Female repro n
advertisement

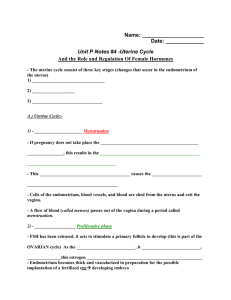
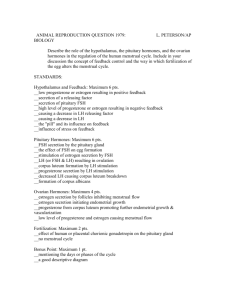
Learning objectives • Name the key hormones secreted by graffian follicles and corpora lutea of the ovaries. • Describe the physiologic changes that occur in the female reproductive organs during the ovarian and menstrual cycle. • Know the general actions of 17-estradiol and progesterone. hundred thousand • When a female child is born, each ovum is surrounded by a single layer of granulosa cells; the ovum, with this granulosa cell sheath, is called a primordial follicle, • Throughout childhood, the granulosa cells are believed to provide nourishment for the ovum and to secrete an oocyte maturation-inhibiting factor that keeps the ovum suspended in its primordial state in the prophase stage of meiotic division. • Then, after puberty, when FSH and LH from the anterior pituitary gland begin to be secreted in significant quantities, the ovaries, together with some of the follicles within them, begin to grow. FSH is decreasing because of the inhibitory effect of estrogen on FSH release. Peripher al Actions estrogen increases their proliferation and sensitivity to FSH. Peripheral effects of estrogen produced by the granulosa cells during the follicular phase include • Circulating estrogens stimulate the female sex accessory organs and sec-ondary sex characteristics. • Rising levels of estrogens cause the endometrial cells of the uterine mucosal layers to increase their rate of mitotic division (proliferate). • Circulating estrogens cause the cervical mucus to be thin and watery, making the cervix easy for sperm to traverse 5-10 developing follicle progesterone LH Proliferative Phase (Estrogen Phase) of the Endometrial Cycle, Occurring Before Ovulation • The endometrial surface is re epithelialized • Endometrium increases greatly in thickness, owing to increasing numbers of stromal cells and to progressive growth of the endometrial glands and new blood vessels into the endometrium. • The endometrial glands, especially those of the cervical region, secrete a thin, stringy mucus. 2 days prior to ovulation estrogen begins to fall about 1 day before ovulation Estrogen FSH LH removes the restraint upon meiosis, which has been arrested in prophase for years. The first meiotic division is completed, and the first polar body is extruded 2 days Corpus Luteum • The process of luteinization occurs following the exit of the oocyte from the follicle. • The corpus luteum is made up of the remaining granulose cells, thecal cells, and supportive tissue. • Once formed, the luteal cells are stimulated by LH to secrete considerable progesterone and some estrogen. Progesterone inhibits LH secretion (negative feedback). The increased plasma level of progesterone has several actions • It causes the uterine endometrium to become secretory, providing a source of nutrients for the blastocyst. • It causes the cervical mucus to become thick, sealing off the uterus from further entry of sperm or bacteria. • It has thermogenic properties, causing the basal body temperature to increase by 0.5– 1.0° F. Secretory Phase (Progestational Phase) of the Endometrial Cycle, Occurring After Ovulation • Progesterone causes marked swelling and secretory development of the endometrium. • The glands increase in tortuosity; an excess of secretory substances accumulates in the glandular epithelial cells. • Also, the cytoplasm of the stromal cells increases; lipid and glycogen deposits increase greatly in the stromal cells; • Blood supply to the endometrium further increases in proportion to the developing secretory activity. • Length of the secretory phase is constant – 14 days Involution of the Corpus Luteum and Onset of the Next Ovarian Cycle • Estrogen and progesterone, secreted by the corpus luteum during the luteal phase of the ovarian cycle, have strong feedback effects on the anterior pituitary gland to maintain low secretory rates of both FSH and LH. • The lutein cells secrete small amounts of the hormone inhibin, inhibits secretion by the anterior pituitary gland, especially FSH secretion Final involution • Occurs at the end of almost exactly 12 days of corpus luteum life. • At this time, the sudden cessation of secretion of estrogen, progesterone, and inhibin by the corpus luteum removes the feedback inhibition of the anterior pituitary gland, allowing it to begin secreting increasing amounts of FSH and LH again. Monthly endometrial cycle and mensuration (1) proliferation of the uterine endometrium; (2) development of secretory changes in the endometrium (3) desquamation of the endometrium, which is known as menstruation Proliferative Phase (Estrogen Phase) of the Endometrial Cycle, Occurring Before Ovulation • The endometrial surface is re epithelialized • Endometrium increases greatly in thickness, owing to increasing numbers of stromal cells and to progressive growth of the endometrial glands and new blood vessels into the endometrium. • The endometrial glands, especially those of the cervical region, secrete a thin, stringy mucus. Secretory Phase (Progestational Phase) of the Endometrial Cycle, Occurring After Ovulation • Progesterone causes marked swelling and secretory development of the endometrium. • The glands increase in tortuosity; an excess of secretory substances accumulates in the glandular epithelial cells. • Also, the cytoplasm of the stromal cells increases; lipid and glycogen deposits increase greatly in the stromal cells; • Blood supply to the endometrium further increases in proportion to the developing secretory activity. • Length of the secretory phase is constant – 14 days Monitoring the Menstrual Cycle The amount of sex steroids excreted in the urine can be used to monitor the menstrual cycle. For example: • Low progesterone metabolites and low but slowly rising estrogen metabo-lites characterize the early follicular phase. • Low progesterone metabolites and rapidly rising estrogen metabolites characterize the latter part of the follicular phase just before ovulation. • Elevated levels of progesterone metabolites characterize the luteal phase and pregnancy. In the early luteal phase progesterone is rising, in the latter half it is falling. pathological • Anatomic abnormalities • A hypothalamic–pituitary origini. Kallman’s syndrome, ii. Functional hypothalamic amenorrhea, iii. Amenorrhea in female athletes, iv. Eating disorders, v. Hypothyroidism, and vi. Pituitary tumors such as prolactinomas. • Ovarian causes – i. Premature ovarian failure (premature meno-pause), ii. Repetitive ovulation failure, or iii. Anovulation (intermittent bleeding), iv. Polycystic ovary. Polycystic Ovarian Syndrome • One theory suggests that it originates as an exaggerated adrenarche in obese girls. • The high extraglandular estrogens (mainly estrone) selectively suppress FSH. Ovarian follicles do have a suppressed aromatase activity and thus a diminished capacity to convert androgen into estrogen, but the adrenals may also contribute to the excess androgens as well. • High androgens promote atresia in developing follicles and disrupt feedback relationships. Polycystic Ovarian Syndrome • The overall result is anovulation-induced amenorrhea with an estrogen-induced endometrial hyperplasia and breakthrough bleeding. • Characterized by infertility, hirsutism, obesity, insulin resistance, and amenorrhea or oligomenorrhea Hirsutism • Defined as an excessive generally male pattern of hair growth. • Virilization refers to accompanying additional alterations, such as deepening of the voice, clitoromegaly, increased muscle bulk, and breast atrophy. • It is often associated with conditions of androgen excess such as con-genital adrenal hyperplasia and polycystic ovarian syndrome. • Axillary and pubic hair are sensitive to low levels of androgen. Hair on the upper chest, face (scalp region not involved), and back requires more androgen and represents the pattern seen in males. Hirsutism • Circulating androgens involved are testosterone, DHEA, DHEAS, and androstenedione in response to LH and ACTH. • Measurements of DHEAS as well as a dexamethasone suppression test helps in separating an adrenal from an ovarian source. • Polycystic ovarian syndrome is the most common cause of ovarian androgen excess Menopause • At age 40 to 50 years, the sexual cycle usually becomes irregular, and ovulation often fails to occur. • At about age 45 years, only a few primordial follicles remain to be stimulated by FSH and LH, the production of estrogens by the ovaries decreases as the number of primordial follicles approaches zero. • When estrogen production falls below a critical value, the estrogens can no longer inhibit the production of the gonadotropins FSH and LH. • FSH and LH ,are produced after menopause in large and continuous quantities. physiological changes (1) “hot flushes” (2) psychic sensations of dyspnea (3) irritability, (4) fatigue, (5) anxiety, (6) occasionally various psychotic states, (7)decreased strength and decreased calcification of bones throughout the body. Female hormones Functions of the Estrogens— Their Effects on the Primary and Secondary Female Sex Characteristics 1. Effect of Estrogens on the Uterus and External Female Sex Organs. • The ovaries, fallopian tubes, uterus, and vagina all increase several times in size. Also, the external genitalia enlarge, with deposition of fat. • change the vaginal epithelium from a cuboidal into a stratified type • marked proliferation of the endometrial stroma and greatly increased development of the endometrial glands, 2. Effect of Estrogens on the Fallopian Tubes 3. Effect of Estrogens on the Breasts. (1) development of the stromal tissues of the breasts, (2) growth of an extensive ductile system, and (3) deposition of fat in the breasts 4. Effect of Estrogens on the Skeleton inhibit osteoclastic activity in the bones unite the epiphyses with the shafts of the long bones 5. Effect of Estrogens on Protein Deposition slight positive nitrogen balance 6. Effect of Estrogens on Body Metabolism and Fat Deposition. increase the whole-body metabolic rate fat in the subcutaneous tissues deposition of fat in the buttocks and thighs 7. Effect of Estrogens on the Skin. Soft, smooth vascular 8. Effect of Estrogens on Electrolyte Balance sodium and water retention by the kidney tubules Relative levels of LH release in human females throughout life. During the first few years after menopause, follicles timulating hormone (FSH) levels are normally extremely high. A 56-year-old woman completed menopause 3 years ago. However, she is found to have low levels of FSH in her blood. Which of the following is the best explanation for this finding? A) She has been receiving hormone replacement therapy with estrogen and progesterone since she completed menopause B) Her adrenal glands continue to produce estrogen C) Her ovaries continue to secrete estrogen D) She took birth control pills for 20 years before menopause A female athlete who took testosterone-like steroids for several months stopped having normal menstrual cycles. What is the best explanation for this observation? A) Testosterone stimulates inhibin production from the corpus luteum B) Testosterone binds to receptors in the endometrium, resulting in the endometrium’s failure to develop during the normal cycle C) Testosterone binds to receptors in the anterior pituitary that stimulate the secretion of folliclestimulating hormone (FSH) and luteinizing hormone (LH) D) Testosterone inhibits the hypothalamic secretion of gonadotropin-releasing hormone and the pituitary secretion of LH and FSH Seven days after ovulation, pituitary secretion of luteinizing hormone (LH) decreases rapidly. What is the cause of this decrease in secretion? A) The anterior pituitary gland becomes unresponsive to the stimulatory effect of gonadotropin-releasing hormone (GnRH) B) Estrogen from the developing follicles exerts a feedback inhibition on the hypothalamus C) The rise in body temperature inhibits hypothalamic release of GnRH D) Secretion of estrogen and progesterone by the corpus luteum suppresses hypothalamic secretion of GnRH and pituitary secretion of LH E) None of the above A young woman is given daily injections of a substance beginning on the 16th day of her normal menstrual cycle and continuing for 3 weeks. As long as the injections continue, she does not menstruate. The injected substance could be which of the following? A) Testosterone B) FSH C) An inhibitor of progesterone’s actions D) A prostaglandin E2 inhibitor E) HCG During the 12-hr period preceding ovulation, which of the following is true? A) The plasma concentration of estrogen is rising B) A surge of luteinizing hormone is secreted from the pituitary C) The surge occurs immediately after the formation of the corpus luteum D) The surge is followed immediately by a fall in the plasma concentration of progesterone E) The number of developing follicles is increasing When do progesterone levels rise to their highest point during the female hormonal cycle? A) Between ovulation and the beginning of menstruation B) Immediately before ovulation C) When the blood concentration of luteinizing hormone is at its highest point D) When 12 primary follicles are developing to the antral stage As menstruation ends estrogen levels in the blood rise rapidly. What is the source of the estrogen? A) Corpus luteum B) Developing follicles C) Endometrium D) Stromal cells of the ovaries E) Anterior pituitary gland If a woman has a tumor secreting large amounts of estrogen from the adrenal gland, which of the following will occur? A) Progesterone levels in the blood will be very low B) Her luteinizing hormone secretion rate will be totally suppressed C) She will not have normal menstrual cycles D) Her bones will be normally calcified E) All of the above A 20-year-old woman is not having menstrual cycles. Her plasma progesterone concentration is found to be minimal. What is the explanation for the low level of progesterone? A) LH secretion rate is elevated B) LH secretion rate is suppressed C) FSH secretion rate is suppressed D) No corpus luteum is present E) High inhibin concentration in the plasma has suppressed progesterone synthesis Before the preovulatory surge in luteinizing hormone, granulosa cells of the follicle secrete which of the following? A) Testosterone B) Progesterone C) Estrogen D) Inhibin Two days before the onset of menstruation, secretions of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) reach their lowest levels. What is the cause of this low level of secretion? A) The anterior pituitary gland becomes unresponsive to the stimulatory effect of gonadotropinreleasing hormone (GnRH) B) Estrogen from the developing follicles exerts a feedback inhibition on the hypothalamus C) The rise in body temperature inhibits hypothalamic release of GnRH D) Secretion of estrogen, progesterone, and inhibin by the corpus luteum suppresses hypothalamic secretion of GnRH and pituitary secretion of FSH What is the cause of menopause? A) Reduced levels of gonadotropic hormones secreted from the anterior pituitary gland B) Reduced responsiveness of the follicles to the stimulatory effects of gonadotropic hormones C) Reduced rate of secretion of progesterone from the corpus luteum D) Reduced numbers of follicles available in the ovary for stimulation by gonadotropic hormones