5.3 Components of Inpatient Stroke Rehabilitation
advertisement

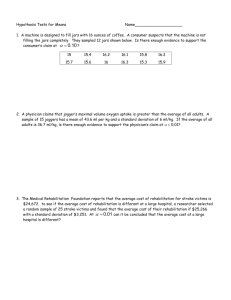
Canadian Best Practice Recommendations for Stroke Care Canadian Best Practice (Updated 2008) Recommendations for Stroke Care: 2008 Section # 3 Recommendation 5: Management Hyperacute Stroke Stroke Rehabilitation and Community Reintegration 5.0 Stroke Rehabilitation and Community Reintegration 5.1 Initial stroke rehabilitation assessment 5.2 Provision of inpatient stroke rehabilitation 5.3 Components of inpatient stroke rehabilitation 5.4 Outpatient and community-based rehabilitation 5.5 Follow-up and community reintegration 5.1 Initial Stroke Rehabilitation Assessment All persons with stroke should be assessed for their rehabilitation needs. All people admitted to hospital with acute stroke should have an initial assessment by rehabilitation professionals as soon as possible after admission; preferably within the first 24-48 hours. All people with acute stroke with any residual strokerelated impairments who are not admitted to hospital should have a comprehensive outpatient assessment for functional impairment, preferably within two weeks. 5.1 Initial Stroke Rehabilitation Assessment Functional assessment should include: A cognitive evaluation Screening for depression Screening of fitness to drive Functional assessments for potential rehabilitation treatment Clinicians should use standardized, valid assessment tools to evaluate the patient’s stroke-related impairments and functional status. Survivors of a severe or moderate stroke should be reassessed at regular intervals for their rehabilitation needs. Outcome Tools for Stroke Rehabilitation Recommended by SCORE/CSQCS Stroke Rehabilitation Outcomes Panel Domain Selected Measure Measures of Stroke Severity Orpington or NIH Stroke Scale Medical Conditions Charlson Co-Morbidity Upper Extremity Structure and Function Chedoke-McMaster Assessment (CMSA) Lower Extremity Chedoke-McMaster Stroke Assessment Spasticity Modified Ashworth + Spasticity Subscale of CMSA Bayley, Lindsay et al, Canadian Stroke Network, 2006 Outcome Tools for Stroke Rehabilitation Recommended by SCORE/CSQCS Stroke Rehabilitation Outcomes Panel Domain Selected Measure Visual Perception a) b) c) d) Language a) Screening in acute and follow-up: Frenchay Aphasia Screening Test b) Rehabilitation: Boston Diagnostic Aphasia Assessment Cognition a) MoCA b) Five Minute protocol from the MoCA c) Screening MMSE + Line Bisection+Semantic Fluency Bayley, Lindsay et al, Canadian Stroke Network, 2006 Comb and Razor Behavioural Inattention Test Line Bisection Alternates: Rivermead, OSOT,MVPT Outcome Tools for Stroke Rehabilitation Recommended by SCORE/CSQCS Stroke Rehabilitation Outcomes Panel Domain Selected Measure Arm Function a) Chedoke Arm and Hand Activity Inventory b) Box and Block c) Nine Hole Peg Test Walking/Lower Extremity a) b) c) d) Balance Berg Balance Scale Functional Communication Amsterdam (ANELT) Alternate: ASHA-Functional Assessment of Communication of Activities of Daily Living (ASHA-FACS) Bayley, Lindsay et al, Canadian Stroke Network, 2006 Chedoke Inventory Timed up and Go 6 Minute walk test Alternate-Rivermead Mobility Index Outcome Tools for Stroke Rehabilitation Recommended by SCORE/CSQCS Stroke Rehabilitation Outcomes Panel Domain Selected Measure Self-Care Activities of Daily Living Functional Independence Measure (FIM) Instrumental Activities of Daily a) Reintegration to Normal Living Living Index b) Leisure section of the LIFE-H Participation Stroke Impact Scale Bayley, Lindsay et al, Canadian Stroke Network, 2006 System Implications Adequate complement of experienced clinicians Clear referral processes Screening and assessment tools Access to follow-up services Strong partnerships Performance Measures Median time from hospital admission for stroke to initial rehabilitation assessment for each of the rehabilitation disciplines. Proportion of acute stroke patients discharged from acute care to inpatient rehabilitation. % of stroke patients discharged to the community who receive a referral for outpatient rehabilitation before discharge from hospital. Median time between referral for outpatient rehabilitation to admission to a community rehabilitation program. 5.2 Provision of Inpatient Stroke Rehabilitation * All patients with stroke who are admitted to hospital and who require rehabilitation should be treated in a comprehensive or rehabilitation stroke unit by an interdisciplinary team. Post-acute stroke care should be delivered in a setting in which rehabilitation is formally coordinated and organized. All patients should be referred to a specialist rehabilitation team on a geographically defined unit as soon as possible after admission. Pediatric acute and rehabilitation stroke care should be provided on a specialized pediatric unit. 5.2 Provision of Inpatient Stroke Rehabilitation Post-acute stroke care should be delivered by a variety of treatment disciplines, experienced in providing post-stroke care, to ensure consistency and reduce the risk of complications. The interdisciplinary rehabilitation team may consist of: Physician Nurse Physiotherapist Occupational therapist Speech-language pathologist Pharmacist Psychologist Recreation therapist Patient/family caregivers For children, also includes educators and child-life workers. 5.2 Provision of Inpatient Stroke Rehabilitation The interdisciplinary rehabilitation team should assess patients within 24-48 hours of admission and develop a comprehensive individualized rehabilitation plan which reflects severity of the stroke and needs and goals of the stroke patient. Patients with moderate or severe stroke who are rehabilitation ready and have goals should be given an opportunity to participate in inpatient stroke rehabilitation. 5.2 Provision of Inpatient Stroke Rehabilitation Stroke unit teams should conduct at least one formal interdisciplinary meeting a week to discuss progress and problems, rehabilitation goals and discharge arrangements for patients on the unit; individualized rehabilitation plans should be regularly updated based on patient status reviews. Clinicians should use standardized, valid assessment tools to evaluate the patient’s stroke-related impairments and functional status. Where admission to a stroke rehabilitation unit is not possible, a less optimal solution is inpatient rehabilitation on a mixed rehabilitation unit. System Implications Timely access to specialized inpatient rehabilitation services. Adequate number of geographically defined stroke units with critical mass of trained staff; interdisciplinary team during the rehabilitation period. Clinicians with expertise in stroke rehabilitation. Timely access to appropriate type and intensity of rehabilitation professionals. Optimization of strategies to prevent complications and recurrence of stroke. Consistent implementation of evidence-based best practices for stroke rehabilitation across the continuum of care. Performance Measures Number of stroke patients treated in a geographically defined stroke rehabilitation unit at any time during their inpatient rehabilitation phase following an acute stroke event. Final discharge disposition for stroke survivors following inpatient rehabilitation: % discharged to original place of residence % discharged to long-term care facility or nursing home % requiring readmission to an acute care hospital for stroke-related causes. Performance Measures Number of stroke patients assessed during inpatient rehabilitation by: Physiotherapist Occupational therapist Speech-language pathologist Social worker Proportion of total time during inpatient rehabilitation following acute event spent on stroke rehabilitation unit. Frequency, duration and intensity of therapies received from rehabilitation professionals while in an inpatient rehabilitation setting. Change in functional status measured with a standardized measurement tool, from time of admission to an inpatient rehabilitation unit for stroke patients to the time of discharge. 5.3 Components of Inpatient Stroke Rehabilitation All patients with stroke should begin rehabilitation therapy as early as possible once medically stable. Patients should receive intensity and duration of clinically relevant therapy defined in their individualized rehabilitation plan and appropriate to their needs and tolerance levels. Stroke patients should receive, through an individualized treatment plan, a minimum of one hour of direct therapy by the interprofessional stroke team for each relevant core therapy, for a minimum of five days a week based on individual tolerance, with duration of therapy being dependant on stroke severity. 5.3 Components of Inpatient Stroke Rehabilitation The team should promote the practice of skills gained in therapy into patient’s daily routine in a consistent manner. Therapy should include repetitive and intense use of novel tasks that challenge patient to acquire necessary motor skills to use the involved limb during functional tasks and activities. Stroke unit teams should conduct at least one formal interdisciplinary meeting a week at which patient problems are identified, rehabilitation goals set, progress monitored and support after discharge planned. 5.3 Components of Inpatient Stroke Rehabilitation The care management plan should include a pre-discharge needs assessment. Elements of discharge planning should include a home visit by a health care professional. Ideally before discharge, to assess home environment and suitability for safe discharge. Determine equipment needs and home modifications Begin caregiver training for how patient will manage activities of daily living and instrumental activities of daily living in their environment. System Implications Timely access Critical mass of trained clinicians Protocols and partnerships Strategies to prevent recurrence Initiatives for caregivers Ability to reassess as required Selected Performance Measures Length of time from stroke admission in an acute care hospital to assessment of rehabilitation potential by a rehabilitation health care professional. Length of time between stroke onset and admission to stroke inpatient rehabilitation. Number or percentage of patients admitted to a coordinated stroke unit — either a combined acute care and rehabilitation unit or a rehabilitation stroke unit in an inpatient rehabilitation facility — at any time during their hospital stay (acute and/or rehabilitation). Selected Performance Measures Change (improvement) in functional status scores using a standardized assessment tool from admission to an inpatient rehabilitation program to discharge Final discharge disposition for stroke survivors following inpatient rehabilitation: percentage discharged to their original place of residence, percentage discharged to a longterm care facility or nursing home, percentage discharged to supportive housing or assisted living. Percentage of patients requiring readmission to an acute care hospital for stroke-related causes. 5.4 Outpatient and Community-Based Rehabilitation After leaving hospital, stroke survivors must have access to specialized stroke care and rehabilitation services appropriate to their needs (acute and/or inpatient rehabilitation). Early supported discharge services and transition planning should be provided by a well-resourced, coordinated specialist interdisciplinary team with ageappropriate expertise. These are an acceptable alternative to extended in-hospital rehabilitation and can reduce length of stay for selected patients. Patients requiring early supported discharge services should not be referred to generic (non-specific) community services. 5.4 Outpatient and Community-Based Rehabilitation People who have difficulty in activities of daily living, including self care, productivity and leisure should receive occupational therapy or multi-disciplinary interventions targeting activities of daily living. Multifactorial interventions provided in the community including an individually prescribed exercise program, may be provided for people who are at risk for falling, in order to prevent or reduce the number and severity of falls. 5.4 Outpatient and Community-Based Rehabilitation People with difficulties in mobility should be offered an exercise program and monitored throughout the program. 5.4 Outpatient and Community-Based Rehabilitation Patients with aphasia should be taught supportive conversation techniques. Patients with dysphagia should be offered swallowing therapy and opportunity for reassessment as required. 5.4 Outpatient and Community-Based Rehabilitation Children affected by stroke should be offered advice on and treatment aimed at achieving play, self-care, leisure and school-related skills that are developmentally relevant and appropriate in their home, community and school environment. System Implications Organized and accessible stroke care in communities Increased number of experienced clinicians Access to services in the community Early supported discharge services Support for caregivers Long-term rehabilitation services widely available in nursing and continuing care facilities, and in outpatient community programs. Selected Performance Measures Percentage of stroke patients discharged to the community who receive a referral for ongoing rehabilitation before discharge from hospital (acute and/or inpatient rehabilitation). Change in functional status scores, using a standardized measurement tool, for stroke survivors engaged in community rehabilitation programs. Number of stroke patients assessed by physiotherapy, occupational therapy, speechlanguage pathologists and social workers in the community 5. 5 Follow-Up and Community Reintegration People with stroke living in the community should have regular and ongoing follow-up assessment to assess recovery, prevent deterioration and maximize functional outcome. Post acute stroke patients should be followed up by a primary care provider to address: Stroke risk factors Ongoing rehabilitation needs Continuation of treatment of comorbidities and other sequelae of stroke Stroke survivors and their caregivers should have psychosocial and support needs reviewed on a regular basis. 5.5 Follow-Up and Community Reintegration People living in the community who have difficulty with activities of daily living should have access, as appropriate, to therapy services to improve or prevent deterioration in activities of daily living. Identification and Management of Post-Stroke Depression (Rec. # 6.2) should also be observed as part of follow-up and evaluation of stroke survivors in the community. Any stroke survivor with declining activity at six months or later after stroke should be assessed for appropriate targeted rehabilitation. 5.5 Follow-Up and Community Reintegration Infants and children, in whom new motor, language or cognitive deficits emerge over time, require ongoing follow-up and assessment throughout their development. Pediatric stroke survivors in the community should have ongoing assessments of education and vocational needs throughout their development. 5.5 Follow-Up and Community Reintegration Stroke survivors and families should be provided with timely, up-to date information in conjunction with opportunities to learn from members of the interdisciplinary team and other appropriate community service providers. Simple information provision alone is not sufficient. Patients and caregivers should be offered education programs to assist them in adapting to their new role. System Implications Assistance for stroke survivors and families Stroke care expertise and education in community and long-term care settings Support including community programs, respite care and education to support caregivers Social supports and re-engagement strategies Selected Performance Measures Proportion of patients who are discharged from acute care who receive a referral for home care or community supportive services. Median wait time from referral to admission to nursing home or long-term care facility. Number of visits to an emergency department within specified time frames. Number of readmissions from stroke rehabilitation to acute care for strokerelated causes Implementation Tips Form a working group, consider both local and regional stakeholders and include a stroke survivor and family. Complete a gap analysis to compare current practices using the Canadian Best Practice Recommendations: 2008 Gap Analysis Tool. Identify strengths, challenges, opportunities. Identify 2-3 priorities for action. Implementation Tips Identify local and regional champions. Identify professional education needs and develop a professional education learning plan. Consider local or regional workshops to focus on Stroke Rehabilitation and Community Reintegration. Access resources such as CSS experts, Heart and Stroke Foundation, provincial contacts, stroke recovery groups. www.canadianstrokestrategy.ca www.cmaj.ca