Online MANDATORY Orientation Training
advertisement

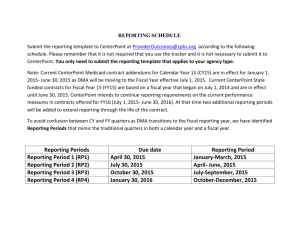
Mandatory Orientation Training for New Network Providers Welcome to CenterPoint Human Services’ Provider Network CenterPoint Human Services is a managed care organization (MCO) managing the delivery of Medicaid and State-funded mental health, intellectual/developmental disabilities and substance abuse services through a network of providers. CenterPoint works closely with providers, clients, family members and community partners to meet the needs of people in Forsyth, Stokes, Davie and Rockingham Counties. We are People in Partnership Making a Difference! Orientation It is required that all Solo practitioners and at least one representative from an agency or group participates in this mandatory orientation training for new network providers. They are then expected to share information with remaining employees. Additional information can be found in the Provider Manual posted on the CenterPoint website: www.cphs.org This training session highlights many LME/MCO topics and references resources where providers can find additional information. CenterPoint contacts are also listed to address any questions providers may have. You can log into the course as many times as you wish. Please allow a minimum of 45 minutes to complete this course. Once you have finished reviewing all course material you must also complete the attestation form and evaluation to get credit for your participation. Please be sure to “submit” when you complete the form. What will be covered in this course? Customer Services Care Coordination Utilization Management Appeals Process Quality Management Corporate Compliance Contracts, Claims and Billing Administrative and Professional Competence Network Operations Monitoring Process Disputes IRIS Customer Services Customer Services Also known as STR or ACCESS 3 Main Functions: 1. Maintain 24/7/365 ACCESS Line (Call Center) dedicated for clients - 1-888-581-9988 2. Maintain 24/7/365 Provider Line dedicated for Providers - 1-888-220-5280 3. Client Follow Up – If client “no shows” for appointment, we follow up with them. ACCESS Call Center Overview Receives 150-200 calls a day 13 staff during day / 2 in evening / 1 overnight Average call time is 8 – 10 minutes Goals are to: Answer calls in 30 seconds / Average is 22 seconds Have less than 5% Abandonment (Hang ups) / Average is 1% – 2% When all of our call center agents are on a call and unavailable to take a new call, then calls “overflow” to a backup call center vendor called ProtoCall, Inc. We triage calls into 4 different categories: Emergent, Urgent, Routine, Non-threshold ACCESS Line: Emergent Calls Call received regarding client being dangerous to self or others: If mobile crisis is not appropriate then we will dispatch police or EMS to given address. If mobile crisis is requested or seems appropriate then we will dispatch mobile crisis. If person is able to safely get to an emergency provider then we will refer to crisis services provider. We will follow-up until we know client has been seen by someone face-to-face. Access Line: Urgent The Access Standard for Urgent Services is to arrange for services within 48 hours of contact with the Customer Services access line. Any caller who presents with moderate risk in physical, cognitive, or behavioral functioning. North Carolina treats any Substance Abuse Client as an “Urgent” and offers an appointment within 48 hours. Access Line: Routine The Access Standard for Routine Services is to arrange for services within 14 days of contact with the Customer Services access line. We refer for assessment – NOT for enhanced benefits. If caller does not have a provider of choice, we offer provider choice based on requested services, funding source, and location. Provider Line: 1-888-220-5280 Need basic Information or not sure who to call? Call us, we will be glad to help. Provider needing Emergent/Urgent Authorizations (Mobile Crisis, Inpatient, Detox, authorization to assess in ED, etc…) can call Provider Line Hospital D/C appointments Emergency Respite If call goes to Voicemail, we will call you back within 30 minutes ProtoCall: If all of our agents are busy, then call will go to company called ProtoCall. They will triage call and take care of Emergent Call (get police out, dispatch mobile crisis, get person to emergency provider etc…). All other calls, they will take information and forward report to CenterPoint staff. Within 30 minutes CenterPoint staff will make contact. Follow-Up: For each triage disposition (Emergent 2 hrs., Urgent 48 hrs., and Routine 14 days) Customer Services will be responsible for seeing if client made scheduled appointment or not. For Emergent, Customer Service staff will contact provider to see if client made appt. For Urgent and Routine appointments, Providers will enter compliance data into Alpha System. We will run a “No-Show” report daily and attempt to make contact with clients to reschedule an appointment. Important for Providers: If Provider decides to have a shared calendar with CenterPoint, please update it as frequently as you can. Please keep CenterPoint informed of changes to your agency. For example, if capacity changes, if programs change, if funding sources change, let CenterPoint know. Compliance data entry must occur daily by 10:00 AM for previous day appointments. Customer Services Questions? CenterPoint Human Services Contact: Mike Bridges, LCSW mbridges@cphs.org (336) 714-9104 Care Coordination What is Care Coordination? Care Coordination is a person centered, assessment-based approach to integrating mental health and substance abuse services, primary health care and natural/community supports. CenterPoint’s care coordination department provides care coordination services to enrollees who are considered high cost/high risk (hc/hr) and/or Special Health Care Needs Populations as defined in the 1915 (b)/(c) waivers. What is MH/SA Care Coordination? Care Coordination in an LME/MCO provides a wide range of duties/roles to increase the integration of Behavioral Health and Physical Health. It is typically provided on a short term basis (average 3 to 6 months). Some of the supports provided to clients: Education about all available MH/SA/DD services and supports, as well as education about all types of Medicaid and state funded services Linkage to needed psychological, behavioral, educational and physical evaluations Facilitate access to care for clients who do not have an established clinical home. Monitors hospital admissions and discharges Who is Eligible? Individuals with special health care needs and those who are high cost/high risk will be eligible for care coordination. High Cost/High Risk Overview: High Cost: Clients whose treatment expenses place them in the top 20% of all client expenditures for the catchment area; High Risk: Clients who have been assessed to need emergent services three or more times within the previous 12 months. MH/SA Care Coordination Additional indicators for enrollees to be considered MH/SA High Cost/High Risk may include the following factors: A pattern of failed appointments Two or more jail bookings in a ninety day period Entry into the crisis system via a crisis service Out-of-catchment area residential services Obstacles in finding appropriate placement, treatment and/or funding due to circumstantial variables A history of behaviors placing the enrollee at risk to self or others Co-occurring MH and/or SA along with significant medical problems, i.e., CCNC Quadrant IV enrollee Identified by UM as a “case of concern” Special Health Care Needs Definition – MH/SA (This section will be update with DSM 5 language upon receipt of changes from the state.) Child Mental Health: Children who have a diagnosis within the diagnostic ranges defined below: 293-297.99, 298.8-298.9, 300-300.9, 302-302.6, 302.8-302.9, 307-307.99, 308.3, 309.81, 311-312.99, 313.81,313.89,995.5-995.59, V61.21 AND Current CALOCUS Level of VI, OR Who are currently or have been in the past 30 days, in a facility (including a Youth Developmental Center and Youth Detention Center) operated by the DJJDP or DOC for whom the LME has received notification of discharged. Special Health Care Needs Definition - Cont’d (This section will be update with DSM 5 language upon receipt of changes from the state.) Adult Mental Health: Adults who have a diagnosis within the diagnostic ranges of: 295-295.99, 296-296.99, 298.9, 309.81 AND Current LOCUS Level of VI. Special Health Care Needs Definition - Cont’d (This section will be update with DSM 5 language upon receipt of changes from the state.) Substance Dependent: Individuals with a substance dependence diagnosis AND Current ASAM PPC Level of III.7 or II.2-D or higher. Opioid Dependent: Individuals with an opioid dependence diagnosis AND who have reported to have used drugs by injection within the past 30 days Special Health Care Need Definition - Cont’d (This section will be update with DSM 5 language upon receipt of changes from the state.) Co-Occurring Diagnoses: Individuals with both a mental illness diagnosis and a substance abuse diagnosis AND Current LOCUS or CALOCUS of V or higher OR current ASAM PPC Level of III.5 or higher Individuals with both a mental illness diagnosis and an intellectual or developmental disability diagnosis AND Current LOCUS/CALOCUS of IV or higher Individuals with both an intellectual or developmental disability diagnosis and a substance abuse diagnosis AND Current ASAM PPC Level of III.3 or higher Department of Justice Settlement Individuals involved in the United States Department of Justice and North Carolina Settlement Agreement/Transitions to Community Living Initiative. HC/HR Intellectual and Developmental Disability (I/DD) I/DD High Cost/High Risk Overview: High Cost: I/DD enrollees whose treatment plan expenses fall within the top 20% of expenditures for all enrollees in the MCO’s catchment area. High Risk: I/DD enrollees who have been assessed to need emergent crisis services 3 or more times in the previous twelve months. HC/HR Intellectual and Developmental Disability (I/DD) Additional indicators for enrollees to be considered I/DD High Cost/High Risk may include the following factors: Co-occurring I/DD and significant medical problems Obstacles in finding appropriate placement, treatment and/or funding due to circumstantial variables A history of behavior placing the enrollee at risk of exploitation Entry into the crisis system via a crisis service NC START admission Therapeutic Respite Addressing Crisis for Kids (TRACK) referral and/or admission Special Health Care Needs Definition- I/DD Intellectual and/or Developmental Disabilities: Individuals who are functionally eligible for, but not enrolled in, the Innovations waiver, who are not living in an ICF-MR facility; OR Individuals with an intellectual or developmental disability diagnosis who are currently, or have been within the past 30 days, in a facility operated by the Department of Correction (DOC) or the Department of Juvenile Justice and Delinquency Prevention (DJJDP) for whom the LME has received notification of discharge. Collaboration with Health Home The Four Quadrant Model Work with CCNC to develop integrated care practices Coordination of care with enrollee’s PCP/CCNC physician /Health Home Monthly meetings with regional CCNC network- Northwest Community Care Network (Forsyth, Davie, Stokes) and Partnership for Health Management (Rockingham) Four Quadrant Care Management Model Quad I: Low MH/SA/DD Health Quad II: High MH/SA/DD Health Low Physical Health Complexity /Risk Low Physical Health Complexity/Risk Quad III: Low MH/SA/DD Health Quad IV: High MH/SA/DD Health High Physical Health Complexity/Risk High Physical Health Complexity /Risk Linkage to Care Coordination To link an individual to care coordination, please contact CenterPoint’s Customer Service line: 888-581-9988 Questions: I/DD Care Coordination: Jeff Payne, I/DD Clinical Director 336-714-9171 or jpayne@cphs.org MH/SA Care Coordination: Katy Horne, Care Coordination Director 336-714-9173 or khorne@cphs.org Utilization Management LOCUS/CALOCUS Authorizations EPSDT Appeals LOCUS/CALOCUS Information Sources: © American Association of Community Psychiatrists © American Academy of Child & Adolescent Psychiatry LOCUS/CALOCUS LOCUS: Level of Care Utilization System Psychiatric and Addiction Services CALOCUS: Child and Adolescent Level of Care Utilization System Psychiatric and Addiction Services (Has not been “normed” for ages 0-5) • Developmental status determines the cut-off between LOCUS and CALOCUS LOCUS/CALOCUS With the arrival of managed care programs and principles, the use of quantifiable measures to guide assessment, level of care placement decisions , continued stay criteria, and clinical outcomes is increasingly important. It provides a common language and set of standards with which to make judgments and recommendations. It incorporates developmental, family, and community systems of care perspectives. LOCUS/CALOCUS Main Objectives LOCUS/CALOCUS assesses the enrollee’s needs based on level of functioning, rather than diagnosis and psychiatric risk alone. LOCUS/CALOCUS assesses the enrollee’s needs and allocate resources based on six evaluation dimensions. LOCUS/CALOCUS determines a recommendation for level of care. It is not a substitute for clinical judgment. The Six Dimensions 1) Risk of harm to self or others, including potential for victimization or accidental harm 2) Functional status-ability to function in all age-appropriate roles, as well as basis daily living activities 3) Co-morbidity of other conditions that has the potential to exacerbate the primary presenting problem 4) Recovery environment in terms of strengths/weaknesses of the family, neighborhood and community (including services). Two subscales: a) Environmental Stress b) Environmental Support 5) Treatment history in terms of a history of successful use of treatment a) LOCUS identifies the adult’s extent of recovery in response to prior treatment b) CALOCUS identifies the child's innate or constitutional emotional strength and capacity for successful adaptation [resiliency] as well as treatment history 6) Engagement a) LOCUS identifies the patient’s degree of engagement. b) CALOCUS identifies the child and family's acceptance and engagement in treatment. i) Scale A -- Child/Adolescent ii) Scale B -- Parents/Primary Caretaker A five-point scale is constructed for each dimension Levels of Care LOCUS/CALOCUS assesses service needs and matches them to the clinically appropriate level of care, where level of care refers to intensity of services, not to bricks-and-mortar programs. This permits a broad range of treatment options that: are adaptable to the available continuum in each service area; allows for variations in practice patterns and resources among communities and agencies; Recognizes traditional services, as well as newer forms of care. Levels of Care 1. Recovery Maintenance and Health Management 2. Low Intensity Community Based Services 3. High Intensity Community Based Services 4. Medically Monitored Non-Residential Services 5. Medically Monitored Residential Services 6. Medically Managed Residential Services LOCUS/CALOCUS Links LOCUS http://communitypsychiatry.org/publications/clinical_and_administrative_t ools_guidelines/locus.aspx CALOCUS http://communitypsychiatry.org/publications/clinical_and_administrative_t ools_guidelines/CALOCUS_Instrument_2010.pdf Authorizations Authorizations Clinical information is reviewed and compared against the pertinent Service Definition If the information presented does not appear to meet the criteria for the service being requested, and the UM staff are not able to approve the request, the case is forwarded to the Medical Director, or qualified designee for peer clinical review All non-certification decisions are made by the Medical Director or their designee For Medicaid Enrollees, extensions for certification decisions are processed according to DMA requirements and URAC standards for Medicaid Enrollees Non-Medicaid (IPRS) funded requests , extensions of certification decisions are not allowed by the North Carolina Division of Mental Health/Developmental Disability/Substance Abuse Services Certification decisions are viewable in the Provider Portal with the ability to print out certification letters Pass Through Services In certain circumstances as defined by the LME/MCO or Clinical Coverage Policies, prior authorization is not required. These requests are processed one of two ways. Pass through without Notification: Substance Abuse Intensive Outpatient Program, Substance Abuse Comprehensive Outpatient Treatment Program and Mobile Crisis can be provided up to a set limit without any prior contact with the LME/MCO. Limits are defined within the related Clinical Coverage Policy. Once the limit is reached, a complete Service Authorization Request with supporting documentation must be submitted. Pass through with Notification: Providers must submit a Service Authorization Request (SAR) for notification for Inpatient Behavioral Health Services (Initial 72 hours), Supported Employment /Long Term Vocational Supports (SE/LTVS) and Peer Support Services. Limits for SE/LTVS and Peer Support Services are defined within the related Clinical Coverage Policy. Once the limit is reached, a complete Service Authorization Request with supporting documentation must be submitted. They are submitted to alert the LME/MCO of the initiation of the service and to assure payment via AlphaMCS. These SARs do not require clinical review and are processed within the non-urgent timeframe described below. Authorizations Urgent Requests: those related to inpatient behavioral health services when the provider does not utilize the pass through request, partial hospitalization, detoxification and emergency respite Processed via a telephone call. These requests are processed 24 hours a day, 7 days a week. In most cases a determination is made by the end of the phone call, but a determination is always made and verbal notification provided no later than 24 hours from the request. Authorizations Non-urgent requests: Non-urgent requests are submitted via a web-based portal A complete request includes the following: Comprehensive clinical assessment Service Authorization Request completed in the Provider Portal Person Centered Plan or a service plan with a service order If the client has a Mental Health diagnosis, a LOCUS or CALOCUS If the client has a Substance Use diagnosis, an ASAM Level If the client has a Developmentally Disabled, a SNAP score or SIS™ Reviews of ICF/MR services will include an annual review of the Level of Care If these components are not present, the provider is notified the request was not complete and additional information is requested via the Provider Portal Authorizations Non-urgent requests continued: A Utilization Management Clinician/Specialist will conduct a review. If after review, it is determined that the services requested meet medical necessity criteria, an authorization is entered into the MCO/LME’s MIS system, and the provider is able to view this via the web based portal. The determination is issued within 14 calendar days of the request. For requests involving Medicaid Enrollees, this time period will be extended one time for an additional 14 days if the enrollee requests the extension or the provider requests one on behalf of the enrollee. In cases where the initial clinical reviewer cannot make a clinical determination to certify, the case is referred to the Medical Director (or another designated M.D./PhD) for the purpose of peer clinical review. Continued Authorization/Concurrent Reviews It is the provider or facility's responsibility to submit a request for concurrent authorization to CenterPoint’s UM Department prior to the expiration of the current authorization. Authorizations Post-service/Retrospective Reviews In most cases pre-authorization is required. Since the Customer Services Department is available 24 hours daily, 7 days weekly there should be few situations where a provider is unable to obtain authorization prior to the provision of services. Authorization of care after the client/enrollee has been admitted to the level of care or after the treatment has been completed (retroactive authorization) may be considered under certain specific circumstances as described below: The enrollee is found to be eligible for Medicaid with a retroactive effective date; The request for authorization of emergency inpatient hospitalization is made within 72 hours of the client's admission; The service authorization entry is delayed pending the verification of eligibility or execution of completed provider contract; An error on the part of a UM staff person is indicated in the call or case record; Additional funding becomes available after a service has been provided Authorizations When the request for retroactive authorization does not fall into Categories above, and the UM Manager/Director, Chief Clinical Officer or Chief Operations Officer does not find a valid reason for the retrospective request, the determination is made via one of two processes: Requests for all retrospective dates of service: Returned as unable to process Requests with overlapping request for retrospective and future dates of service: Retrospective dates will be considered as unable to process. A clinical review will be completed with a start date no earlier than the date of submission Appeal rights are not applicable when a request is unable to be processed. The provider will be advised that they may follow the formal grievance processes. Authorizations It is the Provider’s responsibility to submit a request for Postservice/Retrospective review to CenterPoint's UM Department. A utilization management determination is made no later than 30 calendar days If the utilization reviewer determines that the request meets established benefits and medical necessity criteria, an authorization is issued and is viewable via the Provider Portal In cases where the utilization reviewer cannot make a determination to authorize, the case is referred to the Medical Director (or designee) Authorizations Tips for submitting requests from the UM staff: Ask for the correct units and timeframes for the services requested with close attention to begin and end dates. Consider writing requests using the language from the Service Definitions Check that the PCP has been signed and dated by all parties Submit current clinical information on concurrent reviews PCP’s will be reviewed with each request evaluating it to see if it matches current clinical needs Early and Periodic Screening, Diagnostic and Treatment (EPSDT) Medicaid for Children EPSDT U.S. Department of Health and Human Services Definition. The Early Periodic Screening, Diagnosis, and Treatment (EPSDT) Program is the child health component of Medicaid. It’s required in every state and is designed to improve the health of low-income children, by financing appropriate and necessary pediatric services Early- Identifying problems early, starting at birth Periodic – Checking children’s health at periodic, age-appropriate intervals Screening – Doing physical, mental, developmental, dental, hearing, vision, and other screening tests to detect potential problems Diagnosis – Performing diagnostic tests to follow up when a risk is identified Treatment – Treating the problems found EPSDT Defined by Federal Law Available for all individuals under age 21 who are enrolled in Medicaid Allows for Medically necessary health care that will “correct or ameliorate a defect, physical or mental illness or a condition (health problem) identified through a screening to be approved even if not covered by or exceeds the benefit plan EPSDT Criteria Must be within the scope of those listed in the Federal Law at 42 U.S.C. § 1396d(a) [1905 (a) of the Social Security Act Must be medically necessary to correct or ameliorate a defect, physical or mental illness or a condition (health problem) identified through a screening Cannot be experimental/investigational, unsafe or considered ineffective EPSDT Requests for non-covered services If a child's physician or another licensed clinician determines that a child needs a treatment service that is not normally covered by Medicaid, the provider must submit a Non-Covered State Medicaid Plan Services Request Form for Recipients under 21 Years of Age on behalf of the recipient to: CenterPoint Human Services: EPSDT Request Attn: UM Director 4045 University Parkway Winston-Salem, NC 27106 EPSDT Important Points to remember Requests for ESPDT do NOT have to be labeled as such. Any complete request for services is reviewed with ESPDT criteria applied to the review If the service requires prior approval, the fact that the recipient is under 21 does NOT eliminate the requirement for prior approval Requests for prior approval for services must be fully documented to show medical necessity, including current information from enrollee’s physician, other licensed clinicians, requesting qualified provider and or family members Requests for Medical and Dental services must be forwarded to the appropriate vendor (Medical or Dental) EPSDT See below link for more information on EPSDT http://www.ncdhhs.gov/dma/epsdt/ Appeals Process What is an Appeal? If CenterPoint determines it is appropriate to change a service or deny a request for a service, the client will receive a letter explaining the decision and their appeal rights. The letter will also include an Appeal request form. If the enrollee disagrees with the decision, they have the right to appeal any changes to the services. How that is done depends on how their services are funded. Who can request an Appeal? Standard Appeals: Must be requested by client/guardian. If an client/guardian wishes for a provider to represent then during the appeal process there must be signed written consent from the client/guardian. Expedited Appeals: Can be requested by a provider or an client/ guardian verbally or in writing The Process –Medicaid Appeals There are 3 levels of the Medicaid Appeals Process: Level 1: Reconsideration Review Completed within CenterPoint Level 2: Mediation Mediation Network of NC Level 3: OAH Hearing State Fair Hearing Process Level 1: Reconsideration Facts Local impartial review of CenterPoint’s decision to take an action. The reconsideration decision is determined by a health care professional who has appropriate clinical expertise in treating the client’s condition or disorder. The reviewer was not involved in CenterPoint’s initial decision Reconsideration must be completed before the client/guardian can request a hearing or mediation with the NC OAH. Level 1: Reconsideration Process CenterPoint receives client/guardian’s request Appeal Coordinator contracts client/guardian to acknowledge receipt of request Client/guardian or provider has 10 days to submit additional or new information Reconsideration Review is scheduled with a reviewer. Decision will be made within 30 days of request What’s Next? If initial decision is overturned: UM is notified and authorization is created Client/guardian notification via US mail Provider notified via Alpha If initial decision is upheld: Client/guardian are notified via US mail Provider notified via Alpha If client/guardian disagrees they can request a State Fair Hearing within 30 days of when the Reconsideration notices was sent. Level 2: Mediation Facts Mediation is voluntary and client/guardian may accept or decline Mediation. May be resolved quicker than a State Fair Hearing Case referred to the Mediation Network of NC. The mediator is a neutral party who guides the mediation process, facilitates communication, and assist the parties to generate and evaluate possible outcomes. The recipient does not have to accept any offer made during mediation. Offers that are accepted during Mediation are legally binding. Level 2: Mediation Process After requesting a State Fair Hearing, the client/guardian is offered an opportunity to accept Mediation. The Mediation Network of NC will contact client/guardian and CenterPoint to schedule Mediation. Mediation usually occurs via conference call with all involved parties Mediation must be completed with 10 days of receipt of request What’s Next? If Mediation is successful with all parties agreeing on the outcome: Appeal process ends here. The decision is legally binding UM is notified if an authorization is needed If Mediation is declined or unsuccessful: Appeal continues to a hearing at OAH Level 3: OAH Hearing Facts The hearing will be held by an ALJ. The client/guardian (recipient) may represent himself/herself or may hire an attorney or use a legal aid attorney, or ask a relative, friend, or other spokesperson (including provider or case manager) to speak for them. Continuances will NOT be granted on the day of the hearing except for good cause If OAH provides proper notice and the recipient fails to make an appearance, the hearing will be IMMEDIATELY DISMISSED unless the recipient presents good cause explaining why they failed to appear for the hearing within three business days of the date of the dismissal Level 3: OAH Hearing Facts (cont.) The hearing will be held by telephone unless the recipient specifically requests an in-person or videoconference hearing. The recipient may present new evidence at the hearing. This includes medical records and written reports (even if obtained after Medicaid made its decision), testimony from physicians and other providers about why the recipient needs the service, and testimony by family and friends. If new evidence is submitted at the hearing that CenterPoint has not reviewed, CenterPoint may request additional time for review. Level 3: OAH Hearing Process The recipient or legal representative will be notified in advance of the day and time of the hearing. After the Hearing the Administrative Law Judge (ALJ) will make a decision regarding the case. The ALJ will notify all parties in writing of the decision. What’s Next? If the ALJ’s final decision is not decided in favor of the client/guardian the client/guardian can appeal the case to the Superior Court. Expedited Appeals May be requested by client/guardian or provider on behalf of the client May be requested verbally or in writing Expedited Appeals are for urgent cases typically defined as: Cases related to psychiatric hospitalization, partial hospitalization or detoxification where the life or health of the client would be jeopardized by a delay Expedited Appeal Timeline CenterPoint will provide a decision for written request within three (3) calendar days and 72 hours for verbal requests. If the decision is to UPHOLD CenterPoint’s original decision: The client/guardian can proceed with the State Fair Hearing Process The State Fair Hearing Process will follow timeline for standard appeals Expedited Appeals –Non Urgent Cases If an expedited appeal is requested for a non-urgent case, UM will review to determine if an expedited appeal is indicated. If denied: The appeal will be transferred to Appeals Coordinator and will follow standard Appeal timelines If Approved: The appeal will follow timeline for Expedited appeals Non-Medicaid Appeals: Facts A client/guardian has a right to appeal an Adverse Action Client/guardian has 15 days to request an appeal CenterPoint is not required to provide MOS for NonMedicaid Appeals The Process: Non-Medicaid Appeals Level 1: Local Appeal – Completed within CenterPoint Level 2: State Appeal – Completed by NC Division of MH/DD/SAS Level 1: Local Appeal CenterPoint receives client/guardian’s request Appeals Coordinator contracts client/guardian to acknowledge receipt of request Client/guardian or provider can submit additional or new information Local Appeal is scheduled with a reviewer. Decision will be made within 7 days of request What’s Next? If initial decision is overturned: UM is notified and authorization is created Client/guardian notified via US mail Provider notified via Alpha If initial decision is upheld: Client/guardian is notified via US mail Provider notified via Alpha If client/guardian disagrees they can appeal the decision to the Division of MH/DD/SAS Level 2: DMH/DD/SAS Appeal DMH/DD/SAS must receive the request within 11 days from the date on the Local Appeal decision letter. Hearing is scheduled including all parties The Hearing findings are sent to CenterPoint within 60 days of request for DMH/DD/SAS appeal. CenterPoint will issue a final decision to the client/guardian within 10 days of receipt of findings If private insurance pays for your services: Appeal goes through the insurance company. Each company has their own process. For more information you can: Call the customer service number on the card Check their website for more information Review any written letters that were received Need assistance with Appeals? Contact the Appeals Coordinator 336-778-3633 or 1-888-581-9988 Quality Management Quality Improvement Outcomes Grievances Quality Improvement CenterPoint is required to participate in strategic projects to improve care to clients. Such projects can be called Quality Improvement Projects- QIP’s Performance Improvement Projects- PIP’s or Quality Improvement Activities- QIA’s PLAN: assess data and decide the change DO: implement the change STUDY: collect outcome data to assess the impact ACT: decide to continue or alter the plan What does this mean for Providers? If a current project involves your agency or service line: Your expertise may be needed to plan You may be asked to test a change implementation You may be asked to submit data Comparison data Outcome data Reports Performance Indicators Why measure outcomes? To ensure quality of care for enrollees To assess current state To identify what is working well To identify what needs improvement To learn from others who are providing similar services “Work smarter – not harder” What does this mean for Providers? CenterPoint may ask you to provide “outcome data” on a periodic basis You decide how to collect the data Electronically Manually Suggestion: Make it part of the flow of work Submit it electronically to CenterPoint by a specific deadline You could receive feedback of how your data compares to others offering similar services Use this result to: Offer feedback to staff…..celebrate successes! Assess what changes to make in your day to day practice Together we can make a difference! Develop Best Practices Educate and Train Staff Assist Families and Enrollees Create cost effective solutions Improve work flow for providers Fill in “gaps” of service for enrollees Improve the lives of the people we serve! What is a grievance? Per the Division of Medical Assistance (DMA) Contract: A GREIVANCE is an expression of dissatisfaction about matters involving CenterPoint. CenterPoint’s grievance system must meet all regulatory requirements in 42 CFR 438 Subpart F Possible Subjects of Grievances: Quality of Services provided through CenterPoint. Aspects of interpersonal relationships such as rudeness of a Network Provider or CenterPoint employee. Failure of CenterPoint or Network Provider to respect enrollee rights. CenterPoint Policy on Grievances All CenterPoint employees are responsible for receiving and recording grievances. Clients and providers may file grievances. Grievant has the right to be anonymous. Grievances are tracked and trends identified using the Alpha system. When a grievance is made…. CenterPoint staff attempt to resolve immediately If unable to resolve, the grievance is triaged by Quality Management Staff All are responded to within three business days Grievances that may adversely impact the health, safety and welfare of the client will receive immediate attention. This might include a call to DSS, DHSR or the police Resolving the Grievance If appropriate, the grievance may be referred directly to the provider for resolution. When that occurs, CenterPoint staff will: Obtain consent of the complainant to talk to the provider on their behalf Contact the provider, explain the concern, and request their aid in satisfying the complainant Conduct any necessary follow-up activities to assure resolution Providers should expect… Phone call as initial contact Identify a point person for resolution An expectation of collaboration with the grievance and CenterPoint Staff Sense of urgency to resolve We strive to resolve all grievances in 10 Days! Investigations Referral to External Agency: Division of Health Service Regulation: If CenterPoint receives a grievance related to a licensed facility/program we are required to report to DHSR for investigation. Department of Social Services: Any grievance involving an allegation of Abuse, Neglect, or Exploitation MUST be reported to the appropriate DSS office. CenterPoint Network Investigations: If the Network Operations staff determines an investigation is appropriate the provider monitoring team will be assigned accordingly. What should Provider expect during a Network Operations investigation? Announced or unannounced site visit Possible record review Possible staff and client interviews Timely decision (less then 30 days) Unsubstantiated Substantiated Partially Substantiated You will receive documentation Plan of Correction may be necessary Resolution Achieved! Letter is sent to the grievant Data is recorded Information pertaining to grievances is shared with: CenterPoint’s Global Continuous QI Committee CenterPoint’s Human Rights Committee Appropriate CenterPoint Internal Committees (CFTs) Credentialing Committee NC Division of MH/DD/SAS Including Program Integrity Corporate Compliance Program CENTERPOINT COMPLIANCE POLICY STATEMENT • Compliance is…. – Either a state of being in accordance with established guidelines, specifications, or legislation; or the process of becoming so. • CenterPoint is…… – Dedicated to maintaining excellence and integrity in all aspects of operations including professional and business conduct. – Committed to compliance with relevant laws and regulations governing the management of behavioral health services. – Committed to high ethical standards in conducting its business affairs and dealings with employees, providers, payers and the community. • CenterPoint employees, officers and contractors assume personal responsibility for honoring this commitment. CORPORATE COMPLIANCE CODE OF CONDUCT “BIG 8” 1. 2. 3. 4. 5. 6. 7. 8. Employee Responsibility Legal Compliance Business, Billing and Coding Ethics Confidentiality Conflict of Interest Business Relationships Protection of Assets Corporate Culture Any and all suspected violations of the code of conduct must be reported. CORPORATE COMPLIANCE/PROGRAM INTEGRITY FRAUD, WASTE AND ABUSE REFERENCES/AUTHORITY 42 CFR 438 (Managed Care) 42 CFR 434 (Contracts) 42 CFR 455 and 456 (Program Integrity and Utilization Control) NC Medicaid State Plan NC G.S. 108A- 70.1 thru 70.17 (False Claims) NC G.S. 108C (Medicaid and Health Choice Provider Requirements) 10A NCAC 22F (Program Integrity) FRAUD, WASTE AND ABUSE/ PUBLIC CONCERN Fraud, waste and abuse takes money from persons in need, including children, elderly and the disabled. Identifying, investigating and recovering Medicaid monies that are billed inappropriately is important to make sure individuals receive needed services and supports. Prevention and education is equally important to prevent fraud, waste and abuse from ever occurring in the first place. Fraud, waste and abuse costs taxpayers millions of dollars every year. The majority of providers and their billings are honest and accurate; however all it takes is one dishonest provider consistently billing inappropriately, over a period of time, to cost the system millions of dollars and to prevent services from being accessible to those who need them. PROGRAM INTEGRITY/ MCO RESPONSIBILITY Ensure integrity in the Medicaid Managed Care Program. Establish clear policies and procedures for the selection and retention of providers, including credentialing and re-credentialing. Monitor providers regularly to determine compliance and to take corrective action if there is a failure to comply. Provide education to enrollees, providers and MCO staff regarding fraud, waste and abuse including reporting requirements. Implement mechanisms to prevent, identify, investigate and remediate instances of fraud, waste and abuse. Conduct claims audits, clinical reviews and site reviews to determine quality of care, appropriateness of care, accuracy of billing and outliers of utilization of services. ALL staff must report any suspected case of fraud, waste and abuse. PROGRAM INTEGRITY/ PROVIDER RESPONSIBILITY Comply with all State and Federal regulations. Develop agency specific Corporate Compliance Plan to include method of preventing, detecting and addressing fraud, waste and abuse. Conduct regular quality assurance activities and self-audits to prevent, detect and address fraud, waste and abuse. Submit claims that are accurate & consistent with submission guidelines. Provide training on fraud, waste and abuse, to include reporting methods. Designate someone to be your compliance officer. Promote open lines of communication between corporate compliance officer, staff and MCO. Corporate compliance plan and training should include areas specific to behavioral health including professional conduct, ethics and conflict of interest. PROGRAM INTEGRITY/TERMS PROVIDER ABUSE ◦ 10a NCAC 22F .0301 “Includes any incidents, services, or practices inconsistent with accepted fiscal or medical practices which cause financial loss to the Medicaid program or its beneficiaries, or which are not reasonable or which are not necessary.” (i.e. provision of services that are not medically necessary) PROVIDER FRAUD ◦ Deliberate submission of claims for services not actually rendered, or billing for higher-priced services than those actually delivered. ◦ Submission of claims for payment for which there is no documentation. ◦ Billing for services that are provided by an unqualified or unauthorized person. ◦ Double billing and excessive billing beyond 24 hour period. PROGRAM INTEGRITY/TERMS CONFIDENTIALITY 10A NCAC 22F .0106 ◦ “All investigations by the North Carolina Division of Medical Assistance concerning allegations of provider fraud, waste, abuse, over-utilization, or inadequate quality of care shall be confidential, and the information contained in the files of such investigations shall be confidential.” Exceptions as required by legal proceedings apply. ◦ Any individual who reports suspected cases of fraud, waste and abuse may request to remain anonymous and the MCO will make every effort to maintain this anonymity when requested. MEDICAL ASSISTANCE PROVIDER FALSE CLAIMS ACT (MAPFC) OF 1997 The False Claims Act makes it unlawful for any Medicaid provider to knowingly make or cause to be made, a false claim for payment. Under MAPFC, “knowingly” is defined as: ◦ Has actual knowledge of the information. ◦ Acts in deliberate ignorance of the truth or falsity of the information. ◦ Acts in reckless disregard of the truth of falsity of the information. CREDIBLE ALLEGATION OF FRAUD PER 42 CFR 455…. CREDIBLE ALLEGATION OF FRAUD = SUSPENSION OF MEDICAID PAYMENTS DMA must suspend all Medicaid payments to a provider after the agency (DMA) determines there is credible allegation of fraud for which an investigation is pending under the Medicaid program against an individual provider or entity unless the agency (DMA) has good cause to not suspend payments or to suspend payment only in part. Only DMA can suspend Medicaid payments based on credible allegation of fraud, waste and abuse; however the MCO may suspend payment based on administratively based concerns. PROVIDER SANCTIONS & REMEDIAL MEASURES Termination of provider’s participation Suspension of payment Recoupment of overpayment Warning letters Suspension of a provider for a period of time Probation of provider participation Pre-payment reviews Post-payment reviews Corrective action plans Additional training and/or technical assistance Focused monitoring reviews Provider lock-out TO REPORT PROVIDER FRAUD, WASTE AND ABUSE Contact CenterPoint Human Services- Corporate Compliance Officer at 336-714-9114 or our dedicated email address at compliance@cphs.org or Contact the Division of Medical Assistance by calling the DHHS Customer Service Center at 1-800-662-7030 (English, Spanish) or Call the Medicaid fraud, waste and program abuse tip line at 1-877DMA-TIP1 (1-877-362-8471) or Call the Health Care Financing Administration Office of Inspector General’s Fraud Line at 1-800-HHS-TIPS (1-800-447-8477) or Call the State Auditor’s Waste Line at 1-800-730-TIPS (1-800-7308477) TO REPORT RECIPIENT FRAUD, WASTE AND ABUSE Contact CenterPoint Human Services- Corporate Compliance Officer at 336-714-9114 or our dedicated email address at compliance@cphs.org or Contact your local County Department of Social Services or Contact the Division of Medical Assistance by calling the DHHS Customer Service Center at 1-800-662-7030 (English, Spanish) or Call the Medicaid fraud, waste and program abuse tip line at 1-877-DMA-TIP1 (1-877-362-8471) Contracts, Claims and Billing As of February 1, 2013 CenterPoint became a closed provider network. Therefore, to be reimbursed for services rendered to Medicaid and state funded clients, YOU must complete the credentialing process for each practitioner, location and service you wish to deliver, and make SURE you have a contract in place that specifically lists those sites and services. Any and all services (including the sites they are delivered from) that you expect to be reimbursed for must be included in your contract. Contract Auth Provider Changes Contact CenterPoint’s Network Department for any of the following changes: Change in ownership Subcontracting Any changes in a site, including your corporate address If you want to discontinue a service or close a site (you must submit written information) If you want to add a service or a site (you MUST submit a written request IN ADVANCE) Claims Submission – First Steps Provider is contracted to deliver services. Complete Provider data is submitted. This includes sites, clinical staff, credentials, NPI’s , and taxonomy numbers. Services delivered are in your contract. client is eligible for services. Service Authorizations – if needed – has been requested and approved. Claims Submission – Eligibility Verification Verify that Client’s Medicaid originated within CenterPoint’s catchment area - Forsyth, Davie, Stokes and Rockingham Counties and obtain appropriate authorization . Medicaid eligibility may change from month to month. At each visit, Providers should verify current eligibility. Medicaid is payer of last resort. Coordination of Benefits is required – bill all primary third party payers prior to billing CenterPoint. Authorization does not guarantee payment of claim Claims Submission All Providers are required to file claims electronically in one of the two following formats. HIPAA Compliant Standard EDI Transaction Files 837 Institutional Health Care Claim (version 5010) 837 Professional Health Care Claim (version 5010) Direct Data entry through Alpha MCS Provider Portal CMS 1500 for Professional claim UB 04 for Institutional claims Claims Submissions - Clearinghouses For 837 billers If you use a Clearinghouse to submit your claims, you will need to direct the claims submissions to Emdeon. Emdeon is the only Clearinghouse that CenterPoint will accept claims from. 835 is not being sent by via Emdeon, that will need to be downloaded from AlphaMCS Provider Portal. Claims Submission Time limits for filing Claims All inpatient and outpatient claims must be received by CenterPoint within 90 days of the service date to be accepted for processing and payment. Claims Payment The Checkwrite Schedule will be published on our Website and for the first contract year we are following DMA’s Medicaid Schedule. All claims payments will be made electronically by automatic deposit to the account specified by the Provider’s Electronic Funds Transfer(EFT) Agreement. Claim Status To check the status of a claim, you will need to log on Alpha MCS Provider Portal and search by client under the Claims module. Claims Submission Denials and Claim Inquiries Denial reasons are listed on your Alpha MCS RA report. All denial codes will be published on our website. If you need help with denials or have claim inquiries that can not be resolved after reviewing Alpha MCS Claims module, you may contact us via secure Email claims@cphs.org All emails with Protected Health Information must be sent to securely via CenterPoint Zixmail. Contact your assigned Claims Specialist by phone. Alpha Training AlphaMCS Provider Portal training is required for access. Please register for AlphaMCS training via our website: http://www.cphs.org/AlphaProviderTraining.aspx For EDI transaction files 837 –P or 837 I ( version 5010) To initiate testing processes for format and content please contact: CenterPoint Human Services’ IT Help Desk by either: Phone - (336) 714-9139 or e-mail - HelpDesk@cphs.org. Network Operations Routine Monitoring Process Incident Reporting Process Disputes NC TOPPS Monitoring Process Effective on 3/1/14, all LME-MCOs will use the revised Routine Monitoring Process to conduct provider monitoring. Routine monitoring occurs at least every 2 years. Routine monitoring is required for all unlicensed services and for licensed services that are not monitored annually by DHSR. Monitoring Process (cont’d) Only routine post payment reviews are completed for licensed services reviewed by DHSR annually. The MCOs do not currently have monitoring responsibilities for Therapeutic Foster Care, Hospitals or ICF-IDD facilities. Monitoring Tools All MCOs in NC use the same monitoring tools. Tools are found at http://www.ncdhhs.gov/mhddsas/providers/provider monitoring/index.htm. Current Tools Routine Monitoring Tool for Provider Agencies Routine review, site health and safety review, post payment review Routine Monitoring Tool for Licensed Independent Practitioners (solo and group) Office site review, LIP review, post payment review Review Scoring The minimum overall score for the routine review tool is 85%. The threshold for passing each section is also 85%. A Plan of Correction may be requested for identified systemic issues even for providers scoring 85% or greater. IRIS – Incident Response Improvement System WHAT IS IRIS? Web based incident reporting system for reporting and documenting responses to Level II and Level III incidents involving clients receiving Mental Health, Intellectual/Developmental Disabilities and Substance Abuse (MH/DD/SAS) services. WHO MUST REPORT? Category A Providers: providers licensed under NC General Statutes 122c (except hospitals) Category B Providers: providers of non-licensed periodic or community based MH/DD/SAS services Quarterly Provider Incident Report Category A and B providers must also submit a “Quarterly Provider Incident Report” each quarter (due on the 10th day of the month following each quarter) which summarizes Level I as well as Level II and Level III incident data per provider site. Important Information Incident Reporting page on the NC Division of MH/DD/SAS website: http://www.ncdhhs.gov/mhddsas/providers/NCincidentresponse/index.htm Contacts for Incident Reporting Provider Quarterly Incident Reports : Ed Eklund eeklund@cphs.org, 714-9135 IRIS / Technical Assistance: Ed Eklund (A-M) eeklund@cphs.org , 714-9135 Claudia Salgado (N-Z) csalgado@cphs.org , 714-9133 Karen Dingwall kdingwall@cphs.org , 714-9116 Disputes Provider Administrative Disputes (Examples) • • • • Issues related to timely filing of claims Network accessibility issues Failure to submit requested medical records Appeals of administrative denials Processing Administrative Disputes Complainant: Contacts Provider Affairs Specialist (PAS) via phone/fax/e-mail/letter or walk in Completes Provider Dispute Form and returns to PAS along with supplemental materials (optional) that support his/her case within 15 calendar days PAS: Reviews the form/returned materials and consults with other CenterPoint staff as needed Completes mediation of case, obtains approval from management and sends decision via certified mail to complainant within 20 business days from receipt of the Provider Dispute Form and supplemental materials, as applicable Provider Professional Competence Disputes (Examples) Participating (contracted) provider’s status within the provider network Potential quality of care or client safety issues Ethics Clinical Boundaries Dual Relationships Professional competence to perform contracted services Professional competence or conduct that could result in a change in provider status Primary Difference with Provider Professional Competence Disputes 1st and 2nd level panels: Comprised of two Provider Council, Steering Committee members and one clinical peer (licensed CenterPoint staff) PAS randomly selects 1st and 2nd level panel members, as applicable, and facilitates the review and deliberation of the case (20 business days, plus 5 business days for each level involved). Accessing Necessary Forms The Provider Administrative Dispute and Provider Professional Competence Dispute procedure and form(s) are available on the CenterPoint website. www.cphs.org At top of home page, click on the “Providers” tab In left margin, click on Provider Network Click on applicable entry under Provider Resources NC-TOPPS NC-TOPPS The NC-TOPPS interview is required for clients formally admitted to the LME/MCO and who are receiving qualifying MH and/or SA services from a publicly funded source. Managed by NC DMH/DD/SAS NC-TOPPS is a self-guided, web-based system for gathering outcome and performance data on behalf of MH/SA clients It provides reliable information used to measure the impact of treatment and improve service quality Provider Agencies and LME/MCO Superusers have oversight responsibilities: manage user requests, track submissions and due dates, and change a client’s Qualified Professional (QP) Approved QPs and Data Entry Users (DEUs) can enter NC TOPPS interview data NC-TOPPS The NC-TOPPS system provides a One-Stop format to: Register with NC-TOPPS and create secure account-keep your user name and password for all future interactions Enter, update and search client data Create and manage personal information Complete Interviews and manage Episodes of Care Access Tracking and Reporting features NC-TOPPS RESOURCES NC-TOPPS Website: www.ncdhhs.gov/mhddsas/providers/NCTOPPS Help Desk- nctopps@ncsu.edu CenterPoint John Coble, Provider Affairs Specialist, Network Operations (336) 714-9117, jcoble@cphs.org Completion of Course In order for you to receive credit for this course with CenterPoint Human Services, you MUST click on the link below and complete the provider information, attestation, and evaluation. Please be sure you hit “submit” when you complete the form. Thank you. Attestation and Evaluation (http://www.cphs.org/attestation)