Chapter 4 Psychopharmacology
Chapter 4
Psychopharmacology
Psychopharmacology
The study of the effects of dugs on the nervous system and on behavior
Q: What is a drug?
A: “An exogenous chemical not necessary for normal cellular functioning that significantly alters the functions of certain cells of the body when taken in relatively low doses”
Drug effect – the changes a drug produces in an animal’s physiological processes and behavior
Sites of action – the locations at which molecules of drug interact with molecules located on or in cells of the body, thus affecting some biochemical processes of these cells
Principles of Psychopharmacology
Pharmacokinetics – the process by which drugs are absorbed, distributed within the body, metabolized, and excreted
Routes of administration
Intravenous (IV) injection
– directly into a vein; fastest route
Intraperitoneal (IP) injection
– into the peritoneal cavity – the space that surrounds the stomach, intestines, liver, and other abdominal organs
Intramuscluar (IM) injection
– into a muscle
Subcutaneous (SC) injection – into the space beneath the skin
Oral administration – admin into the mouth, so that it is swallowed; most common with humans
Sublingual admin – placing substance beneath tongue
Intrarectal admin
– into the rectum
Inhalation
– admin of a vaporous substance into lungs
Topical admin – directly onto skin or mucous membrane
Intracerebroventricular (ICV) admin – into one of the cerebral ventricles; to allow for widespread distribution in the brain
Principles of Psychopharmacology
Distribution of drugs within the body
Several factors determine the rate at which a drug in the bloodstream reaches sites of action within the brain:
Lipid solubility: BBB blocks only water-soluble molecules; thus, lipidsoluble molecules can pass into brain and distribute themselves
Depot binding – binding of a drug with various tissues of the body or with proteins in the blood; causes drugs to not reach their site of action
e.g. Albumin – a protein found in the blood that transports free fatty acids and can bind with some lipid-soluble drugs
Can delay or prolong the effects of a drug
Inactivation and Excretion
Drugs do not remain in body indefinitely
Most deactivated by enzymes
Excreted by kidneys
Drug effectiveness
The best way to measure the effectiveness of a drug is to plot a dose-response curve
Do this by giving subjects various doses of a drug and plotting effects
Increasingly stronger doses of a drug causes increasingly larger effects, until a maximum effect is reached
Drug effectiveness
One measure of a drug’s margin of safety is its therapeutic index
The ratio b/t the dose that produces the desired effect in 50% of the animals (ED 50) and the dose that produces toxic effects in
50% of the animals (LD 50)
The lower the therapeutic dose is, the more care must be taken when prescribing the drug
Why do drugs vary in effectiveness?
Different drugs may have different sites of action
Affinity – the readiness with which 2 molecules join together; drugs in
CNS produce effects by binding to receptors, transport molecules or enzymes
The higher the affinity, the lower the concentration needed to produce effects
Effects of repeated administration
In some cases, when a drug is administered repeatedly its effects will diminish, i.e. develop tolerance
e.g. heroin, once taken regularly enough, individual will suffer withdrawal symptoms (opposite to those produced by a drug) when they stop taking it; caused by same mech as tolerance
Tolerance is the body’s attempt to compensate for the effects of a drug
In other cases, a drug will become more and more effective, sensitization
Less common than tolerance
Some drug effects show tolerance while others may show sensitization
e.g. cocaine; repeated admin may causes more movement disorders, while euphoric effects may show tolerance
Placebo effects
An innocuous substance that has no specific physiological effect
Often used for control groups in clinical drug studies
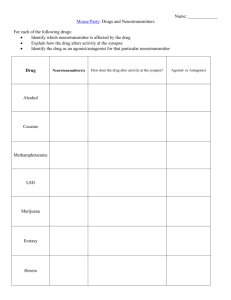
Sites of drug action
Most drugs affecting behavior do so by affecting synaptic transmission:
Antagonist – a drug that opposes or inhibits the effects of a particular NT on the postsynaptic cell
Agonist – a drug that facilitates the effects of a particular NT on the postsynaptic cell
Sites of drug action
Effects on production of NT
precursors can increase rate of NT synthesis and release; agonist
(Step 1)
NT synthesis is controlled by enzymes; some drugs can inactive these enzymes, thus preventing NT production; antagonist (Step 2 in diagram)
Effects of storage and release of NT
transporter molecules that fill synaptic vesicles with molecules of NT can be blocked by a drug; thus, preventing NT to fill vesicles; antagonist (Step 3)
Some drugs prevent release of NT from terminal button by deactivating proteins that help fuse vesicles to membrane; antagonist
(Step 5)
some drugs can trigger release of NT; agonist (Step 4)
Sites of drug action
Effects on receptors
Some drugs can bind to postsynaptic receptors like NT
Direct agonist – a drug that mimics the effects of a NT by binding with and acting on a receptor (Step 6)
Receptor blocker
– a drug that binds with a receptor but does not activate it; prevents the natural ligand from binding with the receptor (Step 7)
Some receptors have multiple binding sites; NT can bind to main sites, while other ligands can bind to alternative sites
these alternative sites can be blocked by a drug, termed noncompetitive binding
drug attached to alt site could prevent ion channels from opening; indirect antagonist
drug attaches to alt site and facilitates opening of ion channel; indirect agonist
some presynaptic membranes have autoreceptors that regulate amount of NT released; stimulation of autoreceptors causes less NT to be released
drugs that activate autoreceptors act as antagonists less NT released (Step 8)
drugs that block autoreceptors act as agonists more NT released (Step 9)
Sites of drug action
Effects on reuptake or destruction of NT
drugs can attach to transporter molecules responsible for reuptake and block it; thus NT in synapse for longer duration; agonist (Step 10)
drugs can bind with enzyme that destroys NT, preventing enzyme from working; agonist (Step 11)
Neurotransmitters and Neuromodulators
In the brain, most synaptic communication is accomplished by 2
NT:
One with excitatory effects: glutamate
One with inhibitory effects: GABA
Most of the activity of local circuits of neurons involves balances b/t the excitatory and inhibitory effects of these chemicals
Most other NT have modulating effects, i.e. they tend to activate or inhibit entire circuits of neurons that are involved in particular brain functions
Acetylcholine
Primary NT secreted by efferent axons of the CNS
All muscular movement is accomplished by the release of ACh, also found in ganglia of ANS and at target organs of the parasymp branch of the ANS
Involved mostly in 3 systems in brain:
Dorsolateral pons, basal forebrain, & medial septum
Composed of choline and acetate
Synthesis:
Acetyl-CoA and choline are combined by choline acetyltransferase (ChAT)
2 drugs affect the release of ACh:
Botulinum toxin – ACh antagonist; prevents release by terminal buttons; found in improperly canned food
Black widow spider venom – stimulates release of ACh
Deactivated by acetylcholinesterase (AChE), which is present in the presynaptic membrane, and produces choline and acetate
Two types of ACh receptors:
Nicotinic – ionotropic ACh receptor that is stimulated by nicotine and blocked by curare
Muscarinic – metabotropic ACh receptor that is stimulated by muscarine and blocked by atropine; slower action, longer lasting
Monoamines
Catecholamines:
Dopamine
Norepinephrine
Epinephrine
Indolamines
Serotonin
Dopamine (DA)
Produces both excitatory and inhibitory postsynaptic potentials, depending on postsynaptic receptor
Implicated in movement, attention, learning, and reinforcing effects of drugs
Synthesis of catecholamines:
1.
Tyrosine (obtained via diet) converted to L-
DOPA by tyrosine hydroxylase
2.
L-DOPA converted to DA by DOPA decarboxylase
3.
DA converted to
Norepinephrine (NE) by
DA
β-hydroxylase
Dopaminergic systems
Nigrostriatal system – originates in the substantia nigra and terminates in the neostriatum (caudate and putamen); control of movement
Mesolimbic system – originates in ventral tegmental area (VTA) and terminates in the nucleus accumbens, amygdala, & hippocampus; reward pathway
Mesocortical system – originates in VTA and terminates in prefrontal cortex; formation of STM, planning, strategies
Dopamine
Parkinson’s disease – a neurological disease caused by degeneration of DA neurons in nigrostriatal system; movement disorder with symptoms of tremors, rigid limbs, poor balance, difficulty initiating movements; individuals with Parkinson’s are given L-DOPA as Tx
Several types of DA subreceptors: D
1
Other drugs effecting DA and D
2 most common
AMPT
Reserpine
Apomorphine
Monoamine oxidase (MAO) – enzyme that destroys catecholamines
Norepinephrine (NE) & Epinephrine
Aka Noradrenaline & adrenaline
NE found in neurons in ANS
Epinephrine produced by adrenal glands
NE synthesis is finished in the vesicles of the terminal button
DA fills the vesicles, and is then converted to NE via DA
β-hydroxylase
Fusaric acid blocks activity of this enzyme and prevents production of NE without affecting DA
Excess NE is destroyed by MAO, type A
Cell bodies of most important NE system are in locus coeruleus
Most noradrenergic cells release NE via axonal varicosities (beadlike swellings of the axonal branches) instead of terminal button
Several types of subreceptors:
β
1
& β
2 receptors, and α
1
& α all metabotropic with GPCRs
2 receptors: sensitive to both NE and epinephrine,
In general, behavioral effects are excitatory
Serotonin (5-HT)
Complex behavioral effects: regulation of mood, control of eating, sleep, and arousal, regulation of pain
Precursor is tryptophan, which is obtained through diet; converted to 5-HTP by the enzyme tryptophan hydroxylase; which is converted to 5-HT by the enzyme 5-HTP decarboxylase
Most 5-HT neurons found in raphe nuclei of the pons, medulla and midbrain and project to cerebral cortex; also innervate basal ganglia, dentate gyrus and hippocampal formation
5-HT release from varicosities rather than terminal buttons; 2 types
D system – originates in dorsal raphe nucleus; thin axonal fibers that do not form synapses with other neurons (i.e. 5-HT serves as modulator here)
M system – originates in median raphe nucleus; thick axonal fibers, form conventional synapses
2 systems have different behavioral effects
At least 9 different subreceptors
Drugs that inhibit reuptake of 5-HT (SSRIs) most widely used clinically for mental disorders (e.g. fluoxetine, or Prozac)
LSD and MDMA affects 5-HT systems
Amino Acids
At least 8 amino acids have been suggested to serve additionally as NT
Glutamate
GABA
Glycine
Peptides
Glutamate
Principle excitatory NT in the CNS
Produced in abundance, no way to disrupt synthesis without disrupting other cellular activities
4 types of receptors:
NMDA – ionotropic, controls calcium channel that is normally blocked, and allows influx of calcium so it can serve as a 2 nd messenger; involved in forming new memories
AMPA – ionotropic, controls sodium channel, stimulated by AMPA
Kainate – ionotropic, controls sodium channel, stimulated by kainic acid
Metabotropic glutamate receptor – sensitive to glutamate
PCP – a drug that binds with the PCP binding site of the NMDA receptor and serves as an indirect antagonist; hallucinogenic drug
GABA
Primary inhibitory NT in CNS
Produced from glutamic acid by the enzyme glutamic acid decarboxylase (GAD)
2 subreceptors:
GABA
A
– have at least 5 different binding sites:
primary for GABA, of which muscimol acts a agonist and bicuculline acts as antagonist
2 nd binding site binds with drugs in benzodiazepines (e.g. Valium; anxiolytic
– anxiety-reducing)
3 rd binding site binds with barbituates
GABA
B
Glycine
Inhibitory NT in SC and lower portions of brain
Receptor is ionotropic, controls chloride channel, and thus produces inhibitory postsynaptic potentials
Strychnine – glycine antagonist
Peptides
Neurons in the CNS release a large variety of peptides from all parts of the terminal button, not just active zone, allowing molecules to travel to other cells
Best known family of peptides is the endogenous opioid family
(opioid refers to natural ligands, opiate to drugs)
e.g. enkephalin
3 types of opiate receptors:
μ (mu)
δ (delta)
κ (kappa)
Several neural systems activated: analgesic, fleeing and hiding behaviors, reinforcement
Naloxone – opiate receptor antagonist
Lipids
various substances derived from lipids can serve as NT
Cannabinoids – endogenous ligand for receptors that bind with
THC, the active ingredient in marijuana
2 types of cannabinoid receptors: CB
1 and CB
2
, both metabotropic
THC produces analgesia, sedation, stimulates appetite, reduces nausea (used with cancer treatments), aids in glaucoma; reduces concentration and memory, alters visual and auditory perceptions, etc.
Anandamide – natural ligand that binds to cannabinoid receptor
Nucleosides
compound that consists of a sugar molecule bound with a purine or pyrimidine base
Adenosine – serves as neuromodulator in brain, released when cells are short of fuel or oxygen
Agonists have general inhibitory effects on behavior
Caffeine is antagonist, thus producing excitatory effects
Soluble gases
Neurons use at least 2 simple, soluble gases, nitric oxide (NO) and carbon monoxide (CO), to communicate with each other
NO used as a messenger in many parts of the body, e.g. control muscle walls of intestines, dilates blood vessels in brain, etc.