May 2014 - Devon Sessional GPs
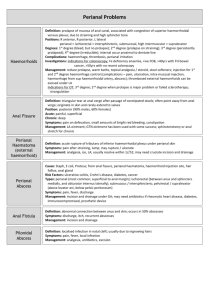
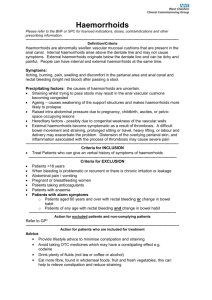
advertisement
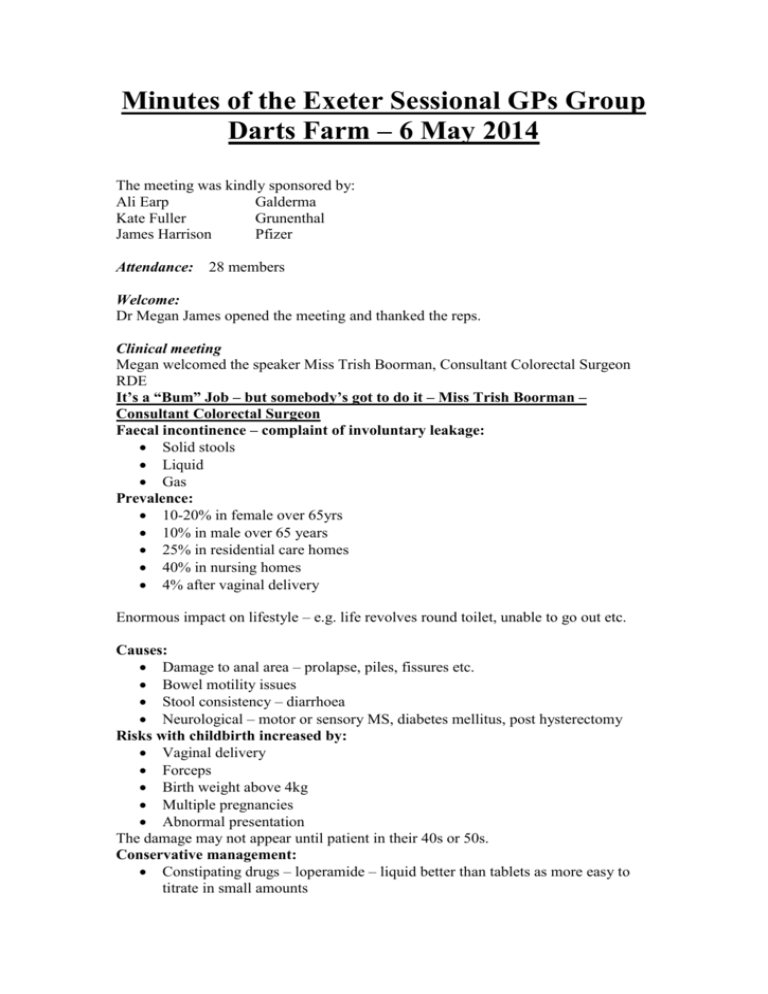
Minutes of the Exeter Sessional GPs Group Darts Farm – 6 May 2014 The meeting was kindly sponsored by: Ali Earp Galderma Kate Fuller Grunenthal James Harrison Pfizer Attendance: 28 members Welcome: Dr Megan James opened the meeting and thanked the reps. Clinical meeting Megan welcomed the speaker Miss Trish Boorman, Consultant Colorectal Surgeon RDE It’s a “Bum” Job – but somebody’s got to do it – Miss Trish Boorman – Consultant Colorectal Surgeon Faecal incontinence – complaint of involuntary leakage: Solid stools Liquid Gas Prevalence: 10-20% in female over 65yrs 10% in male over 65 years 25% in residential care homes 40% in nursing homes 4% after vaginal delivery Enormous impact on lifestyle – e.g. life revolves round toilet, unable to go out etc. Causes: Damage to anal area – prolapse, piles, fissures etc. Bowel motility issues Stool consistency – diarrhoea Neurological – motor or sensory MS, diabetes mellitus, post hysterectomy Risks with childbirth increased by: Vaginal delivery Forceps Birth weight above 4kg Multiple pregnancies Abnormal presentation The damage may not appear until patient in their 40s or 50s. Conservative management: Constipating drugs – loperamide – liquid better than tablets as more easy to titrate in small amounts Enema, suppositories or laxatives if the problem is constipation with overflow Anal plug, absorbent pads Pelvic floor – exercises or biofeedback Irrigation – takes about 20 minutes – alternate days may be enough Surgery: Sphincter repair for mechanical defect Augmentation of functionally deficient but intact sphincter – bulking agents or sacral nerve stimulation Haemorrhoid, fissure or fistula surgery Prolapse repair (Bypass – stoma – rarely used and may not stop the leak) History: Consistency Frequency Obstetric history Previous surgery for haemorrhoids etc. Perianal sepsis Abuse Examination: Tone / squeeze Rectocele, prolapse or piles – note that rectocele seen on defecating proctogram can be normal Impaction Mass Trapping of faeces in a rectocele can lead to incontinence Investigations: Endoscopy Endoanal ultrasound (EAUS) Ano-rectal physiology (ARP) ? Defecating proctogram – patient has phosphate enema to clear bowel then a mushy paste inserted via anus – films taken with patient coughing, straining, squeezing and emptying bowel – use the results in conjunction with symptoms. Haemorrhoids: Management: Diet Bowel regulation Topical treatment Injection rarely used now Banding Haemorrhoidectomy – rarely used now Haemorrhoidal artery ligation operation (HALO) +/- recto-anal repair (RAR) done under general anaesthetic – advantages – no resection, day case, repeatable, less painful, minor complications only, no urinary retention, can return to work next day. Stapled haemorrhoidopexy – done under general anaesthetic – better management of the prolapse element. Purse string suture of mucosa above dentate line and a ring of tissue is taken out. Advantages – infrequent and minor complications, less pain than haemorrhoidectomy, quicker recovery, good aesthetic results, patients very satisfied. Management of prolapsed thrombosed internal haemorrhoids: Analgesia Local anaesthetic cream Ice packs Tip bed head down Laxatives Topical diltiazem or GTN It takes 3-4 days for recovery to begin and two weeks before settled completely – surgery not done as results in sphincter damage in 60% Other painful conditions: Abscess SCC Fissure – conservative management is diet, bowel regulation, topical GTN or diltiazem. If no help then options are botox injection, fissurectomy with advancement flap or rarely lateral sphincterotomy Perianal haematoma – differentiated from thrombosed pile as covered by skin rather than mucosa, a clot under the anal verge. Managed with analgesia and laxatives. Sphincter augmentation: Bulking agents – solesta – a submucosal injection to reform the haemorrhoidal cushions. 3 year data show sustained improvement in continence. Sacral nerve stimulation – stimulate sacral nerve to modify neural reflexes that influence lower bowel, anal sphincter and pelvic floor. A test wire inserted as day case procedure is trialled for 2-3 weeks. If successful then permanent implant inserted with a controller which can be used to change the stimulation level. It lasts 8-10 years, can be life changing. Patients carry a pacemaker card – x ray at airport affects it, cremation rules apply as per pacemaker. Posterior tibial nerve stimulation (PTNS) – non-invasive, low or no risk, outpatient procedure, no embarrassment, little training needed, nurse led procedure, time effective – 30 mins per week for 12 weeks and then top up may be needed, 66-82% success rate. Rectal prolapse: Complete / full thickness or occult Can bleed or ulcerate Very elderly can have a minimal procedure – e.g. Delorme’s procedure – done via rectum but does require general anaesthetic. Has a high recurrence rate so not suitable in young. Permacol “Thiersch” wire can be used in very frail – local anaesthetic Anterior Delormes is a simple repair Stapled trans anal rectal resection (STARR) – done less often now Laparoscopic ventral mesh rectopexy is a good method Perianal itch: Eczema or psoriasis Allergic dermatitis Infections Systemic disease – e.g. diabetes mellitus Foods – caffeine, tomatoes, citrus Medications – steroids, antibiotics Idiopathic Perianal conditions including haemorrhoid, fissure, tumour Management – water to wash, bidets, wipe with non-perfumed wet wipe then dry carefully, wear gloves at night, cotton underwear. Housekeeping Megan thanked Miss Boorman and reminded members to sign the attendance register. Megan also asked that anyone who wishes to express an interest in a CPR session should e mail using the web site contact. The session will only be viable if there are at least fifteen participants – there will be a charge for the session. Future ESGPG Meetings 3rd June 2014 – Functional Illness and Medically Unexplained Symptoms, Dr. Jo Bromley, Consultant Psychiatrist 1st July 2014 – Gastroenterology update, Dr. Shyam Prassad, Consultant Gastroenterologist 5th August 2014 - SUMMER SOCIAL EVENT – Details to follow 2nd September 2014 – The Movement Disorders Clinic Dr. Sarah Jackson 7th October 2014 - Hospice Update Dr. Becky Baines 4th November 2014 - Contraceptive Update Dr. Jane Bush Lead for contraceptive services, NDHC 2nd December 2014 - Diabetes update, Dr. Tom Fox Consultant endocrinologist Meeting time Please note that the meetings are now scheduled to start at 7pm with the guest speaker planned to commence at 7.30pm. Committee Contacts Dr Megan James (chairman) Dr Laura Davies (website co-ordinator) Dr Lynne Reid (appraisal support co-ordinator) Dr Nimita Gandhi (educational co-ordinator) Dr Sarah Hemingway (funding co-ordinator) Dr Anna Beazley (treasurer) Dr Kathryn Shore (minutes’ secretary) Dr Clair Homeyard (social secretary) Dr Megan James (LMC link) meganbyles1@gmail.com ledavies@doctors.org.uk lynnereid@doctors.org.uk nimitagandhi@nhs.net sarahhemingway@doctors.org.uk abeazley22@outlook.com kathrynshore@btinternet.com clair_homeyard@hotmail.com meganbyles1@gmail.com