Managing Care While _x000b_Staying in the Moment
advertisement

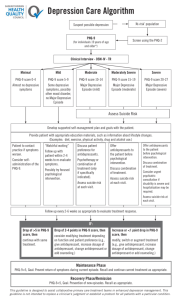
Managing Care While Staying in the Moment October 8, 2015 Learning Objectives 1. List and describe the core components of the IMPACT/Collaborative Care model of care 2. Identify ways to blend IMPACT and other evidencebased models such as behavioral health consultation 3. Describe the IT and clinical infrastructure needed to provide population-based primary care behavioral health 4. Identify the value of participating in a learning collaborative Definition of Integrated Care • The care that results from a practice team of primary care and behavioral health clinicians, working together with patients and families, using a systematic and costeffective approach to provide patient-centered care for a defined population • This care may address mental health, substance abuse conditions, health behaviors, (including their contribution to chronic medical conditions), life stressors and crisis, stress-related physical symptoms, ineffective patterns of health care utilization Peek, C.J. National Integration Academy Council (2013). Lexicon for behavioral Health and Primary Care. Integration: Concepts and Definitions. Developed by Expert Consensus. In Agency for Healthcare Research and Quality The “Face” of Integrated Care • 78 year old male whose family reports depression, agitation, and memory loss. Presents to PCP who orders neurology referral and involves BHC. BHC does phq9 and Montreal cognitive assessment and determines fairly major impairment and depression. SSRI discussed, but patient isn't interested. Never goes to neuro. Later on, he shows up as a transition of care from a psychiatric hospital and is discharged on 2 Alzheimer's meds, Seroquel, and Prozac. Our PCP is very nervous about continuing those meds but consulted with our psychiatrist who educated on the why, advised on what questions to ask the family to determine the root of some of the issues they are seeing, and advised on some possible dosage changes. The PCP was then able to prescribe and the BHCs worked with the family to check in on the depression. The goal for this patient was to keep him out of hospitalization. What the patient really wanted was to go back to Mexico, so the BHC also worked on developing a plan to support this with the patient's daughters who were initially unsupportive. The “Face” of Integrated Care • Patient presents to PCP as depressed with main complaint lack of sleep, no appetite, no interest in doing things, irritability, and recent negative changes at work. He reported insomnia and trouble at home due to the aforementioned reasons. Had failed SSRI trials previously. Got referred to BHC and provider had already started on a tricyclic but he hated it. He had a BHC consult to work on identifying priorities, skill building, general support and a PHQ 9 initial score 15. With psych consult, decided to switch to Remeron. After three weeks he came back and was a changed man. The phq9 went down to 4. He decided to stay on the Remeron for two more months but his depression was so improved and with his new skills he had resolved so many of his source issues that he came off. We still touch base when he comes in to see PCP but the adjustment disorder has completely resolved and he knows we are there when he needs us. Rarely Only Behavioral Disorder Cancer 10-20% Neurologic Disorders 10-20% Chronic Physical Pain 25-50% Mental Health/ Substance Use Smoking, Obesity, Physical Inactivity 4070% Diabetes 10-30% Heart Disease 10-30% What does work? Core Principles of IMPACT/Collaborative Care • Patient-centered team care/Collaborative Care – Collaboration not co-location – Team members have to learn new skills • Population-based care – Patients tracked in a registry; no one falls through the cracks • Measurement-based treatment to target – Treatments are actively changed until the clinical goals are achieved • Evidence-based care – Treatments used are evidence-based • Accountable care – Providers are accountable and reimbursed for quality of care and clinical outcomes, not just the volume of care provided Collaborative Care Team Care Model Two processes: 1. Systematic diagnosis and outcomes tracking – PHQ-9 to facilitate diagnosis and track depression outcomes 2. Stepped Care – Change treatment according to evidence-based algorithm if patient is not improving – Relapse prevention once patient is improved Primary Care Provider Role • Oversees all aspects of patient’s care • Diagnoses common mental disorders – Brief screeners (e.g., PHQ-9, GAD-7) • Starts & prescribes pharmacotherapy • Introduces collaborative care team and care manager • Collaborates with care manager and psychiatric consultant to make treatment adjustments as needed One Treatment Plan • Team-based care: patient, PCP, BHC, psychiatrist all involved in developing and carrying out the treatment plan • Regular communication through team huddles, shared appointments • All members of the team give consistent recommendations Two New “Team Members” Behavioral Health Clinician (BHC) Consulting Psychiatrist • Patient education/selfmanagement support • Close follow-up to make sure pts don’t ‘fall through the cracks’ • Support anti-depressant Rx by PCP • Brief counseling (behavioral activation, PST-PC, CBT, IPT) • Facilitate treatment change/referral to mental health • Relapse prevention • Caseload consultation for care manager and PCP (populationbased) • Diagnostic consultation on difficult cases • Consultation focused on patients not improving as expected • Recommend additional treatment/referral according to evidence-based guidelines BHC Role • Supports and collaborates closely with PCPs managing patients in primary care • Patient education/selfmanagement support • Brief counseling (behavioral activation, PST-PC, CBT, IPT) • Support anti-depressant Rx by PCP • Supports medication management by PCPs • Reviews cases with psychiatric consultant weekly • Facilitate treatment change/referral to mental health • Relapse prevention Psychiatric Consultant Role • Caseload-focused consultation supported by BHC • Better access: – PCPs get input on their patients’ behavioral health within a day/week vs. months – Focuses in-person visits on the most challenging patients • Regular communication: – Psychiatrist has regular (weekly) meetings with the BHC – Reviews all of the patients who are not improving and makes treatment recommendations Measurement-Based Care (PHQ-9) • Assists with identification and diagnosis • Tracks 9 core symptoms over time • Easy to use: can be self-administered and done over the phone • A good communication and teaching tool • Available in many languages: http://www.phqscreeners.com/ Population/Care Management • Use a clinical registry to: – Proactively follow up to prevent people from ‘falling through the cracks’ – Systematically track treatment response – Facilitate treatment planning and adjustment • Combat ‘clinical inertia’: patients staying on ineffective treatments for too long – Know when it is time to get consultation/get help and when it is time to change treatment Depression Registry Outcome Aim: Depression Improvement Outcome Aim information: Number of patients with a PHQ-9 >10 0 Number of patients with >50% improvement 0 Assessment month: Reassessment month: ID (non-PHI) Instructions: Please enter the individual's identifier in the blue column. Please enter the dates of the indivdual's first and second PHQ-9 assessments in the green columns. Please enter the indivdual's first and second PHQ-9 scores in the purple columns. Please do not enter or delete the numbers in the Days Apart or % Change columns - these compute automatically. As of: Date of 1st PHQ-9 1st PHQ-9 Score Date of 2nd PHQ-9 2nd PHQ-9 Score Days Apart Average Days apart: Average % Change: 9/17/15 % Change 2nd Assessment Due i2i Tracks Population Management Software Integrates data from internal and external systems, aggregating data about your entire patient population. i2i Tracks Transforming Practice Through Participation in a Learning Collaborative What is a learning collaborative? Structured approach for change Adopt best practices in multiple settings Time-limited learning process Uses adult learning principles & techniques Shared learning and collaboration Breakthrough LC Model http://www.ihi.org Components of Our LC • Learning Sessions Training Manuals Apply Skills Test Changes • Action Periods • Collaborative Meetings Ongoing TA & Support Share Progress • Measure Outcomes Learning Collaborative Process Create Change Package Implement Action Periods Develop Charter Hold Learning Sessions Select Teams Begin PreWork Measure Progress The Charter • Mission – Primary focus of the collaborative • Aims – Written statements of expected accomplishments • Expectations – Commitments to meet during LC • Community Care • Provider agencies • Other partners Aims • Process Aim 1: – By March 31, 2016, 100% of adults, age 18 years and older, are screened for depression using the PHQ-2 within the previous 12 months • Process Aim 2: – By March 31, 2016, 50% of individuals with a PHQ-9 score >10 are seen by the behavioral health clinician • Outcome Aim 1: – By March 31, 2016, 50% of individuals with a PHQ-9 score >10 have a 50% improvement in score after 3 months of treatment Select the Teams • Quality Improvement Teams (QIT) – Executive leadership – Clinical/quality improvement – Leadership – Lead behavioral health provider – Health center patient – Psychiatrist • Intervention faculty – Content experts • Support and TA teams (Community Care staff) Milestones PDSA Cycles: Plan-Do-Study-Act • PDSA cycles are how aims are achieved • Small tests of change • Conduct one or more each month • Measure impact • Submit workbook to producer • Share progress in monthly collaborative calls PDSA Cycle August BEGIN DATE: 8/3/15 DATE COMPLETED: Milestone/Fidelity: Improve overall behavioral health of BCHC patients PLAN What is your objective? Engage in a pro-active stance by earlier identifying patients with moderate depression rather than moderately severe or severe depression. What question(s) do you want to answer on this PDSA cycle? By using PHQ 9 screening tools are we able to identify patients with moderate depression earlier thereby have better outcome aims with 50% improvement? Number of patient referrals to BHC may increase/decrease, decrease need for What do you predict will happen? traditional outpatient mental health services, greater focus on relationship between physical and mental health conditions which may improve patient general wellbeing. What is your specific plan? PHQ 9 will be given by PSRs to patients during registration process. MA will collect and document PHQ 9 in EMR,if PHQ-9 is >10, patient will be informed of BHC onsite. In addition, PCP will review PHQ 9 score and discuss with patients the recommendation to see BHC onsite. Follow up with warm off hand to BHC onsite. DO Did you carry out your plan? □ Yes Summarize what happened. STUDY What did you find out? Compare your observation/data to your predictions and summarize what you learned. ACT What is your next logical step? Move on and develop a new PDSA cycle based on what you learned in this one. □ No Measure Progress on Aims • Update monthly Excel workbooks – Pre-formatted – Automatically graphs progress – Submitted monthly to producer – Reviewed by facilitator – Shared with collaborative • Synthesized in quarterly reports • Summative final report Process Aim 1 By March 31, 2016, 100% of adults, age 18 years and older, are screened for depression using the PHQ-2 within the previous 12 months Process Aim 2 By March 31, 2016, 100% of patients with a PHQ-9 score >10 are seen by the behavioral health provider Outcome Aim By March 31, 2016, 50% of patients with a PHQ-9 score >10 have a 50% improvement in score within 3 months Monthly Progress Assessment Questions Contact Suzanne Daub, LCSW Senior Director, Integrated Care Initiatives, Community Care daubs@ccbh.com Amy Lambert Director, Behavioral Health, La Comunidad Hispana alambert@lchps.org Helen Wooten, LCSW Behavioral Health Consultant, Berks Community Health Center hwooten@berkschc.org