MAM Decision-making Tool
advertisement

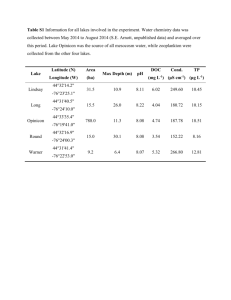
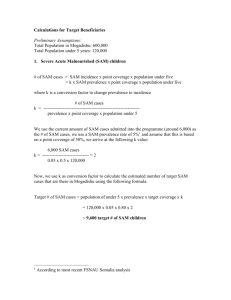
MAM Decision-making Tool Meeting Objectives Review the MAM decision-making tool Work through country situation Provide feedback on Content Usability Layout Moderate Acute Malnutrition (MAM) Background Review of supplementary feeding programs (2007) WHO consultations MMI (2008) and MMII (2010) Dietary needs Programme approaches to manage MAM NUGAG review on MAM Limited guidance on programming Differing approaches Increase in products available for programming CONFUSION!!! Moderate Acute Malnutrition (MAM) Burden of MAM 11 million children affected globally 41 million children 3 x risk of death compared to well-nourished Increased risk of acute malnutrition in emergencies MAM Taskforce Formed by the Global Nutrition Cluster UNHCR UNICEF WFP OFDA ACF Save the Children CDC Additional Members WHO ECHO Tool Objectives Guide practitioners to identify most appropriate and feasible strategies to address MAM Prevention Management (treatment) Harmonize nutrition programme decision-making on MAM in emergency situations Incorporate contextual situational factors into the decision making process Beyond nutritional status Engage in discussion Decision making process grounded by data, but is subjective on some levels Caveats of Tool Limited to emergency contexts Rapid/sudden onset Slow onset Protracted emergencies Acute emergency within a chronic emergency setting Local or large-scale emergencies Not for refugee contexts UNHCR/WFP Guidelines for Selective Feeding: The Management of Malnutrition in Emergencies 2011 http://www.unhcr.org/4b7421fd20.pdf Caveats of Tool Primary objective: prevent morbidity and mortality associated with MAM Linkages: MAM cannot be addressed in isolation SAM IYCF-E Other sectors (WASH, health, food security) Re-assessment MAM decision tool steps Step 1: Programme Type/Objective Step 2: Modality Prevention/treatment Prevention Treatment No additional programme Supplementary feeding Cash/voucher Infant and Young Child Feeding Step 3: Programme Operation Target group Product Duration Delivery Step 4: Review and Revise Regularly throughout the emergency Data Needs Prevalence of GAM in the affected area (current or historical) Information nature and severity of the crisis (risk) Baseline health data in affected areas Expected impact on morbidity Food security situation Expected impact on food security Population data Displacement Density Nutritional Data MAG scenarios for the tool High >15% Medium 8-15% Low <8% Sources Trend data Seasonality Admission data (coverage should be assessed) Screening data Risk of Deterioration Risk of Deterioration Analysis Score Increased morbidity (acute watery diarrhea, measles, acute respiratory infections) High 3 Medium 2 Low 1 Food availability and/or access disrupted (markets, prices and/or production) High 3 Medium 2 Low 1 Significant population displacement Yes 1 No 0 Populati0n density Yes 1 No 0 Sum Score Risk Category Score 6-8: High Score 4-5 :Medium Score <3: Low Morbidity Malnutrition Infection Cycle Likelihood of morbidity and/or outbreak to impact GAM Baseline data Vaccination coverage, vitamin A coverage, disease profile WASH services Access to care Risk of Deterioration Analysis Score Increased morbidity • acute watery diarrhea • measles • acute respiratory infections High 3 • Epidemic (outbreak) Medium 2 • Increasing incidence • High levels Low • Stable incidence • Low levels 1 Food Security Magnitude, extent, severity and duration of the crisis on food security Household consumption and market data sources Risk of Deterioration Analysis Score Food availability and/or access disrupted (markets, prices and/or production) High 3 • Extreme food consumption gaps • Livelihood assets being depleted • Irreversible coping strategies Medium 2 • Significant food consumption gaps • Irreversible coping strategies • Initial depletion of livelihood assets Low • Food consumption reduced • No deficient intakes • No negative coping strategies 1 Displacement Influences type and frequency of programme Many different contexts and types of displacement Dispersed settlements, mass shelter in collective centers, reception and transit camps, self settled camps, planned camps (official and unofficial), IDPs with host populations Risk of Deterioration Analysis Score Significant population displacement Yes 1 Displacement increasing and concentrated No 0 • No displacement • No increase in displacement • Sparsely populated area Population Density Risk of morbidity Consider in programme delivery design Example: low GAM, but high density= large number of children in need Haiti, post earthquake in Port au Prince Kenya, post election violence in urban centers Risk of Deterioration Analysis Score Populati0n density Yes 1 • Urban area • Dense population concentration No 0 All other areas Risk of Deterioration Risk of Deterioration Analysis Score Increased morbidity (acute watery diarrhea, measles, acute respiratory infections) High 3 Medium 2 Low 1 Food availability and/or access disrupted (markets, prices and/or production) High 3 Medium 2 Low 1 Significant population displacement Yes 1 No 0 Populati0n density Yes 1 No 0 Sum Score Risk Category Score 6-8: High Score 4-5 :Medium Score <3: Low Programme Recommendations MAM decision tool steps Step 1: Programme Type/Objective Step 2: Modality Prevention/treatment Prevention Treatment No additional programme Supplementary feeding Cash/voucher Infant and Young Child Feeding Step 3: Programme Operation Target group Product Duration Delivery Step 4: Review and Revise Regularly throughout the emergency Prevention: Modality Blanket Supplementary Feeding Provision of supplementary food Platform for other interventions Screenings + referrals Child survival (deworming, vit A, immunisation) Health/nutrition education Cash or Voucher Infant & Young Child IYCF-E support Feeding in Emergencies Component Cash/voucher if food and nutrient availability is good, markets functioning, caring practices maintained Further research needed Specialised product + cash Cash 4X value of specialised product Prevention: Target Group Children under 5 at increased risk mortality Target children 6-59 months If logistical constraints consider reducing target group PLW No standard criteria for enrollment Impact on IYCF-E MAM treatment programming exist Low birth weight Prioritise children over PLW lactating over pregnant women (protecting 0-6 month old infants) BSFP should not be expanded to beyond 6-59 months and PLW except under serious conditions The general food distribution (GFD) should meet the needs of other household members. Advocacy for improving the GFD or other food security measures. Prevention: Product Considerations Government approval Objective of the intervention & target group Some products are targeted for 6-23/36 months Household’s ability to cook Are there cooking facilities, easy access to fuel and water? Cultural practices and food preferences Corn, wheat & rice based supercereals RUFs- peanut, chickpea and milk based (limited quantities) Nutrient gap (energy & micronutrient) Decide upon higher or lower level energy HH food security, diet diversity, baseline diets, chronic malnutrition, micronutrient deficiencies Sharing practices, household use of foods, access to other foods Product Sheet Nutrition Specialised Products Product Sheet Nutrition Specialised Products Recommended Products and Alternatives Target group Primary Recommendation Interim/Alternative 6- 59 months RUSF Supercereal Plus Supercereal/oil/sugar premix PLW Supercereal/oil/sugar Older Children Supercereal/oil/sugar RUSF or Supercereal Plus 6-23 or 6-59 months Supercereal Plus LNS medium quantity RUSF± Supercereal/oil/sugar ½ sachet RUSF PLW Supercereal/oil/sugar LNS medium quantity Treatment of MAM Prevention of MAM ± Only where supplement is the primary source of available food Prevention: Duration and Exit Strategy Duration of BSFP based on scale & severity of emergency GAM + Risk of deterioration Generally 3-6 months Example start at least 1 month prior to leans season and run until post-harvest Regular re-assessment Scaling up or down Extension Rolling admission and no discharge (exiting) until end of programme (even if child is older than upper limit at the close of programme) Prevention: Delivery Mechanism Considerations Access to the population Security, seasonal, physical Scale of crisis (total area affected) Implementation capacity Low or security- consider combining with GFD Population density Determine number of sites If dense, may need multiple days/week for distribution Prevention: Delivery Mechanism BSFP stand alone programme Targeted directly to households with children BSFP Integrated delivery Child’s supplementary food is added to food/cash/voucher distribution Low security context Rapid onset immediate programming Exclusion and inclusion errors Shift to parallel independent programme as soon as feasible Treatment Targeted Supplementary Feeding (TSFP) Treatment for MAM with nutritious food supplement and routine medical care Admission/discharge criteria based on anthropometric measures (national or international guidelines) Nutrition communication Support for IYCF-E Cash/vouchers need more evidence Treatment: Target Group Malnourished children 6-59 months Discharges from SAM Pregnant and lactating (up to 6 months postpartum) women Chronic illness (HIV, TB) Exceptions Infants <6 months not admitted, support IYCF strengthened Other vulnerable populations identified (disabled children , 5-10 years olds, older people) Treatment: Product Considerations Government approval Target group Household’s ability to cook Are there cooking facilities, easy access to fuel and water? Cultural practices and food preferences Corn, wheat & rice based supercereals RUFs- peanut, chickpea and milk based (limited quantities) Product Sheet Nutrition Specialised Products Recommended Products and Alternatives Target group Primary Recommendation Interim/Alternative 6- 59 months RUSF Supercereal Plus Supercereal/oil/sugar premix PLW Supercereal/oil/sugar Older Children Supercereal/oil/sugar RUSF or Supercereal Plus 6-23 or 6-59 months Supercereal Plus LNS medium quantity RUSF± Supercereal/oil/sugar ½ sachet RUSF PLW Supercereal/oil/sugar LNS medium quantity Treatment of MAM Prevention of MAM ± Only where supplement is the primary source of available food Treatment: Duration and Exit Strategy Treatment range 1-4 months Scale down of TSFP considered when: GAM <5% No aggravating factors Low numbers of admissions in MAM and SAM treatment may also be used to decide to phase out Be mindful of programme coverage and performance Treatment: Delivery Mechanism Considerations Access to the population Security, seasonal, physical Scale of crisis (total area affected) Implementation capacity Low or security- consider combining with GFD Population density Determine number of sites If dense, may need multiple days/week for distribution Treatment: Delivery Mechanism Linked closely to treatment of SAM under CMAM model TSFP sites adjacent to OTP or health centres support referrals (both directions) Large area for distribution/services If mobile or away from health centres provide basic health interventions Considerations Health service coverage, existing MAM/SAM programmes, capacity to scale-up Prevention &Treatment Both prevention and treatment may be recommended Follow the previous steps to design each programme Think through linkages between programmes Ideally, children should not be simultaneously enrolled in both programmes In reality, the risks associated with non-participation outweigh the cost of dual participation In some large emergencies children should be enrolled in prevention programmes as they may come in and out of treatment Example: Northern Kenya, 2011/12 No Additional Intervention Additional programs not needed Existing nutritional programs Re-evaluate risk as emergency progresses Build into nutrition response plan Strengthen support for IYCF or micronutrient programmes Emergency programming is in addition to existing nutrition programmes MAM decision tool steps Step 1: Programme Type/Objective Step 2: Modality Prevention/treatment Prevention Treatment No additional programme Supplementary feeding Cash/voucher Infant and Young Child Feeding Step 3: Programme Operation Target group Product Duration Delivery Step 4: Review and Revise Regularly throughout the emergency Programme Linkages Interventions in emergencies: Addressing acute malnutrition Selective feeding programmes General Food Distribution IYCF-E Addressing underlying causes of undernutrition WASH Health Food security Addressing micronutrient deficiencies MAM Programmes Prevention Blanket feeding Cash/voucher Treatment Targeted Treatment for SAM Outpatient treatment Inpatient treatment Additional Feedback Josephine Ippe: Global Nutrition Cluster jippe@unicef.org Lynnda Kiess: World Food Programme lynnda.kiess@wfp.org My contact: Leisel Talley, Centers for Disease Control and Prevention: Ltalley@cdc.gov