Documentation and the MSE
advertisement

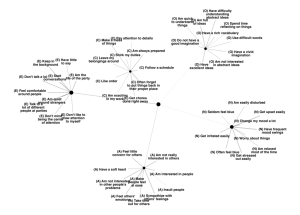
Documentation & the MSE 1 CNE point Good documentation – good defence Poor documentation – poor defence No documentation – no defence Objectives - Documentation Participants will: • have a greater appreciation / understanding of the need of accurate documentation in the mental health setting • be able to demonstrate use of the documentation framework presented • have a great awareness of professional accountability and documentation Objectives - MSE • to visit/revisit the essential components of an MSE • to consolidate current knowledge of conducting and interpreting an MSE • to practice conducting and writing up an MSE Increased awareness and curiosity • about the language used • messages, interpretations and meanings provoked and transferred in the documentation Problem based and solution focused Documentation Reflects the professionalism, competence, respect for patients and their families and the degree of competence with the policies and procedures of the workplace (Navuluri, 2001) The quality of documentation can determine whether a malpractice attorney accepts or declines a suicide case (Simpson & Stacy, 2004) Benefits to the client • Ensures the client is consulted and included in their care planning and that their decisions are recorded • Supports continuity of care – allows professionals involved in care to safely take over the clients ongoing care • Gives useful historical information for future care • Provide a legal document of the care they received (QNC, 2005) Benefits to the health professional • Gives clear and dependable instructions • Highlights unique contribution to care • Increases professional credibility by recording clinical judgement, delegation decisions and critical thinking • Involves a structured reflective reasoning process (identifying an emerging pattern) • Saves time – less energy spent searching for information/instructions • Provides reliable, accurate and complete information for safe and effective care & treatment (QNC, 2005) Benefits to organisation • Provides complete & reliable data to justify financial expenditure and resource allocation such as staffing levels and equipment • Facilitates research, auditing and quality improvement processes (QNC, 2005) F.A.C.T.U.A.L. Focused on the client Accurate Complete Timely Understandable Always objective Legible (QNC, 2005) Patient settled ATOR Patient more settled today, less intrusive. S/B S.W. today. Spending time in courtyard. Plans to go to local shops today Patient given 1:1 time. Pt struggling and reports low mood. Pt reactive throughout 1:1. Pt continues to use CBT techniques from last admission and is able to stop irrational thoughts. Encouraged patient to seek support. Reported increase in suicidal thoughts (no intent) early in the shift but these subsided following prn diazepam. Superficial conversation with staff only M S E ..is • Used as a screening tool to assess an individuals current neurological & psychological status • A means to transfer knowledge and clinical practice • A guide to individuals presentation and progress • Involves observations as well as an interview • Assess safety Important part of treatment planning MSE • Appearance & Behaviour • Speech • Mood & Affect • Thought content / processes • Perception • Insight & Judgement • Sensorium & cognition • Safety Appearance & Behaviour • Describe the individuals physical appearance (grooming, hygiene, clothing, nails, build, tattoos, piercing) • Individuals reaction to your interaction/ being admitted / present situation (hostile, friendly, grandiose, withdrawn, uncommunicative, seductive) • Motor behaviour (psychomotor retardation, restless, repetitive behaviours, hyperactive, tremor, hand wringing bizarre, agitated, anxious) Speech Rate (slow, accelerated, normal) Volume (loud, soft, whispered) Quantity of information Mutism (absence of speech) Poverty of speech (responses brief & monosyllabic) Pressure of speech (rapid, difficult to interrupt, loud and hard to understanding) Mood Defined in the Diagnostic and Statistical Manual of Mental Disorders IV (DSM IV) “is a pervasive and sustained emotion that colours the perception of the world. Variations in mood occur as a normal response to specific life experiences. Those responses are transient and are not associated with significant functional impairment such as depression elation, anger, and, anxiety”. • With a mood disorder: “the individual has persistent or recurrent disturbances or alterations in mood that continually cause psychological stress and behavioural impairment over the year” (Boyd & Nihart 1998:439). • Internal feeling or emotion – often influences behaviour Depressed, labile, euphoric, fearful, hostile, anxious, dysphoric, euthymic What about…… exhausted, confused, ecstatic, guilty, confident shy, bored, surprised, overwhelmed, embarrassed, thoughtful, relived, impressed, determined Affect - the observable expression of emotion - striated muscles controlling face, posture, vocalization (Nathanson, 1992) Reactive (normal) Restricted (decreased intensity & range) Blunted (severe decease in intensity & range of emotional expression) Flat (almost complete or complete absence of emotional expression - usually accompanied with monotonous voice) What about ….. Interest, excitement, enjoyment Surprised, startled Shame, humiliation Dissmell, disgust Fear, terror Distress, anguish Anger, rage (Nathanson, 1992;Tomkins, 1963) Thought content Amount of thought and rate of production – Poverty of ideas – Flight of ideas – Slow/hesitant thinking – Vague Continuity of ideas – Logical order – Tangential Disturbance in language – New words – Conversations that do not make sense Thought processes Thought blocking Neologism Fragmentation Perseveration Flight of ideas Word Salad Confabulation Circumstantiality Loose associations Tangentiality Thought Content Delusions – Fixed beliefs (grandiosity, jealousy, fantastic, nihilistic, religious) Suicidal thoughts – Transient, intrusive, persistent – Plan Other – Obsessions, antisocial urges, hypochondriacal • • • • • • • • • Delusions of persecution Delusional mood Delusions of reference Delusions of control, influence or passivity Religious delusion Nihilistic beliefs Fantastic delusions Delusions of jealousy Grandiose delusions Perception Hallucinations auditory visual olfactory gustatory tactile somatic Derealisation Depersonalisation Heightened perception Dulled perception Insight & Judgement Judgement During the course of an assessment many aspects of the individuals capacity for social judgment may be obvious. The clinician has to make an assessment on whether or not the individual has the ability and capacity to self assess what is happening around them and to make important discussions in their own best interests. Insight Refers to the DEGREE of awareness and understanding that the person has that she/he is ill. May be total denial. Some awareness but still denying. Awareness of illness but blaming on others. Acknowledge the illness but ascribe it to some unknown illness or event. Sensorium & cognition Attention and concentration • Provides an assessment on whether the person is alert and able to follow the interview or whether they are easily distracted by other things happening around them. Poor concentration • May be due to inefficiency of thinking, distractability, anxiety, delusions etc. (Assessment tool named Serial 7’s can be used to assess concentration – ask person to subtract from 100 by 7’s - how far can they go). Orientation • To time, place and person • True disturbances in orientation are found only in organic mental disorders. Memory - loss of: • Immediate (recall and retention) (give your name, date 10 mins later can the person recall) • Recent (what did they have for breakfast? what did they do yesterday?) • Remote (ask questions about persons childhood, important events in their life) General knowledge How is the person at counting, telling the time, naming the prime minister, what is the latest news Abstract thinking Generally assessed by asking the person to interpret proverbs (i.e. a rolling stone gathers no moss). However this can be difficult to assess based on persons intelligence, culture, language, beliefs. The presentation of changes to one or more of those process (attention, concentration, thinking etc) may be caused by a number of factors such as physical complications: (tumour, infection, or pain); influence of drugs (prescribed and non prescribed, or alcohol), post effects of poisoning deliberate or non deliberate: Safety Suicidal, homicidal, self harm and impulsive thinking – behaviour are important in the area of MSE Consider also safety in terms of vulnerability (sexual activity – consumer/consumer, consumer/staff member, consumer/external other) Other safety considerations include: AWOL physical risks, child safety MSE (or CP) Presenting a picture of the patients presentation to the reader A Attending to ADL’s. Casual attire Socialising with peers, engaging with staff, good eye contact, participating in groups today (self esteem) S Normal rate and flow M describes mood as “low”, rates on scale of 1-10 as 3 states that her mood “gets better as day progresses” and last night scored her mood as 6 Reactive affect in conversation T States that she has been “experiencing thoughts of self harm especially in the mornings”. States does not want to “self harm whilst in hospital” “want to try the new strategies that I have been learning” No obvious thought disturbances voiced or observed during interaction P No obvious perceptual disturbance observed or voiced during interaction I During interaction patient demonstrated insight about her admission and about her self harm thoughts. Pt. has the capacity to self assess as demonstrated in behaviour not to follow through with self harm thoughts S Patient alert, short and long term memory intact, able to engage in a conversation for 30 mins S Patient has stated that she has felt safe this morning and has not experienced any suicidal or self harm thoughts to time of report Interventions Tell the reader what you did • Staff time – 30 mins • Discussed with patient the issues they were concerned about (family, work) • Encouraged patient to identify strategies to manage concerns (journaling, discuss concerns with partner) • Developed with patient hierarchy of self harm reduction strategies (same attached to front of chart) • Accompanied patient on walk round hospital grounds observed interest patient expressed in physical surroundings • Patient offered PRN medication Outcomes Inform the reader about the effectiveness of the interventions that you used • Patient’s safety maintained throughout shift • Patient’s level of distress increased following discussion and patient has verbally stated that they are not suicidal and will approach staff if they are feeling unsafe and wish staff time and or prn medication, • Patient maintained on 30/60 visual obs • Dr Blogg’s informed re patients progress/status In summary • Be guided by policies of organisation • Be aware of the value of your documentation • Be thoughtful of what you write and how you write it • Be aware that patients can access their notes – include them in your readership • Initially takes time to use the framework – easier with practice Preparing for discharge … What is the individuals wishes ……? References • • • • • • • Elder, R., Evans, D, & Nizette, D. (2004). Psychiatric and Mental Health Nursing. Elsevier Australia: Marrickville. Navuluri, R. (2001). Documentation: What, why, where, who and how? Research for Nursing Practice, 3(1). Retrieved 10 August 2006 from http://www.ateresearch.com/Navu-Docu.htm Nathanson, D.L. (1992). Shame and pride. Affect, sex, and the birth of the self. New York: W.W. Norton & Company. Queensland Nursing Council. (2005). Professional documentation standards. Framework Information Sheet No 3. Simpson, S., & Stacy, M. (2004). Avoiding the malpractice snare: Documenting suicide risk assessment. Journal of Psychiatric Practice, 10, 185-189. Tomkins, S. (1963). Affect, imagery, consciousness. Vol 2. The negative affects. New York: Springer. Sanders, M. R., Mitchell, C., & Byrne, G. J. A. (Eds.) Medical Consultation Skills. Behavioural and Interpersonal Dimensions of Health Care. AddisonWesley: South Melbourne.