Male reproductive system
advertisement
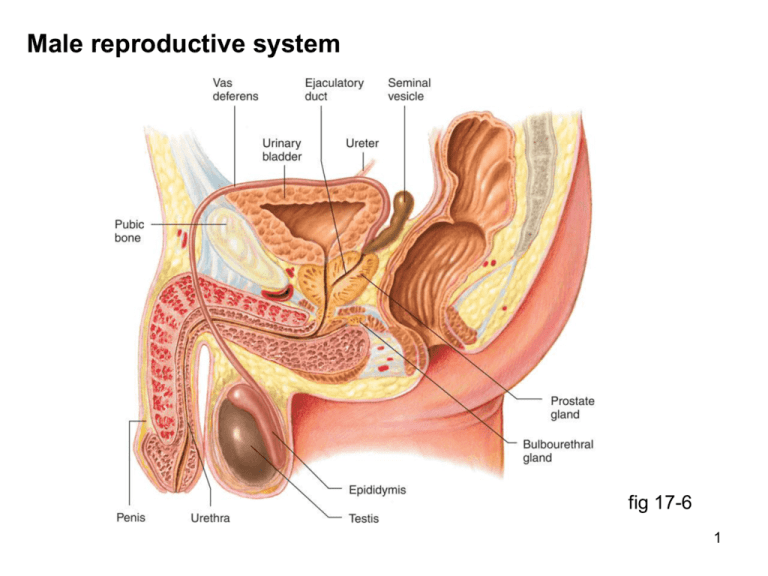
Male reproductive system fig 17-6 1 Testis & seminiferous tubules fig 17-5 2 Spermatogenesis fig 17-7 3 Structure of seminiferous tubules fig 17-4 4 Spermatogenesis fig 17-9 5 Spermatogenesis (notes) Spermatogenesis begins at puberty Spermatogonia primary spermatocytes mitotic division, occurring in basal compartment primary spermatocytes cross tight junction to adluminal compartment Primary spermatocyte secondary spermatocytes first meiotic division, occurring in adluminal compartment Secondary spermatocyte spermatids second meiotic division, adluminal compartment Spermatids spermatozoa no division, maturation process 6 Sertoli cell (functions) 1. form barrier between plasma & mature sperm 2. nourish developing sperm 3. secrete luminal fluid & androgen binding protein 4. respond to FSH & testosterone to stimulate spermatogenesis 5. secrete inhibin which inhibits release of FSH 6. absorb & destroy defective sperm 7 Structure of spermatozoon fig 17-8 Acrosome: contains enzymes involved in fertilization process 8 Erection & ejaculation fig 17-10 9 Erection, emission & ejaculation (notes) Erection: stimuli from CNS systems, penile mechanoreceptors parasympathetic nerves (nonadrenergic noncholinergic) release NO NO stimulates soluble guanylate cyclase in penile arteriole smooth muscle cyclic GMP relaxes smooth muscle & increases blood flow increased blood flow into 2 corpora cavernosa & corpus spongiosum erection compresses venous outflow & maintains erection Emission: (movement of seminal fluid into prostatic urethra) sympathetic NS peristaltic contractions of vas deferens Ejaculation: semen entering prostatic urethra spinal reflex involving somatic NS & skeletal muscle of perineal floor 10 Male hormonal control fig 17-11 11 GnRH, LH, FSH (notes) Gonadotropin releasing hormone (GnRH) secreted by hypothalamus into hypothalamo-hypophyseal portal system increases at puberty, ? less sensitivity to testosterone feedback pulsatile release ~90 min pulsatile LH & FSH release Luteinizing hormone (LH) from anterior pituitary, stimulated by GnRH, inhibited by testosterone acts on Leydig cells of testis testosterone release Follicle stimulating hormone (FSH) from anterior pituitary, stimulated by GnRH, inhibited by inhibin acts with testosterone on Sertoli cells to promote spermatogenesis Note: LH & FSH are produced by the same anterior pituitary cell 12 Testosterone (notes) Source synthesized & released by Leydig (interstitial) cells of testis release stimulated by LH Actions inhibits release of GnRH & LH (not FSH) stimulates spermatogenesis (in conjunction with FSH) stimulates differentiation of male genitalia (in utero) stimulates development of male 2 sexual characteristics at puberty growth & development of internal/external genitalia bone growth and epiphyseal plate closure, muscle development axillary, pubic, body hair, male pattern baldness fat distribution, laryngeal growth, sebaceous glands behavioral effects, libido, aggression Mechanism: steroid, androgen binding protein, transcription, translation 13 Female reproductive system fig 17-13a 14 Female genitalia (internal) fig 17-13b 15 Female genitalia (external) fig 17-14 16 Oogenesis Note: asymmetric meiotic divisions timing of mitotic & meiotic divisions fig 17-15 17 Oogenesis (notes) Timing of divisions oogonium primary oocyte (mitosis) in utero 1 oocytes begin 1st meiotic division, stop in prophase, still in utero 1 oocyte 2 oocyte + 1st polar body, (1st meiotic) before ovulation 2 oocyte ovum + 2nd polar body (2nd meiotic) after fertilization Note: one 1 spermatocyte 4 spermatozoa; one 1 oocyte 1 ovum Follicular attrition oocyte surrounded by layer of granulosa cells primordial follicle several million follicles form in utero, 2-4 x 106 remain at birth ~400,000 remain at puberty, ~400 ovulated during reproductive life last ovulated may be 35 years older than first ovulated at puberty 18 Follicular development fig 17-16 19 Follicular life cycle through menstrual cycle (notes) In childhood & adult life many primordial follicles develop to preantral follicles day 1 – day 7 10-25 preantral follicles antral follicles (larger oocyte, more layers of granulosa cells, antrum appears, thecal cells differentiate) around day 7 one antral follicle becomes dominant, rest degenerate around day 14 mature follicle ~ 1.5 cm diameter, bulging through surface of ovary, primary oocyte divides hours before ovulation occurs day 14 – day 25 corpus luteum produces estrogens, progesterone & inhibin day 25 – day 28 corpus luteum spontanteously degenerates, menstrual flow begins 20 Follicular life cycle through menstrual cycle fig 17-17 21 Functions of granulosa & thecal cells Granulosa cells 1. nourish the developing oocyte 2. secrete antral fluid 3. site of action of estrogens & FSH 4. contains aromatase, the enzyme which converts androgen to estrogens 5. secrete inhibin (inhibits FSH release by anterior pituitary) Note the similarities between granulosa cells & Sertoli cells Theca cells 1. secrete androgens which diffuse to granulosa cells Note the similarity between theca cells & Leydig cells 22 Estrogens synthesis by granulosa & thecal cells Note: LH & FSH are shown as acting on the wrong cells in your text book LH FSH Note: “estrogens” are a mixture of estradiol (most), estriol, & estrone fig 17-19 23 Hormonal control of the menstrual cycle fig 17-18 24 Sequential hormonal changes during menstrual cycle 1. degeneration of corpus luteum estrogen, progesterone, inhibin FSH & LH 2. antral follicles develop estrogen levels 3. plasma estrogen levels increase 4. ~day 7, dominant follicle secretes high levels of estrogen 5. plasma estrogen level increases sharply 6. high estrogen levels suppress FSH levels causing degeneration of non-dominant follicles 7/8. estrogen levels LH surge (positive feedback) 9. 1st meiotic division of 1 oocyte 10. ~day 14, ovulation occurs 11. the dominant follicle collapses, and reogranizes as the corpus luteum 25 Sequential hormonal changes during menstrual cycle 12. corpus luteum secretes estrogen & progesterone 13. plasma levels of estrogen & progesterone increase, suppressing release of GnRH, LH, & FSH 14. ~day 25, corpus luteum spontaneously degenerates 15. secretion & plasma levels of estrogen & progesterone 16. estrogen & progesterone FSH & LH levels which begin follicular development of the next menstrual cycle 26 Hormonal interactions in the female fig 17-20 27 Hormonal initiation of ovulation fig 17-21 28 Endometrial changes during menstrual cycle fig 17-22 29 Endometrial changes during menstrual cycle Menstrual phase (first 3-5 days) corpus luteum degenerates, estrogen & progesterone levels fall endometrial blood vessels constrict ischemia, then relax endometrium degenerates resulting in menstrual flow Proliferative phase (day 5-14) increasing estrogen levels myometrial & endometrial growth progesterone receptors on endometrial cells cervix secretes abundant, clear, watery fluid Secretory phase (day 15-28) high progesterone levels blood vessels, coiling of glands, glycogen in cells cervix secretes thick sticky mucus (mucus plug) contraction of myometrium 30 Estrogen actions moderate increase inhibits release of GnRH & LH (negative feedback) large increase stimulates LH release (positive feedback) differentiation of female genitalia in utero is due to the absence of testosterone, not any actions of estrogens stimulates the changes seen at puberty growth of external genitalia growth of breasts (particularly fat deposition & duct growth) bone growth & epiphyseal plate closure (pubertal spurt & female configuration) fat distribution, reduces LDL & raises HDL (anti-atherogenic) during menstrual cycle Fallopian tube peristalsis & ciliary activity, growth of myometrium & endometrium, cervical mucus abundant & clear 31 Progesterone actions high levels (in presence of estrogen) inhibit release of GnRH, hence LH & FSH (negative feedback) stimulates the changes seen at puberty growth of breasts (particularly glandular tissue) during menstrual cycle Fallopian tube peristalsis & myometrial contractions endometrial blood flow, coiling of glands, glycogen content thick sticky cervical secretion (mucus plug) body temperature by ~0.5 C Note: adrenal androgens stimulate axillary & pubic hair growth, libido 32 Female sexual response Arousal phase initiated by physical (e.g. clitoral stimulation) or psychological stimuli mostly directed by parasympathetic nervous system blood flow to breasts, nipple erection blood flow to genitalia, swelling of labia, clitoral erection mucus secretion by vaginal epithelium Orgasmic phase mostly directed by sympathetic nervous system rhythmic contractions of lower 1/3 of vaginal canal associated physical responses ( heart rate, respiratory rate, intensely pleasurable sensations) Note: achieval of orgasm is not necessary for fertilization to occur 33 Fertilization 1 Viability of ovulated oocyte: ~24 hours Viability of ejaculated sperm: ~4 days Fertilization could occur from 4 days prior to, or 1 day after ovulation Sperm transport & capacitation each ejaculate contains ~3x106 spermatozoa sperm transport into Fallopian tube part by peristalsis, part by sperm flagellar action; only ~100 sperm make it sperm capacitation: several hours in female tract, flagellar function changes, membrane changes permit fusion with egg Oocyte structure ovulated as 2 oocyte, surrounded by zona pellucida (clear non-cellular layer, and corona radiata (granulosa cells ovulated with oocyte) 34 Fertilization 2 oocyte picked up by cilia on fimbriae, moves into ampulla of oviduct, and is moved by ciliary action to uterus taking ~4 days fertilization typically occurs in ampulla sperm moves between corona cells, fuses with species-specific receptors on zona pellucida enzymes of acrosome dissolve path through zona pellucida sperm head enters oocyte, tail remains outside entry of first sperm causes oocyte membrane to become impermeable to subsequent sperm entry of sperm induces 2nd meiotic division & expulsion of 2nd polar body sperm & ovum nuclei fuse zygote 35 Fertilization fig 17-23 36 Implantation zygote takes 3-4 days to reach uterus, undergoing several cell divisions en route cell mass (morula) floats in uterus for additional 3 days & develops into blastocyst note: at this time corpus luteum is functioning and the cervix secretes the mucus plug that prevents exit of blastocyst blastocyst implants in endometrium and begins to organize placenta placenta begins secretion of human chorionic gonadotropin (HCG) ~3 days after implantation HCG maintains function of corpus luteum beyond normal life (~11 days) HCG is what is detected by pregnancy tests clinical labs can detect HCG before the next menstrual period is due 37 Implantation of blastocyst fig 17-24 38