Pharmacology (translated questions from the Dutch master) 2012 1
advertisement
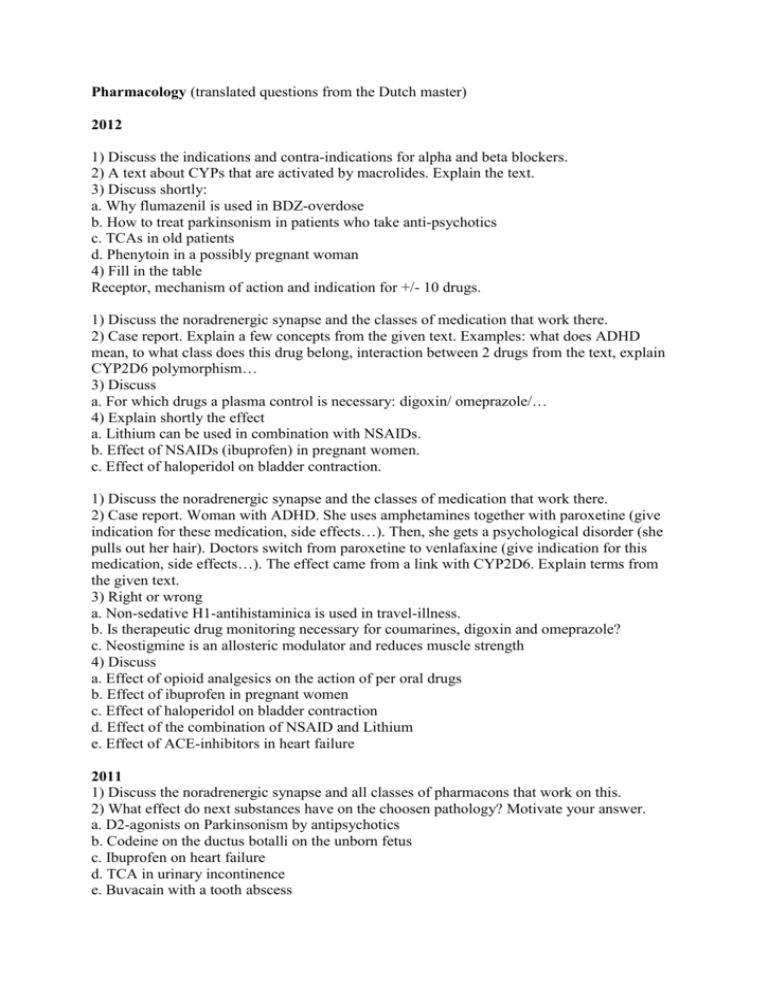
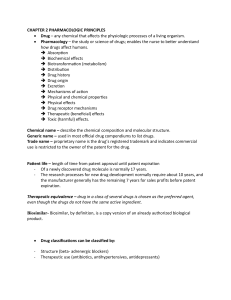
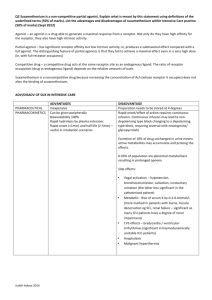
Pharmacology (translated questions from the Dutch master) 2012 1) Discuss the indications and contra-indications for alpha and beta blockers. 2) A text about CYPs that are activated by macrolides. Explain the text. 3) Discuss shortly: a. Why flumazenil is used in BDZ-overdose b. How to treat parkinsonism in patients who take anti-psychotics c. TCAs in old patients d. Phenytoin in a possibly pregnant woman 4) Fill in the table Receptor, mechanism of action and indication for +/- 10 drugs. 1) Discuss the noradrenergic synapse and the classes of medication that work there. 2) Case report. Explain a few concepts from the given text. Examples: what does ADHD mean, to what class does this drug belong, interaction between 2 drugs from the text, explain CYP2D6 polymorphism… 3) Discuss a. For which drugs a plasma control is necessary: digoxin/ omeprazole/… 4) Explain shortly the effect a. Lithium can be used in combination with NSAIDs. b. Effect of NSAIDs (ibuprofen) in pregnant women. c. Effect of haloperidol on bladder contraction. 1) Discuss the noradrenergic synapse and the classes of medication that work there. 2) Case report. Woman with ADHD. She uses amphetamines together with paroxetine (give indication for these medication, side effects…). Then, she gets a psychological disorder (she pulls out her hair). Doctors switch from paroxetine to venlafaxine (give indication for this medication, side effects…). The effect came from a link with CYP2D6. Explain terms from the given text. 3) Right or wrong a. Non-sedative H1-antihistaminica is used in travel-illness. b. Is therapeutic drug monitoring necessary for coumarines, digoxin and omeprazole? c. Neostigmine is an allosteric modulator and reduces muscle strength 4) Discuss a. Effect of opioid analgesics on the action of per oral drugs b. Effect of ibuprofen in pregnant women c. Effect of haloperidol on bladder contraction d. Effect of the combination of NSAID and Lithium e. Effect of ACE-inhibitors in heart failure 2011 1) Discuss the noradrenergic synapse and all classes of pharmacons that work on this. 2) What effect do next substances have on the choosen pathology? Motivate your answer. a. D2-agonists on Parkinsonism by antipsychotics b. Codeine on the ductus botalli on the unborn fetus c. Ibuprofen on heart failure d. TCA in urinary incontinence e. Buvacain with a tooth abscess 3) Choose the correct answer(s) and motivate. a. H1-antihistaminica X and Y. X is 10x more potent than Y, but they have the same efficiency. The patient must take 200 mg/day of Y. Side effects and pharmacokinetic profiles don’t play a role. Which one do you choose in the treatment of hay fever? b. In the use of paracetamol we must keep next risk factors in mind: gastro-duodenal ulcers, bleeding, liver failure, gout, sedation c. A child drank 2 bottles of nose decongestive. The main substance is an alpha adrenergic agonist. What effects can occur in the child? Bronchodilatation, tachycardia, mydriase, hyperthermia 4) Give the mechanism of action for these drugs, the receptor and the therapeutic effect. For the mechanism of action, choose from: competitive antagonist, antagonist, agonist, inhibitor, ion channel blocker - Cetirizine - Risperidone - Botulinetoxine - Captopril - Tubocurarine - Ethosuximide - L-DOPA - Cortisol - Celecoxib 1) What mechanisms of action of ACE-inhibitors are favorable for chronic heart failure? 2) Text about botulin toxin and myasthenia gravis. Explain all pharmacological terms. 3) Right/Wrong. Why? TCA a. Work after 3 days b. Elevate presynaptic uptake of NA. c. Must not be prescribed when glaucoma is present d. Do not sedate e. Are favorable when heart failure is present 4) Dose-Response graph. Which one is the most potent? Which one is the most efficient? Which one can be a partial agonist? What shift is suspected if addition from a competitive antagonist? 1) Discuss the medication that work on the cholinergic synapse. Discuss the clinical indications and the side effects. 2) Casus: Text about a child of 11y old that underwent surgery. 2 Drugs were administered: Odansetron and x. After administration the doctors noticed a QT-elongation. This elongation was still present postoperative (but less severe). They decided the child suffered from congenital QT-elongation, but this was undiagnosed till that age. Discuss. (Side question: What does the abbreviation HERG stand for?) 3) Dose-Response graph with 5 different data from a GABAa Receptor. a. Which one is the most potent? Relevance? b. Which one has the highest efficiency? c. What graph is the partial agonist? d. What is B is the normal graph. We add a positive modulator. What graph gives then the stimulation by GABA? (Side question: Do you know a positive modulator of the GABAa receptor?) 4) For the next drugs: give the mechanism of action, receptor class and clinical indication: laratidine, haloperidol, colecoxib, sumatriptan, fysostygmine, propranolol, theophylline, captopril, fentanyl and spironolactone. 2009 1) Discuss the drugs used against allergy. (hay fever, urticarial and angio-edema) 2) Text about secondary prevention of CVA. Discuss the pharmacological terms (CVA, secondary prevention, sartanes…) 3) Discuss a. paracetamol and codein are pharmacological stronger together than alone. b. lidocain is appropriate for usage as local anesthetic for surgery of an abscess of the teeth c. proton pomp inhibitors have an half-value life of 1.5h and are taken only once every 24h d. IMAO is chosen over SSRIs in a patient with depression (and who is treated with indirectly working sympathomimetic). e. An Addison crisis can only occur in patients that were treated with glucocorticoids during 6 months. 4) Discuss a. TCAs and anti-epileptics can be used for treatment of neuropathic pain b. In the smooth muscles of the bronchi you can find B2 and nicotinic receptors. 1) Discuss drugs against Parkinsonism (mechanism of action and side effects) 2) Text. Discuss the pharmacological terms. (nitrates, botulin toxin, muscarinic receptor…) 3) Discuss (right or wrong) a. Thiazids, lisdiuretica and digoxin can cause hypokalemia b. Do you give TCA to a depressed old person? c. Nor haloridol, nor spironolactone can cause gyneacomastia d. Sedation of an indirect GABAa agonist is a type A side effect. e. A basic local anaesthetic works better. 4) Discuss the problems in these interactions a. Phenytoine + Phenylbutazone b. aldronaat + calciumsupplements c. oral contraception + St. John’s worth d. Lithium and salt-less diet e. anti-acidics + tetracycline 1) Epilepsy: Give the possibilities to increase GABA 2) Casus: patient takes lithium: What is wrong with the patient? Patient suffers from rheumatoid arthritis. What are the drugs for RA? Is there interference with Lithium? What can you do if there is? 3) a. What happens to coagulation if you add a vitamin K antagonist to a sample of fresh blood? b. What happens if you combine IMAO and indirect sympathomimetic? c. Naloxone can be administered to a new borne baby of a heroin addicted mother 4) Right or wrong a. Is ASA advised against hay fever in children with a viral infection? b. Lisdiuretics are administered parenteral in the treatment for lung edema. c. Neuroleptics, TCA and domperidone increase the threshold for epileptic attacks. 1) anti-epileptics: What are the 4 mechanisms? Give examples of drugs and their most important pharmacokinetic properties. 2) Casus: patient with Myasthenia gravis arrives at ER with extreme muscle weakness. Why is Edrofonium better than atropine to show the difference between a Myasthenia gravis crisis (low Ach) and a cholinergic crisis (too much Ach)? 3) Right or wrong? a. Fresh blood sample: vitamin K antagonists do not influence the coagulation b. Treatment of delirium tremens: BDZ can be used because they bind the ethanol-binding site of the GABAa receptor. c. In long term use of aspirin, metoprolol, BDZ and morphine it is not advised to stop the treatment abruptly. d. Nifedipine, prazosine (alfa-1 antagonist), verapamil and nitroglycerin all cause tachycardia. e. In a heart patient, they prefer to not use TCA to treat depression. 4) Which of the 2 drugs is selected in these circumstances? a. Acute dystonia by neuroleptics: central-active anticholinergic or central-active D2-R agonist? b. esophagus ulcer and osteoporosis: strontium ranelate or alendronate? c. Baby of heroin-addicted mother: morphine or naloxone? d. pH of tissue is 6: local anesthetic with pKa= 8 or pKa = 9? e Treatment of depressed patient who is taking indirect-working sympathomimetics: IMAO or SSRI? 1) Discuss the autonomous effects of morphine. Compare to Pentazocine. 2) Casus: Article about a woman with diabetes and mania. They try to find a treatment. Discuss terms from the article. (bipolar defect, lithium, anti-epileptics, benzodiazepines,…) 3) List with names of drugs. Complete the table. (mechanism of action, receptor, use) Examples: simvastatine, ondansetron, benzodiazepines, verapamil, metoclopramide, fentanyl,... 4) Right or wrong. Discuss a. Spironolacton and neuroleptics are given in gynaecomastia. b. Furosemide is preferably administered parenteral in acute lung edema. c. paracetamol is contra-indicated in people with a history of gastric ulcers. d. Lidocaine is appropriate as local anesthetic for abscess of the teeth. e. Glucocorticoids promote wound healing by their anti-inflammatory effect. 1) Drugs used in Angor. 2) Text: Girl with a lot of symptoms (headaches, dizzy…). She received an anti-histaminic. a. Why does she have these symptoms? What does the drug do? What could be other symptoms? b. Why can you prescribe this drug? 3) Explain the effects: a. Ibuprofen ductus botalli in an unborn child b. Carbidopa nausea through L-DOPA c. Dopamine cardiogenic shock d. propranolol control of glycaemia e. Haloperidol contraction of uterus 4) Explain the interaction if there is one. a. Iburprofen and Li-salts b. Morphine and Buprenorfine c. Phenytoin and Phenylbutazone d. aldronate and Ca-supplements



![Shark Electrosense: physiology and circuit model []](http://s2.studylib.net/store/data/005306781_1-34d5e86294a52e9275a69716495e2e51-300x300.png)