NHSN Enrollment
advertisement

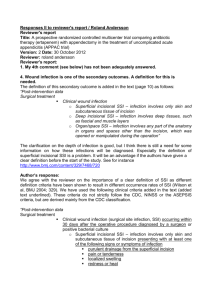
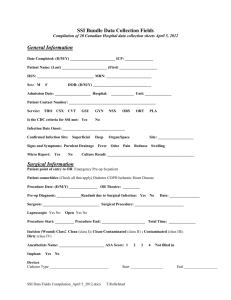
SURGICAL SITE INFECTION SURVEILLANCE STANLEY OSTRAWSKI, MS, RN, MT(ASCP), CIC Infection Preventionist Consultant Objectives • Explain how to calculate an SSI rate • Explain how to complete NHSN SSI forms using CDC definitions and protocols • Apply case definitions of procedure-associated infections to case studies Choosing Procedures to Monitor High Volume Requirements High Risk Sample 12 month Surveillance Plan Timeline Jan Feb Mar Apr May • CLABSI • SSI - HPRO • Surgical ABX Prophylaxis Jun • CLABSI • SSI - HPRO • Surgical ABX Prophylaxis • HCW Influenza Vaccine • CLABSI • SSI - KPRO • Surgical ABX Prophylaxis • HCW Influenza Vaccine • CLABSI • SSI - HPRO • Surgical ABX Prophylaxis • HCW Influenza Vaccine • CLABSI • SSI - KPRO • Surgical ABX Prophylaxis • HCW Influenza Vaccine • CLABSI • SSI - KPRO • Surgical ABX Prophylaxis Jul Aug Sep Oct Nov Dec • CLABSI • SSI - HPRO • Surgical ABX Prophylaxis • CLABSI • SSI - KPRO • Surgical ABX Prophylaxis • CLABSI • SSI - HPRO • Surgical ABX Prophylaxis • CLABSI • SSI - KPRO • Surgical ABX Prophylaxis • HCW Influenza Vaccine • CLABSI • SSI - HPRO • Surgical ABX Prophylaxis • HCW Influenza Vaccine • CLABSI • SSI - KPRO • Surgical ABX Prophylaxis • HCW Influenza Vaccine Denominator for Procedure 1. The reporting period is one month 2. Collect a procedure record for every procedure that was done during that month For example, if you plan to monitor KPRO procedures in July and 43 KPRO operations are done in July, then you should collect details with risk factor data on each of the 43 cases. Terms and Definitions • The data you report must use exactly the same terms and definitions – – – – Inpatient Outpatient Operative Procedure Operating Room Additional terms will be added as we specifically discuss SSI and PPP Definition: Inpatient A patient whose date of admission to the healthcare facility and the date of discharge are different calendar days. Definition: Outpatient A patient whose date of admission to the healthcare facility and the date of discharge are the same day Definition: Operative Procedure A procedure that 1. is performed on a patient who is an inpatient or an outpatient 2. takes place during an operation where a surgeon makes a skin or mucous membrane incision (including the laparoscopic approach) and primarily closes the incision before the patient leaves the operating room 3. is represented by an Operative Procedure Code NHSN Operative Procedure Codes Each NHSN operative procedure category is defined by a group of ICD-9-CM codes NHSN Operative Procedures When an NHSN Operative Procedure is selected for monitoring, all the procedures within that category must be followed CBGC -- Coronary artery bypass graft with only a chest incision (mammary donor site) CBGB – Coronary artery bypass graft with two incisions – chest incision and donor site (usually leg) These procedures are mutually exclusive for a single trip to the OR. A patient can never have both! Definition: Operating Room • A patient care area that meets the American Institute of Architects (AIA) criteria for an operating room • May include: • Traditional operating room • C-section room • Interventional radiology room • Cardiac cath lab Duration Duration: Record the hours and minutes between the skin incision and skin closure. Do not record anesthesia time! Additional Rules about Duration • If more than one NHSN operative procedure is done through the same incision during the same trip to the OR, create a record for each procedure and use the total time for the duration of both Example: Mr. Jones goes to the OR and has a coronary artery bypass graft with a [leg] donor site (CBGB) and also a mitral valve replacement (CARD). The time from the first incision until skin closure is 5 hours. A Denominator for Procedure record is completed for the CBGB and another for the CARD. The duration for each is recorded as 5 hours and 0 minutes. Additional Rules about Duration • If the patient goes to the OR more than once during the same admission and another procedure is performed through the same incision within 24 hours of the original incision, report the combined duration of operation for both procedures Example: Fred Smith had a small bowel resection done on Tuesday morning which had a duration of 3 hours and 10 minutes. On Tuesday evening, he was returned to the OR where an exploratory laparotomy (XLAP) was done through the same incision to repair a leaking anastamosis. The XLAP cut time was 1 hour and 10 minutes. The Duration for each procedure – SB and XLAP -- is reported as 4 hours and 20 minutes Wound Class Wound class is an assessment of the likelihood and degree of contamination of a surgical wound at the time of the operation C = Clean CC = Clean Contaminated CO = Contaminated D = Dirty Wound Class Clean Uninfected wound with no inflammation Respiratory, alimentary, genital or uninfected urinary tract are not entered Primarily closed Closed drainage, if needed Clean-Contaminated Respiratory, alimentary, genital, or urinary tracts entered under controlled conditions and without unusual contamination Include operations on biliary tract, appendix, vagina, oropharynx if no evidence of infection or major break in technique Wound Class Contaminated Open, fresh, accidental wounds Major breaks in sterile technique or gross spillage from the GI tract Includes incisions into acute, nonpurulent inflamed tissues Dirty Old traumatic wounds with retained devitalized tissue Wounds involving existing clinical infection or perforated viscera Wound Class Cases Case Susanne undergoes an appendectomy following 2 days of acute abdominal pain with rebound tenderness. At the end of the case, the surgeon indicates that the appendix had ruptured and the surgical area was irrigated and keflex was ordered for 3 days postoperatively. Fred has a cholecystectomy using a laparoscopic technique. The gallbladder was removed successfully with no breaks in operative asepsis. George has a KPRO revision. When the surgeon makes the incision into the surgical site, she notes that the knee joint demonstrates purulent matter and inflammation. A specimen is obtained and sent to the laboratory which grows S. aureus (MSSA). Wound Class 3 2 4 ASA Class An assessment score by the anesthesiologist of the patient’s preoperative physical condition using the American Society of Anesthesiologists Classification of Physical Status schema 1. Normally healthy patient 2. Patient with mild systemic disease 3. Patient with severe systemic disease that is not incapacitating 4. Patient with an incapacitating systemic disease that is a constant threat to life 5. Moribund patient who is not expected to survive for 24 hours with or without operation Implant Implant: A nonhuman-derived object, material, or tissue that is permanently placed in a patient during an operative procedure and is not routinely manipulated for diagnostic or therapeutic purposes. Examples include: porcine or synthetic heart valves, mechanical heart, metal rods, mesh, sternal wires, screws, cements, and other devices. Also includes surgical clips and staples left in permanently. Ella Baxter underwent a CBGB (coronary artery bypass graft with a leg donor site). During the same operation, she had a mitral valve replacement (CARD)with a porcine valve. Did Ms. Baxter’s procedure include an implant? Did Ms. Baxter’s procedure include a transplant? Surgical Site Infection (SSI) Introduction • SSI occurs in 2 – 5% of patients undergoing inpatient surgery in the U.S. • Approximately 500,000 each year • Each SSI is associated with approximately 7-10 additional postoperative hospital days • Attributable cost estimates of SSI range from $3,000 - $29,000 each Minimum SSI Surveillance • Review of patient and laboratory records during the patient admission • Review of surgical patient readmissions • Microbiology data from postoperative wound cultures SSI Post-discharge Surveillance Post-discharge surveillance methods may also include: • Examination of patient surgical site during follow-up visits to physician office or surgery clinic • Surgeon surveys by mail or phone • Review of medical records for postoperative visits The definition of the specific SSI must be met for any methodology used! SSI Definitions Superficial Incisional • SIP • SIS Deep Incisional • DIP • DIS Organ/Space • • • • • • • • BONE BRST CARD DISC EAR EMET ENDO etc. Superficial Incisional SSI Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 1992;13(10):606-8. Superficial Incisional SSI SIP and SIS Superficial incisional primary (SIP) A superficial incisional SSI that is identified in the primary incision in a patient that has had an operation with one or more incisions (e.g., C-section incision or chest incision for coronary artery bypass graft with a donor site [CBGB]) Superficial incisional secondary (SIS) A superficial incisional SSI that is identified in the secondary incision in a patient that has had an operation with more than one incision (e.g., donor site [leg] incision for coronary artery bypass graft with a donor site [CBGB]) Example Gretchen Dale delivers a baby by C-Section on August 23. On her 2-week postpartum visit to her surgeon, she notes yellow purulent drainage in the superficial incision. Does Gretchen have a surgical site infection? Is it a superficial SSI? Is it an SIP or an SIS? Deep Incisional SSI Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 1992;13(10):606-8. Deep Incisional SSI DIP and DIS Deep incisional primary (DIP) A deep incisional SSI that is identified in the primary incision in a patient that has had an operation with one or more incisions (e.g., C-section incision or chest incision for coronary artery bypass graft with a donor site [CBGB]) Deep incisional secondary (DIS) A deep incisional SSI that is identified in the secondary incision in a patient that has had an operation with more than one incision (e.g., donor site [leg] incision for coronary artery bypass graft with a donor site [CBGB]) Examples Charles has purulent drainage from the chest incision following a coronary artery bypass graft with a donor site from the left leg. He also has redness and pain at the leg incision. The doctor opens and drains the incision. No culture is done for either site. How should this be reported to NHSN? A. SIP B. SIS C. Both D. Neither Organ/Space SSI Specific event types that must be used to differentiate organ/space SSI BONE Osteomyelitis JNT Joint or bursa BRST Breast abscess/mastitis LUNG Other infections of respiratory tract CARD Myocarditis/ pericarditis MED Mediastinitis DISC Disc space ORAL Oral cavity EAR Ear, mastoid OREP Other respiratory EMET Endometritis OUTI Other urinary ENDO Endocarditis SA Spinal abscess EYE Eye, other than conjunctivitis SINU Sinusitis GIT GI tract UR Upper respiratory IAB Intraabdominal, NOS VASC Arterial or venous IC Intracranial VCUF Vaginal cuff Organ/Space SSI http://www.cdc.gov/nhsn/PDFs/pscManual/17pscNosInfDef_current.pdf has had more than one operation… If a patient has several NHSN operations prior to an SSI, report the operation that was performed most closely in time to the infection date Example: Mr. Smith underwent a SB on 12/02/2011. Three days later, he went back to surgery to repair a leaking anastamosis (OTH). He developed an intraabdominal abscess on 18/03/2011. This SSI is attributed to the second procedure (OTH), not the SB Example Robert Jones undergoes a coronary artery bypass graft (CBGB) in which the surgeon obtained a donor vessel from a site in Robert’s left leg. 5 days postoperatively, Robert had pain and edema in the leg incision. The surgeon opened the superficial incision, drained the pus, and irrigated the wound. Does Robert have a superficial incisional SSI? Is it a SIS or SIP? SSI – Event Details Select the specific elements of the definition that were used to identify this infection Secondary BSI • A culture-confirmed BSI associated with a documented HAI at another site • If a primary infection is cultured, the Secondary BSI must yield culture of same organism and exhibit the same antibiogram as the primary HAI site Example: Mrs. Jones grows E. coli in her urine (>100,000 col/cc) and in her blood. Both organisms have the same antimicrobial susceptibility pattern. The UTI is reported with a secondary BSI. Example: Mr. Smith grows A. baumanii in his surgical wound which is resistant to amikacin and levofloxin but sensitive to other tested antimicrobials. He is also growing A. baumanii in his blood, but it is susceptible to amikacin. Secondary BSI (cont.) • If an infection is identified and no culture is used to meet the infection criteria and a blood culture is positive, then the first infection is considered primary and the bloodstream infection is reported as secondary. The organism cultured from the blood is reported as the organism for the primary site. Example: 6 days postoperatively, Miss Green has an abdominal abscess, confirmed by CT scan. On the same day, her blood is drawn and grows Bacteroides fragilis. The infection is reported as an SSI-GIT (organ space SSI) with a secondary BSI. The organism is reported as B. fragilis Mr. Fuentes has a central line for infusion of fluids during a complex abdominal procedure and the blood culture grows Bacteroides fragilis on the 4th postoperative day. His surgeon states that the BSI is secondary to the operation – he says there was probably a small leak in the anastamosis. Does Mr. Fuentes have a secondary BSI? A. Yes, the primary infection is SSI-IAB B. Mr. Fuentes has both a CLABSI and an SSI-IAB C. Mr. Fuentes has a CLABSI – not secondary to an SSI SSI Rate * Stratify by: •Type of NHSN operative procedure •Basic NHSN Risk Index NHSN Basic Risk Index •The index used in NHSN assigns surgical patients into categories based on the presence of three major risk factors: The patient’s SSI risk category is simply the number of these factors present at the time of the operation Example of NHSN Risk Index Elements Operation > duration cut point Wound class ASA Score Risk Index Category Patient #1 Yes IV 4 3 Patient #2 No I 1 0 Patient #3 Yes II 1 1 2008 NHSH Report – SSI Rates George Bolthouse, 51 • The patient has an aortic aneurysm repair (AAA) surgery and is discharged, then comes back about a week later with peritonitis. A needle aspiration of purulent material from the abdomen grows P. aeruginosa. The surgeon attributes the peritonitis to a perforated diverticulum. Should this be counted as a surgical site infection associated with the AAA? A. Yes – this is an organ/space SSI (IAB) B. No, a perforated diverticulum is a complication of the surgery, not an infection Tom Jones, 32 • Mr. Jones is a post op hernia (HER) patient that was seen in the ER 6 days post op with a large cellulitis, a pain level 10/10, swelling, tenderness, and redness. He was admitted for treatment with antibiotics. He had leukocytosis and an elevated CRP (199). Serous drainage from the incision was no growth. Is this a superficial incisional or a deep incisional SSI? A. Superficial incisional SSI B. Deep incisional SSI C. Neither – the surveillance criteria for SSI are not met Bruce Keller • Patient underwent a KPRO procedure at our hospital • The patient was discharged to a Is this an SSI? Should it rehab facility and be reported? sustained a fall one As long as there is no indication week later that the wound dehisced • The incision dehisced because it was infected, it would and became infected not be reported. Mary Blair, 77 • Patient had a hip prosthesis procedure (HPRO) on 2/4/08. She had an infected AV dialysis graft rupture on 7/6/08 – blood cultures grew Staph aureus and she was placed on antimicrobials for treatment of the bloodstream infection. On 7/21/08, Jane experienced pain in the hip joint – radiographic evidence on gallium scan shows an abscess at the hip prosthesis site– culture of hip was no growth. Should this be counted as a SSI associated with the HPRO if the AV graft was the primary infection and it appears that the hip became seeded secondarily? A. Yes, this is an SSI B. No, this infection is secondary to the bloodstream infection Question? • Which of the following does not meet the criteria for a superficial incisional SSI if identified within 30 days after the procedure? A. Culture of fluid obtained from superficial incision grows MRSA B. Physician documents “superficial surgical site infection” in patient record C. Purulent drainage noted from superficial incision D. Physician documents “cellulitis” at incision site What do you do about high rates? • • • • Share data with surgeons either way (High or Low) Type of surgery Same surgeon, OR room, etc Surveillance methods – Extensive vs minimal. • Look at SCIP measures – Prophylactic ABX • Timing important • Is MRSA a problem? • Are doses weight based? • Look at other pre op measures • Post op measures