development of the pelvic muscles. Low abnormality which is simply to treat:These abnormalities should be diagnosed at birth is the standard physical examination of the new born infant. If the diagnosis missed the infant developed symptoms and signs of large bowel obstruction. Congenital Abnormalities High abnormalities: The rectum stops short of the pelvic floor and the anal canal is absent. Low abnormalities: The abnormality is usually either ectopic or covered anus. Diagnosis On physical examination: If the baby fail to produce meconium stool in the first few hours of life. Investigation: urine for meconium, if no meconium is visible the site of the anus marked with metal and x-ray taken for the baby up side down so gas shadow may helps to show the distal point of bowel development. Treatment Need early and vigorous treatment in infancy. Low abnormalities: should be treat by “cutback type operation” followed by regular digital dilatation by the mother. High abnormalities: should be treated by colostomy in the 1st few days followed by some sort “pull through operation” at the age of one year. Examination of Anus This requires careful attention to circumstances (couch, light, gloves). The Sims (left lateral position) is satisfactory. The examination proceed by; inspection digital examination with index finger proctoscopy sigmoidoscopy Hemorrhoids Piles may be internal or external according to whether they are internal or external to anal orifice. The internal Haemorrhoids: They are dilation of the superior haemorrhoidal veins above the denate line each pile consists of mass of dilated vein, artery, some connective tissue and mucosal investment. Hemorrhoids The location of piles, right anterior, right posterior and left lateral situated respectively 11, 7, 3 o’clock with patient in the lithotomy position, these are give daughter piles. Etiology Primary Causes: Hereditary factors e.g, structural weakness of the vein. Anatomical factors. Partial congestion. Chronic constipation. Sphincteric relaxation. Etiology Secondary Causes: pregnancy venous obstruction straining on micturation venous congestion carcinoma of the rectum Clinical features Bleeding at defecation Prolapse Discharge with pruritus ani Pain Thrombosed piles Assessment and Diagnosis Careful history Abdominal Examination Anorectal Examination Investigation e.g., proctoscopy Complications Profuse haemorrhage Acute thrombosis Treatment Treatment Injection treatment Gabriel syringe is filled with sclerosant 5% phenol with almond oil Barron’s rubber banding Cryosurgery Co2 Laser Lord’s manual dilation Hemorrhoidectomy Stapled Hemorrhoidectomy External Hemorrhoids Perianal Hematoma Due to rupture of dilated anal vein as result of sever straining. Sudden onset of painful lump at the anus. Swelling tense & tender, bluish in colour covered with smooth shining skin. External Hemorrhoids Treatment Evacuation if the patient come within 48hours If patient come late conservative treatment. If untreated the haematoma undergoes: resolution ulceration suppuration to forms in abscess fibrosis which give rise to skin tag. Perianal Abscess The infection usually starts in one of the crypts of Morgagni and extends along the related anal gland to the intersphincteric plane where it forms as abscess. Soon it tracks in various directions to produce different types of abscesses . Types of Abscess Perianal abscess (60%) Ischiorectal abscess (30%) Sub mucous abscess (5%) Pelvirectal abscess Perianal Abscess Patient with recurrent anorectal abscess always consider associated underlying diseases such as Crohn’s, UC, rectal cancer and active TB. Perianal Abscess Symptoms Acute pain High fever Signs Swelling Tenderness with induration Treatment Incision and drainage and covered by antibiotics. Perianal Abscess Fistula in ano Defined as track lined by granulation tissues, which connects deeply in the anal canal or rectum and superficially on the skin around the anus. It usually result from an anorectal abscess. Fistula in ano Anal fistulas have well recognized association with crohn’s disease, UC, TB, colloid carcinoma of the rectum and lympho granuloma venercum. Types of Anal Fistulas According to whether their natural opening is below or above the anorectal ring Low level e.g., subcutaneous, low anal, sub mucous. High level – open into anal canal at or above the anorectal ring e.g., high anal, pelvirectal Park’s Classification Inter sphincteric (70%) low level Trans-sphincteric (25%) high anal fistula level anal fistula Supra sphincteric fistulae (4%). Extra sphincteric (1%) rare type include the tract passes outside all sphincter muscles to open in the rectum. Good Sall's Rule Fistulas with external opening in relation to the anterior ½ of the anus tend to be direct type. Clinical features Persistent discharge which irritates the skin and causes discomfort at the anus may be associated with pain. External opening may be seen with palpation the tracks is often palpable as cord. Investigations Proctoscopy Radiology Biopsy Surgery Fistulectomy Always sent track for biopsy. Seton placement Anal Fissure Defined as longitudinal tear in the mucosa and skin of the anal canal. Commonly posterior midline more common in female than male. Anal Fissure Lateral fissures are so rare there presence suggest specific lesions such as, Crohn’s disease, UC, TB or malignancy. Etiology Tearing of the anal lining by over distension of the anal canal during passage of large scybalous mass (stool). Tearing of anal valve or fibrous polyps. Laceration of the anal canal by sharp FB. Excessive straining during child birth. Anal Fissure The acute anal fissure if not treated becomes chronic anal fissures. As result secondary pathological changes may occurs: Chronicity A “sentinel” pile Hypertrophied anal papilla Contracture of the anus Suppuration Clinical Features Pain during and after defecation. Constipation Bleeding Discharge Findings Fissure or ulcer distal to dentate line. Sentinel Tag Hypertrophied papilla. Spasms of the internal sphincter Treatment Conservative Treatment Stool softeners (laxative) Sitz baths (10 – 15 mins.) Ointments & Suppository Treatment Surgical Treatment Dilation under anaesthesia (Anal Stretch) Fissurectomy and dorsal sphincterotomy Lateral internal sphincterotomy Rectal Prolapse Rectal prolapse occurs most often at extremes of age. Children between 1-5 years of age and elderly people. More common in female than male. Rectal Prolapse Prolapse of the rectum mainly two types: Partial or incomplete prolapse when the mucous membrane lining the anal canal protrudes through the anus only. Complete prolapse in which the whole thickness of the bowel protrudes through the anus. Etiology In children: The vertical straight course of the rectum. Reduction of supporting fat in the ischiorectal fossa. Straining at stool. Chronic cough. Adults: Partial prolapse: Advance degree of prolapsing piles. Loss of sphincter tone. Straining from urethral obstruction. Operations for fistula. Complete prolapse: generally regarded as sliding hernia of the recto vesical or recto vaginal pouch due to stretching of the levator ani from pregnancy, obesity. Clinical Features Prolapse is first noted during defecation. Discomfort during defecation. Bleeding. Mucous discharge. Bowel habit irregular and may lead to incontinence. Complications of rectal prolapse Irreducibility Infection Ulceration Severe haemorrhage from one of the mucosal vein Thrombosis and obstruction of the venous returns leading to oedema Irreducibility and gangrene Treatment In children the prolapse tends to disappear spontaneously by the age of 5 years. So conservative measures are sufficient. Conservative treatment: constipation and straining at stool are avoided and the buttocks may be strapped together to discourage prolapse during defaecation. Perirectal injection of alcohol/phenol may be used to fix the lax mucosa to underlying tissue. Prolapse in adults Partial prolapse Provided sphincter tone is satisfactory can be treated by ligature excision of prolapsed mucosa. Injections of 5% phenol in oil in submucosa. 15ml total. 10- Electrical stimulation with sphincteric exercises. Prolapse in adults Complete prolapse: Surgery always necessary, none are ideal. Thiersch’s operation Rectopexy (lock haurt) Rectosigmoidectomy (Mikulicz’s op.) Ivalon sponge rectopexy (Well’s op.) Ripstein operation Low anterior resection (minor) Anal Incontinence Normal anal continence depends on an intact spinal cord reflex acting on an adequate sphincteric mechanism under cortical inhibitory control. Causes of Incontinence Congenital malformations of the anus in which the sphincter is partially or completely lacking. Trauma. e.g accidental injury, obstetrical tears or operative trauma Causes of Incontinence Medical conditions e.g., mental deficiency, senility and spinal cord lesions. Neurological and physiological diseases e.g. spina bifida, spinal tumours and trauma. Anorectal disease e.g. rectal prolapsed, piles, chronic inflammatory bowel disease, faecal impaction, destruction as carcinoma of anus. Clinical Features The following are the clinical types: True incontinence Partial incontinence Overflow incontinence Treatment There is no satisfactory treatment for many causes of incontinence. Conservative measure: satisfactory for minor degree of incontinence e.g., anorectal lesion, faecal impaction and the sphincter tone improved by daily exercises. Operative treatment: this depend on the causes of incontinence. Treatment Thiersch’s operation Obstetrical injury (coloperincorrhaphy) Sphincteroplasty in cases of traumatic postoperative incontinence. Sphincter reefing Colostomy Anorectal Tumours Benign tumours Epithelial Tumours Anal warts (virus) Juvenile polyp Adenomatous polyps Villous papilloma Familial polyposis Pseudo polyps Endometrioma Anorectal Tumours Connective Tissue Tumours Fibrous polyp Lipoma Myoma Haemangioma Benign Lymphoma Malignant Tumours of the Anal Canal The lesion is usually squamous cell carcinoma. Rarely adenocarcinoma, malignant melanoma or basal cell carcinoma. Squamous cell carcinoma 5% of all anorectal malignancies. Arising from the stratified squamous epithelium of the lower ½ of the anal canal. It is disease of elderly. Squamous cell carcinoma more common in males. The aetiology of anal carcinoma unknown but chronic irritation or infection may be predisposing factors. Clinical Features Localized ulcer or raised growth with irregular ulcerated surface. History of bleeding. History of pain with discomfort. Tenesmus with incontinence. Discharge. Examination On palpation squamous carcinoma feels hard and woody due to invasion of perianal tissues. P/R examination may prove impossible because of stenosis or discomfort. Inguinal LN are examined carefully as they receive lymph from the lower anal canal and perianal region and may be the site of metastasis. Treatment Above the pectinate line Abdomino perineal excision Below the pertinate line local excision. If inguinal LN metastasis present should be removed by block dissection. Treatment Late cases Palliative colostomy. Radiotherapy. Rare Malignant Anal Tumours Adenocarcinoma Basal cell carcinoma Malignant melanoma Benign strictures Stricture of the anus and rectum may be: Congenital Postoperative Inflammatory Clinical features Progressive difficulty in defecation In cases of inflammatory strictures Bleeding Discharge Tenesmus Late cases subacute intestinal obstruction Diagnosis Rectal examination reveals the location type and degree of the stenosis. Proctoscopy Biopsy Treatment Dilation Superficial external proctotomy Thanks