Slide Presentation - Curriculum for the Hospitalized Aging Medical

CHAMP
Early to Bed, Early to Rise:
The Adverse Consequences of Bed Rest
Deón Cox Hayley, DO
University of Chicago
Objectives
What you want to teach, ie goals and their explicit content
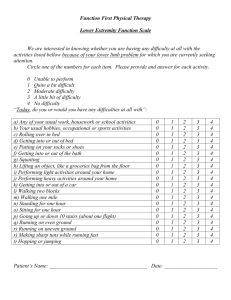
Poor functional outcomes associated with hospitalization in the elderly
Specific organ pathophysiology associated with prolonged bed rest
Most hospitalized patients should not be on complete bedrest.
What you want students to begin doing as a result of the learning in this module
Recognize the serious consequences of bedrest
Identify certain consequences as potentially preventable and be able to explain these to trainees.
Change physician’s perception of writing an order for physical therapy as fulfilling their obligation to help patients get out of bed
How you expect to teach students to know/do, ie specific teaching methods
Power point lecture with pictures/graphics
Case based lecture
Discuss exceptions to indications for getting out of bed
• Brainstorm ways to broaden the approach to getting people out of bed.
Outline--Adverse Effects of Bed Rest
1. Case
2. History of use
3. Elderly as important sub-group a. special concerns
4. How Bed Rest affects: a. Function b. Individual organ systems
5. Summary
Get people out of bed!
Patient G.J.
78 y/o female
Admitted to sub-acute rehabilitation (in
NH)
HPI: s/p surgical repair of traumatic right knee fracture then dislocation
PMH: OA, DM, HTN, bipolar disease
Soc Hx: Husband does most IADLs, independent in ADLs and ambulatory
Exam:
• Gen: flattened affect
• Obese
• Long leg cast on right
(thigh ankle)
Function:
• On admission
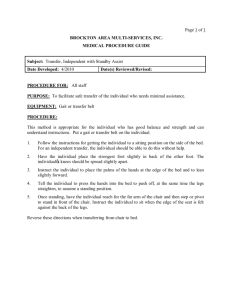
– NWB on right leg, transfer on left leg
– Needed assistance of 2
• Goal
– Get back to previous status at home
Knee fracture pain narcotics constipation
Bed rest weight gain worsened DM weakness poor motivation delirium urinary retention incontinence pressure sores
IMMOBILITY
Follow up
• Discharged home, walking with a walker
Sick role model
• Doctor authority
• Hospital disorienting, threatening to older patients
• Study of elderly hospitalized patients showed that 72% didn’t ambulate in the halls at all.
Mahoney J. Wisc Med J. 1999.
Practice of using bed rest
Dramatically decreased:
1. OB
2. Surgery a. General b. Orthopedics
3. Cardiology a. Post-MI b. CHF
Still too much in general medicine
For if the whole body is rested much more than is usual, there is no immediate increase in strength. In fact, should a long period of inactivity be followed by a sudden return to exercise there will be an obvious deterioration.
-Hippocrates
Chadwick J, Mann Wm. The Medical Works of Hippocrates. Oxford,
UK: Blackwell, 1950 p. 140.
Review of literature on the utility of bed rest
• 39 trials of bed rest for 15 different conditions
(n=
5777)
• 24 trials investigating bed rest following a medical procedure
– no outcomes improved significantly
– 8 worsened significantly
• 15 trials investigating bed rest as a primary treatment
– no outcomes improved significantly
– 9 worsened significantly
Allen C et al. Bed rest: A potentially harmful treatment needing more careful evaluation. Lancet 354:1229-33, 1999.
Why are the elderly more at risk?
1. Co-morbidities
2. Decreased reserve
What do we know about the adverse effects of bed rest?
1. Effects on total functioning
2. Effects on individual organs/systems
• Elderly admitted to the hospital:
– At discharge, 31% deteriorated in ADLs
– At 3 months, 51% had either died or worsened in functional status
Sager MA, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 156:645-52, 1996.
• Continued decline in function after hospitalization
– 2 days post-hospitalization, 65% lost ability to walk
– At discharge, 2/3 did not improve in function
10% deteriorated further
Hirsch et al. The natural history of functional morbidity in hospitalized older patients. JAGS 38:1296-1303, 1990.
• One month post-hospitalization
– 59% were not back to baseline
• Risk Factors for functional decline:
– age
– cognitive impairment,
– low social activity,
– pre-hospitalization functional impairment.
Innouye S et al. A predictive index for functional decline in hospitalized elderly medical patients. JGIM 8:645-52. 1993.
Sager MA. Hospital Admission Risk Profile (HARP): Identifying older patients at risk for functional decline following acute medical illness and hospitalization. JAGS 44:251-7, 1996.
Hansen K et al. Risk factors for lack of recovery of ADL independence after hospital discharge. JAGS 47(3):360-5. 1999.
Pathophysiology--organ systems
Man was designed … to function more or less in the upright posture in earth’s gravitational environment. Thus, the deconditioning that occurs during bed rest would be viewed as a departure from the optimal posture.
- Greenleaf J.
CV
1. Change in hemodynamics
2. Orthostatic incompetence
3. Changes in peripheral circulation
Browse NL: The Physiology and Pathology of Bed Rest.
Springfield, Illinois, Charles C. Thomas Publisher, 1963.
CV
1.
Eleven percent of circulating blood shunted to the central circulation initial in cardiac output and stroke volume
2.
With increased time in bed, HR increases daily
3. Cardiomegaly, mild though progressive
Chobanian AV et al, The metabolic and hemodynamic effects of prolonged bed rest in normal subjects. Circulation 49:551, 1974.
Orthostasis
• Prolonged bed rest twice the usual fall in
SV and CO with standing.
• Pooled blood in lower extremities increased HR and alpha- adrenergic response
• Symptoms occur early and are profound
Hung J, et al. Mechanisms for decreased exercise capacity after bed rest in normal middle-aged med. Am Jour Card. 51;344-8. 1983.
CV response to activity after bed rest
1. Aging cardiac dilatation maximum heart rate
2. Immobility adrenergic system upregulation and reserve to increase CV signals in response to initial exercise
Respiratory
1. Restrictive impairment
2. Alteration in blood flow
Pulmonary Blood Flow
1. Highly perfused areas become posterior V:Q ratio changes
2. Blood flow changes ( central circulation and tissue hydrostatic pressure) pulmonary edema
Muscle
• Rapid loss of strength
– 5% per day
– 50% of strength lost in first 3 weeks
• Leg strength loss more quickly than arms
• Atrophy twice as fast if muscle shortened
Muller LA: Influence of training and of activity on muscle strength.Aron Physics Med Rehab 51:449, 1970.
Skeletal
• Bone loss 0.9 % per week
• Both increased absorption as well as cessation of new bone formation
Wheldon GD: Disuse osteoporosis: Physiological aspects. Calcif tissue Int 36:5146, 1984.
Joint changes
• Joint loading important to keep healthy cartilage
• Fibrosis and ankylosis
• Decreased lubrication
• Diminished cartilage smoothness within one week
• Osteophyte formation within two weeks
Gastrointestinal
• Increased risk of aspiration
• Increased transit time
– Anorexia
– Constipation
Genitourinary
1. Diuresis 300-600 cc in first week then stable
2. Hypovolemia
3. Bladder evacuation impaired
CNS
• EEG slowing on young immobilized patients who did not have any other sensory deprivations
Skin- break down
1. With age, skin is less resistant barrier
2. Mechanics of pressure, friction, traction and maceration
• Effects on other systems:
– endocrine
– immune
– sensory changes