Chapter 17
advertisement

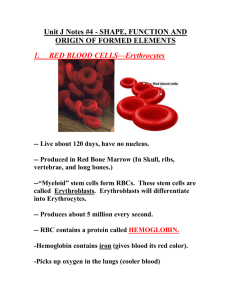
Chapter 17 BLOOD Blood Composition & Functions • Blood is the ONLY fluid tissue (connective) – Why is a fluid considered a tissue? • Composed of formed elements suspended in plasma Fun Facts! • • • • • The color of blood depends on the amount of Oxygen it is carrying Scarlet = Oxygen Rich Dark Red = Oxygen Poor Blood accounts for approx. 8% of your body weight Average adult male has 5-6L Average adult female has 4-5L 3-4 pounds of “baby weight” can be attributed to increased blood volume Functions of blood Distribution – Delivers oxygen and nutrients to the cells of the body – Transports metabolic waste products to lungs (CO2) and kidneys (nitrogenous wastes) for elimination – Transports hormones Regulation – Maintains body temperature – Maintains pH in body tissues – Maintains fluid volume in the circulatory system Protection – Prevents catastrophic blood loss – Prevents infection Blood Plasma • Straw-colored sticky fluid that is 90% water • Remaining 10% contains proteins (most abundant 8%), nitrogenous wastes, nutrients, electrolytes, respiratory gases, hormones • Albumin makes up 60% of plasma protein and is vital for helping to keep water in the blood stream • Plasma proteins are not the same proteins used by your cells for energy! • Fibrinogen (4% of plasma proteins) is the plasma protein that facilitates blood clot formation Check Point!!!! • What is the hematocrit? What is a normal value? The % of blood made up by erythrocytes approx. 45% is the normal range • List 2 protective functions of blood Blood clotting and protection from infection • Are plasma proteins used as fuel for body cells? No…they serve other functions such as transport and fluid volume regulation Formed Elements • Erythrocytes aka: Red Blood Cells (RBCs) • Not a true cell • Does not contain a nucleus • Leukocytes aka: White Blood Cells (WBCs) • Platelets aka: Thrombocytes • Not a true cell • Does not contain a nucleus • Actually only a cell fragment Erythrocytes (RBCs) • Small biconcave disc shaped cells with depressed centers • Lack a nucleus (anucleate) and organelles • Contain primarily hemoglobin (97%) which is the protein that binds to and transports respiratory gases • Since they do not have mitochondria, they generate ATP anaerobically and do not consume any of the oxygen they carry • RBCs are the major factor that contributes to blood viscosity RBCs and Hemoglobin… • Transportation of respiratory gases O2 and CO2 bound to hemoglobin • Hemoglobin is made up of the protein globin which is bound to a heme group • Globin consists of 4 polypeptide chains each bound to a heme group • Each heme group contains an iron atom • Each hemoglobin can transport 4 molecules of oxygen because each iron atom can bind with one oxygen molecule • A single RBC contains about 250 million hemoglobin molecules so each little cell can hold around a billion molecules of oxygen! Hemoglobin inside RBC Function of the RBCs • Oxygen loading occurs in the capillaries surround the alveoli of the lungs • Oxygen diffuses through the capillaries and binds to the iron attached to the hemoglobin of oxygen poor RBCs and becomes bright red oxyhemoglobin • After the RBC leaves the lungs and reaches tissues that need O2 the oxygen detaches from the iron resulting in deoxyhemoglobin and becomes dark red again Function of the RBCs • About 20% of CO2 carried in the blood binds to the globin’s amino acids rather than the heme group • This usually occurs in the deoxyhemoglobin state when the cell is oxygen poor • CO2 loading occurs in the tissues where it is then carried back to the lungs to be eliminated from the body Hematopoiesis aka: production of blood cells • Occurs in the red bone marrow • In adults it occurs primarily in the axial skeleton and flat portions of the girdles as well as the proximal epiphyses of the humerus and femur • Each type of blood cell is produced in different numbers depending on the bodies needs at the time • The entire process takes about 15 days • All the formed elements of blood take place and originate from the same stem cells (hemocytoblasts) which later become differentiated into a specific type of blood cell • Reticulocytes are immature RBCs and account for approximately 1-2% of all erythrocytes in healthy people • Reticulocyte counts below or above this percentage rate indicate abnormal rates of RBC function Erythropoiesis Red Blood Cell formation • rate of RBC production is controlled by hormone called Erythropoietin (EPO) • erythropoietin is produced by the kidneys and stimulated by blood level of oxygen low 02 = more erythropoietin high O2 = less erythropoietin Erythropoiesis Red Blood Cell formation The drop in normal blood oxygen levels that triggers EPO formation can result from: – Reduced numbers of RBCs due to hemorrhage or excessive RBC destruction – Insufficient hemoglobin per RBC (iron deficiency) – Reduced availability of oxygen, i.e. high altitudes or respiratory illness such as pneumonia Note: low oxygen levels alone do not activate the bone marrow, rather it stimulates the kidneys to release more EPO EPO: The Good, The Bad, & The Ugly Renal dialysis patients whose kidneys fail to produce enough erythropoietin to support adequate RBC formation often times have hematocrits less than half of healthy individuals. Genetically engineered injectable EPO can dramatically help patients like this in increase their RBC formation and improve their quality of life In groups of 2, please answer the following questions and turn them in with both names on the paper What symptoms do you think a patient with a low hematocrit would have? What possible reasons do you think someone would have to abuse this medication? What possible complications do you think could arise from this abuse? Destruction of RBCs • Due to being anucleate RBCs only have a lifespan of 100-120 days • As they age, the become more inflexible and fragile and hemoglobin begins to deteriorate • Old cells are often destroyed by macrophages • The iron core of the heme group is saved and stored for reuse the rest is broken down into bilirubin • Most broken down bilirubin leave the body through the feces and attributes to the brown coloring of fecal material • Buildup of excessive amounts of bilirubin in the blood can lead to jaundice Erythrocyte Disorders Anemia – “Lacking Blood” • A sign of a disorder rather than a disease of its own • Condition in which the blood has abnormally low oxygen-carrying capacity • People with anemia often are fatigued, pale, short of breath, and chilly • Many different types of anemia with different causes Causes of Anemia 1. An insufficient number of red blood cells Common Causes: • Hemorrhage – usually due to trauma or illness that causes internal bleeding i.e. gastric ulcers • Excessive blood cell destruction (hemolytic anemia) – RBC’s rupture prematurely. Can be caused by hemoglobin abnormalities, transfusion of mismatched blood, or bacterial or parasitic infections • Bone marrow failure (aplastic anemia)- results from the destruction or inhibition of the red bone marrow. Can be caused by certain drugs or chemicals, radiation, or viruses. Often times the cause may be unknown. Blood transfusions will help until a bone marrow transplant can occur Causes of Anemia 2. Low Hemoglobin Content - Occurs when hemoglobin molecules are normal, but RBCs contain fewer than usual • Iron deficiency anemia – usually a result of hemorrhagic anemias, but may occur due to low intake of iron-rich foods or impaired iron absorption • Pernicious anemia – due to a deficiency of vitamin B12 which is found in meats, poultry, and fish so is not usually a dietary disorder except for strict vegetarians. It is usually caused by a lack of intrinsic factor which is produced in the stomach and allows for vitamin B12 absorption. Causes of Anemia 3. Abnormal hemoglobin • Thalassemia- typically found in those of Mediterranean decent (Greeks and Italians). One of the globin chains is absent or faulty, and the RBCs are thin, fragile, and deficient in hemoglobin • Sickle-cell Anemia– caused by a change in one of the 146 amino acids in the beta chain of the globin molecule. Causes the beta chains to link together under low-oxygen conditions. Causes the cells to become sickle shaped when they unload O2 molecules or when O2 content in blood is lower than normal. Cells are fragile and lyse easily and cause the blood vessels to clog. Depending on where the crisis is occuring patients may experience severe pain, shortness of breath, infection, or stroke. Occurs primarily in African Americans but can be seen in other ethnicities as well Polycythemia…Too much of a good thing! • Excessive amount of RBCs that increase blood viscosity, causing it to sludge and flow slowly – Increases risk for stroke and heart failure • Secondary polycythemia- occurs when less oxygen is available or EPO production increases • Blood doping – dangerous practice used by some athletes competing in aerobic events is an artificially induced polycythemia Leukocytes (WBC’s) • The only formed elements that are complete cells • Account for less than 1% of total blood volume • Vital for our defense against disease by protecting us from bacteria, viruses, parasites, toxins, and tumor cells • WBCs only use the circulatory system as a method of transportation • WBCs are able to travel out of the blood vessels (diapedesis) and create a defense where they are needed. • Capable of ameboid movement both in the blood vessels and in the tissues Leukocytes Grouped into 2 main categories Granulocytes – Contain specialized membrane-bound cytoplasmic granules – Include neutrophils, eosinophils, and basophils – PHIL eats Grains Agranulocytes – lack obvious granules – Include lymphocytes and monocytes – No grains in sight (cyte) Types of Leukocytes in order of abundance Remember! Never Let Monkeys Eat Bananas Neutrophils Leukocytes Monocytes Eosinophils Basophils Neutrophils • Granulocyte • Accounts for 50-70% of WBCs • Named for the fact that they are “neutral” when stained and the granules in the plasma pick up both red and blue stain creating a lilac appearance of the plasma • Multi-lobed nucleus with 2-5 lobes • 1st cells to arrive to an injury site • Actively phagocytic and partial to bacteria • Most have a short lifespan (10 hours) and upon their death, they release chemicals that attract new neutrophils • A mixture of dead neutrophils, cellular debris, and other waste products form the pus associated with infected wounds Eosinophils • • • • Granulocyte Account for 2-4% of all leukocytes Bi-lobed nucleus Named because of the deep red stain the granules take on with acid dye (eosin) • Best defense cell for parasitic worms (flatworms & roundworms) • Attack objects that are coated with antibodies • Their numbers increase with parasitic infections and allergic reactions Basophils • Granulocytes • Rarest of the WBCs and account for less than 1% of the WBC count • Granules stain a dark blue with basic dyes • Granules contain heparin (prevents clotting) and histamine (dilates blood vessels and produces inflammation) that are released at an injury site which increases WBC response Lymphocytes • • • • Agranulocytes Account for 25% or more of the WBC population 2 types (T lymphocytes & B lymphocytes) T lymphocytes act directly against virus-infected cells and tumor cells • B lymphocytes give rise to plasma cells that produce antibodies • When stained they have a very large dark blue stained nucleus that makes up most of the cell volume • Few lymphocytes circulate in the blood and are most frequently found in lymph tissue Monocytes • • • • Agranulocytes Account for 3-8% of all WBCs Larges of the WBCs U or Kidney shaped purple staining nucleus with lots of plasma that stains pale blue • Travel to the tissues and transform into Macrophages • Defend against viruses, bacterial parasites, and chronic infections • Activate lymphocytes to mount the immune response Check Point!!!! • Identify the 5 types of Leukocytes Neutrophils Lymphocytes Monocyte Eosinophil Basophils • Which type of WBC would you expect to find in an infected cut? Neutrophils , they are usually the first to arrive on scene and actively phagocytize bacteria • Which type of WBC would you find in elevated numbers in a person producing large amounts of circulating antibodies to combat a virus? Lymphocytes usually attack viruses and produce antibodies in response to infections White Blood Cell Count Normal White Count: 4800-10,800/µL Leukopenia- indicates a reduced number of WBCs. May be caused by diseases, medications, and genetic deficiencies. Leukocytosis- excessive numbers of WBCs due to any cause Leukemia- indicated in extreme leukocytosis with white counts in excess of 100,000/µL or more Leukemias • Cause is not well understood, but it is believed to be a combination of genetic and environmental factors • In all leukemias, the red bone marrow becomes almost completely occupied by cancerous leukocytes and immature WBCs that flood the blood stream • Other blood cells are crowded out so severe anemia and bleeding problems result • Other signs and symptoms include: • • • • • • • • • Fever or chills Persistent fatigue, weakness Frequent or severe infections Losing weight without trying Swollen lymph nodes, enlarged liver or spleen Easy bleeding or bruising Recurrent nosebleeds Excessive sweating, especially at night Bone pain or tenderness Leukemias • The leukemia is named for the type of abnormal cell involved Ex. Myelocytic leukemia Lymphocytic leukemia Acute leukemia. In acute leukemia, the abnormal blood cells are immature blood cells (blasts). They can't carry out their normal functions, and they multiply rapidly, so the disease worsens quickly. Acute leukemia requires aggressive, timely treatment. Chronic leukemia. There are many types of chronic leukemias. Some produce too many cells and some cause too few cells to be produced. Chronic leukemia involves more mature blood cells. These blood cells replicate or accumulate more slowly and can function normally for a period of time. Some forms of chronic leukemia initially produce no early symptoms and can go unnoticed or undiagnosed for years. • All are fatal if not treated or if treatment is ineffective Leukemia The major types of leukemia are: • Acute lymphocytic leukemia (ALL). This is the most common type of leukemia in young children. ALL can also occur in adults. • Acute myelogenous leukemia (AML). AML is a common type of leukemia. It occurs in children and adults. AML is the most common type of acute leukemia in adults. • Chronic lymphocytic leukemia (CLL). With CLL, the most common chronic adult leukemia, you may feel well for years without needing treatment. • Chronic myelogenous leukemia (CML). This type of leukemia mainly affects adults. A person with CML may have few or no symptoms for months or years before entering a phase in which the leukemia cells grow more quickly. Platelets • Cell fragments of much larger cells called megakaryocytes • Essential for the clotting process that occurs with blood vessel damage • Form a temporary plug that helps seal the damaged vessel • Anucleate so they age quickly and degenerate if not used in about 10 days Hemostasis the stoppage of bleeding • Fast, localized, and carefully controlled response • Involves many clotting factors normally present in the plasma as well as extra substances that are release by the platelets and injured tissue cells • Three step process 1. Vascular spasm 2. Platelet plug formation 3. Coagulation, or blood clotting Vascular Spasm (Blood vessel constriction) Caused by: • Chemicals released into the blood stream by the cells of the torn vessel, platelets, and as a reflex initiated by pain receptors • As tissue damage increases, so too does vascular spasm • Important response because strongly constricted arteries can significantly reduce blood loss for up to 20-30 minutes allowing time for a platelet plug to form and for coagulation to occur Platelet Plug Formation • Intact vessels prevent platelets from sticking together by producing chemicals that prevent platelet aggregation • Once the tissue is damaged, collagen fibers of the damaged tissue are exposed and platelets adhere to them • Platelets swell, form spiked projections, become stickier, and release chemical messengers that attract more platelets and increase vascular constriction • More platelets = more chemicals = more platelets and so on…(think back to semester one…what type of a feedback mechanism is this?) Coagulation (blood clotting) • Reinforces the platelet plug with fibrin threads that act as a molecular glue • Blood is transformed from a liquid to a gel in a multi-step process than include chemicals called clotting factors and procoagulants • There are 12 different clotting factors which include Ca+ ions • Coagulation occurs in 3 distinct phases about 30 seconds after damage has occurred • Most of the clotting factors are produced by the liver Phases of Coagulation Phase 1: Prothrombin Activator Formation (2 pathways) • Intrinsic pathway – Triggered by negatively charged surfaces such as activated platelets, collagen, or glass – Called intrinsic because the factors needed for clotting are present within (intrinsic to) the blood – Slower because it has many intermediate steps • Extrinsic Pathway – Triggered by exposing blood to tissue factor (TF) found in the tissues underneath the damaged endothelium – Called extrinsic because the tissue factor it requires is found outside of blood – Faster because it bypasses several steps of the intrinsic pathway. Phases of Coagulation Phase 2: Common Pathway to Thrombin • Prothrombin activator initiates (catalyzes) the transformation of the plasma protein prothrombin to the active enzyme thrombin Phases of Coagulation Phase 3: Common Pathway to the Fibrin Mesh • Thrombin initiates the transformation of fibrinogen to fibrin • Fibrin molecules join together to form long hair-like insoluble fibrin strands • Fibrin strands glue the platelets together and make a web that forms the structural basis of the clot • Fibrin makes plasma become gel-like and traps formed elements that try to pass through it • Fibrin + calcium ions activate factor XIII that binds fibrin strands tightly together which strengthens the clot • Clot formation is usually complete within 3-6 minutes after blood vessel damage Human Blood Groups • RBC plasma membranes are covered in antigens called agglutinogens • ABO blood groups are based on the presence or absence of 2 agglutinogens (type A and type B) • Depending on which of these you inherit, your blood type will be either A, B, AB, or O • O blood group has neither agglutinogen and is the most common blood group • AB with both antigens is the most rare • The presence of either the A antigen or the B antigen alone results in either A type or B type blood Human Blood Groups • Plasma contains antibodies called agglutinins which seek out and destroy any cells that carry agglutinogens (antigens) that are not found on a person’s own RBCs • Newborns lack these antibodies, but they begin to appear within 2 months • A person with AB blood type contains neither antibody • Type O blood contains both antibodies Homework!!!!! See if your parents know what their blood type is…if they both know, then make and educated guess at to what your blood type could be!