Case report
advertisement

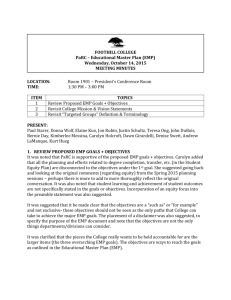
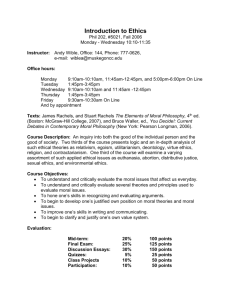
Shih LC, Chen JJ, Tsou YA, Tseng GC, Tsai MH, Chang HF, Huang KW, Chen DL, Chen CM. Multiple extramedullary plasmacytoma involving the vallecula: A case report with 3-year follow-up. Head Neck Oncol 2014 May 03;6(1):6. Section: Assessment of Head & Neck Tumours Category: Case Report Title: Multiple extramedullary plasmacytoma involving the vallecula: A case report with 3-year follow-up Liang-Chun Shih 1, Jiann-Jy Chen 2, Yung-An Tsou 1*, Guan-Chin Tseng 3, Ming-Hsui Tsai 1, Hsin-Feng Chang 4, Kuo-Wei Huang 5, Dem-Lion Chen 6, and Chuan-Mu Chen 7 Author details 1 Departments of Otolaryngology, 2 Neurology, and 3 Pathology, China Medical University Hospital, China Medical University, Taiwan 4 Faculty of Chinese Medicine and 5 Faculty of Medicine, Medical College, China Medical University, Taichung, Taiwan 6 G-Home Otorhinolaryngologic Clinic, Kaohsiung, Taiwan 7 Department of Life Sciences, National Chung-Hsing University, Taichung, Taiwan *Correspondence to: Dr Yung-An Tsou Department of Otolaryngology, China Medical University Hospital, #2, Yude Road, North District, Taichung City 40447, Taiwan E-mail: d22052121@yahoo.com.tw Abstract Introduction Extramedullary plasmacytoma (EMP) is a rare, malignant plasma-cell tumour that accounts for more than 0.04% of all head and neck malignancies. Multifocal EMPs involving at least two sites in the upper airway are extremely rare; to date, only 3 cases have been reported in the related English-language literature. AIM Case report A 63-year-old woman presented with a husky voice and globus pharyngis for two years. Physical examination revealed two sessile laryngeal polypoid lesions and a smooth, bulging mass at the right vallecula. After excision, a left epiglottic cyst, right false vocal-fold EMP, and right vallecular EMP were confirmed. The patient was diagnosed with stage I EMP (Durie-Salmon myeloma staging) after a battery of blood, urine, bone marrow, skeletal imaging, head and neck computed tomography, and bone scan studies. The patient refused any post-excisional radiotherapy; however, no recurrence of the EMP or progression to multiple myeloma was detected over the subsequent 3 years. Discussion It is difficult to associate multifocal polyps or nodules in the upper airway with EMPs because EMPs have no specific macroscopic appearance or symptom profile. The present case of multifocal EMPs at the larynx and oropharynx is novel, and this is the first case report on vallecular EMP in the related English-language literature. Moreover, this is the first case of multiple EMP that did not progress to multiple myeloma within a 3-year follow-up without adjuvant radiotherapy. Therefore, this case calls into question the need for adjuvant radiotherapy in cases of EMPs if complete excision with negative margins has been performed. However, the patient described herein was still at risk of developing multiple myeloma later in life, hence requiring lifelong follow-up. Conclusion Introduction Extramedullary plasmacytoma (EMP) is a rare, malignant plasma-cell tumour. Characteristically, EMP is a localised disease observed in soft tissues exterior to the bone marrow and is associated with a favourable prognosis1. This condition predominantly occurs in men, with a male-to-female ratio of 3:1 and a median age at presentation of 55 years2,3. EMP shows a predilection towards the head and neck region, with 92% of cases occurring in the upper aerodigestive tract4. Although 10% of EMPs are multiple5, multifocal EMPs occurring at two or more sites in the upper airway are extremely rare; to date, only 3 cases have been reported in the related English-language literature (see Table 1): one at the larynx and oropharynx6 and the other two at the larynx and nasopharynx7,8. Herein, we report a new case of multifocal EMPs at the larynx and oropharynx. To the best of our knowledge, vallecular EMP has never been previously reported in the related English-language literature. TABLE1 Case report A 63-year-old woman presented without any history of cigarette smoking, alcohol drinking, or areca consumption, and she did not have any systemic disease. She had suffered from a husky voice and globus pharyngis for two years. During the symptomatic period, she was treated for chronic laryngitis and took oral medication from a private clinic. However, her vocal strain and globus pharyngis became more severe. Furthermore, occasional dyspnoea and dysphagia occurred. Eventually, she was forced to visit our clinic at a local medical centre. Physical examination revealed two sessile laryngeal polypoid lesions: one connected to the right laryngeal ventricle (Figure 1A, arrow 1) and covering the anterior glottis and the other growing from the laryngeal surface of the epiglottis (Figure 1A, arrow 2). In addition, there was a smooth, bulging mass on the right vallecula (Figure 1A, arrow 3). The ears, nasal cavity, oral cavity, nasopharynx, and neck were unremarkable. Therefore, due to the multiple tumours found on the larynx and oropharynx, surgical excision was scheduled for histopathologic confirmation. Under endotracheal general anaesthesia, the two laryngeal polypoid lesions were excised using a direct Dedo laryngoscope. Subsequently, the right vallecular bulging mass was excised en bloc with a transoral CO2 laser. The patient tolerated the procedures well, and there was little bleeding. One week later, she was able to phonate well, and the surgical wounds on the larynx and tongue base had healed. Histopathological studies of the right false vocal-fold and right vallecular lesions revealed that the diffuse subepithelial plasmacytoid cell infiltration contained mature Marschalko-type plasma cells that were indistinguishable from normal plasma cells (Figure 1B). Immunohistochemically, these cells were positive for CD138 (Figure 1C) and negative for CD3 and CD20 with γ-light chain restriction. Low-grade plasmacytoma (Bartl histological grading) was then identified9. The histopathological study of the left epiglottic laryngeal lesion revealed a cyst lined with squamous epithelium. FIGURE1 Next, the patient underwent a battery of studies. A standard blood exam and her renal and liver function, electrolyte levels, and lipid profiles were within the normal ranges. Furthermore, quantitative serum immunoglobulin levels were within the normal limits, and urine protein electrophoresis was negative for Bence-Jones protein. Bone marrow biopsy cytology was normal. Head and neck contrast computed tomography did not reveal any lymphadenopathy. Skeletal bone and chest Roentgen examinations, a whole-body positron emission tomography scan, and a Tc-99m bone scan did not reveal any remarkable findings. Eventually, the patient was diagnosed with stage I EMP (Durie-Salmon myeloma staging)10. However, the patient was not comfortable receiving radiotherapy or other additional therapies because she no longer had any symptoms. For the past three years, she has been symptom free, and all follow-up physical examinations of her upper airway have been unremarkable. At present, there is no evidence of the disease progressing to multiple myeloma; however, follow-up is on-going. Discussion Our patient’s lesions were suspected of being attributable to granulomas, papillomas, or polyps, and the vallecular lesion was attributable to cystic or lymphoid tissue. However, granulomas, papillomas, and polyps are mass lesions of the true cord, rather than of the false cord or valleculae. Granulomas are usually located in the posterior commissure, rather than in the anterior larynx or valleculae; thus, granulomas could be excluded from the diagnosis of this case. Additionally, papillomas have characteristic punctate haemorrhaging that was also not present in this case. Therefore, the presence of mass lesions in the larynx warranted endoscopic excision for histopathological confirmation. According to Susnerwala et al.4, the median age of individuals suffering from EMPs of the head and neck is 68 years, and there is a strong male preponderance (M/F=23:2). All of the studied lesions were solitary, and 44% were located in the nasal cavities and sinuses, 20% were in the nasopharynx, 16% were in the oropharynx, 8% were in the larynx, and 2% were in the oral cavity. Furthermore, 80% were low-grade, 16% were intermediate-grade, and 4% were high-grade lesions (Bartl multiple-myeloma histological grading)9. However, EMPs comprise less than 4% of plasma-cell tumours of the head and neck, which represent less than 1% of head and neck malignancies11,12, indicating that EMPs comprise less than 0.04% of all head and neck malignancies. Laryngeal involvement was noted in the present case and in previous case reports describing EMPs at two or more sites in the upper airway. This laryngeal involvement was equally synchronous with oropharyngeal or nasopharyngeal involvement (see Table 1)6,7,8. In the present case, the laryngeal EMP, located at the right laryngeal ventricle, impaired right vocal-fold mobility, which led to hoarseness and obstructed the glottis. This blockage of the glottic airway contributed to occasional dyspnoea. The vallecular EMP contributed to the globus pharyngis and occasional dysphagia in the present case. In fact, it is difficult to associate multifocal polyps or nodules in the upper airway with EMPs because EMPs have no specific macroscopic appearance or symptom profile. EMP is typically confirmed by histopathology coupled with immunohistochemistry. Histopathology reveals the dense and homogeneous infiltration of plasma cells4. Therefore, the possibility of multiple myeloma should be excluded with quantitative serum immunoglobulin electrophoresis, urine protein electrophoresis, a skeletal bone survey, and a bone marrow biopsy. EMP is confirmed only if (1) bone marrow plasma-cell infiltration does not exceed 5% of all nucleated cells, (2) there is no osteolytic bone lesion or other tissue involvement, (3) there is no hypercalcaemia or renal failure, and (4) there is a low serum M protein concentration13, as in our patient. Furthermore, head and neck contrast computed tomography can help to differentiate normal lymphoid tissue or lymph nodes from occult EMP or lymph node involvement. Our patient did not have another focus of EMP or lymph node involvement, and she was later diagnosed with stage I EMP (Durie-Salmon myeloma staging)10. The primary treatment for EMPs of the head and neck region is excision followed by radiotherapy with a dose of 25-50 Gy over a period of 1.5-3 weeks. However, even patients given adjuvant radiotherapy are still at risk of developing multiple myeloma later in life and hence need lifelong follow-up. The initial control rate is better in patients with low-grade EMPs (83%) than in those with intermediate- or high-grade EMPs (17%). The rate of local or lymph nodular relapse is lower in patients with low-grade EMPs (20%) than in those with intermediate- or high-grade EMPs (80%). Radiotherapy or chemotherapy is recommended for those with local or lymph node relapse, whereas chemotherapy is recommended for those with high-grade EMPs or multiple myelomas (8%). The median survival is 5.7 years, and the 5-year overall survival rate is 58.9%4. Post-excisional radiotherapy was recommended in all of the previous case reports describing EMPs at two or more sites in the upper airway (see Table 1) or with surgical margin involvement; however, Bachar et al.14 did not recommend adjuvant radiotherapy for patients who had undergone complete excision with negative margins. Our patient refused any post-excisional radiotherapy, and surprisingly, no recurrence of EMP or progression to multiple myeloma was detected during three years of follow-up. Therefore, this case calls into question the need for adjuvant radiotherapy in patients with EMPs who have undergone complete excision with negative margins. However, regular follow-up, including not only local control but also systemic observation via blood counts and immunoglobulin measurements, is still warranted to prevent the possibility of local relapse, lymph node relapse, or progression to multiple myeloma. Conclusion Consent Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal. Authors’ contribution Liang-Chun Shih and Jiann-Jy Chen contributed equally to the study design and performed the literature research, manuscript preparation, and manuscript review. Guan-Chin Tseng conducted the histological examination and prepared the pathological figures. Yung-An Tsou and Ming-Hsui Tsa performed the surgery and supervised the related literature research. Dem-Lion Chen revised the article for important intellectual content. Hsin-Feng Chang and Kuo-Wei Huang drafted the manuscript and arranged all of the paragraphs and supporting figures in their proper order. All authors have read and approved the final version of the manuscript. References 1. Kayrouz T, Jose B, Chu AM, Scott RM. Solitary plasmacytoma. J Surg Oncol. 1983, 24(1):46-48. 2. Shih LY, Dunn P, Leung WM, Chen WJ, Wang PN. Localised plasmacytomas in Taiwan: comparison between extramedullary plasmacytoma and solitary plasmacytoma of bone. Br J Cancer. 1995, 71(1):128-133. 3. Strojan P, Soba E, Lamovec J, Munda A. Extramedullary plasmacytoma: Clinical and histopathologic study. Int J Radiat Oncol Biol Phys. 2002, 53(3):692-701. 4. Susnerwala SS, Shanks JH, Banerjee SS, Scarffe JH, Farrington WT, Slevin NJ. Extramedullary plasmacytoma of the head and neck region: clinicopathological correlation in 25 cases. Br J Cancer. 1997, 75(6):921-927. 5. Waldron J, Mitchell DB. Unusual presentations of extramedullary plasmacytoma in the head and neck. J Laryngol Otol. 1988, 102:102-104. 6. Lewis K, Thomas R, Grace R, Moffat C, Manjaly G, Howlett DC. Extramedullary plasmacytomas of the larynx and parapharyngeal space: imaging and pathologic features. Ear Nose Throat J. 2007, 86(9):567-569. 7. Yavas O, Altundag K, Sungur A. Extramedullary plasmacytoma of nasopharynx and larynx: synchronous presentation. Am J Hematol. 2004, 75(4):264-265. 8. Iseri M, Ozturk M, Ulubil SA. Synchronous presentation of extramedullary plasmacytoma in the nasopharynx and the larynx. Ear Nose Throat J. 2009, 88(11):E9-E12. 9. Bartl R, Frisch B, Fateh-Moghadam A, Kettner G, Jaeger K, Sommerfeld W. Histologic classification and staging of multiple myeloma. A retrospective and prospective study of 674 cases. Am J Clin Pathol. 1987, 87(3):342-355. 10. Durie BG, Salmon SE. A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment, and survival. Cancer. 1975, 36(3):842-854. 11. Nofsinger YC, Mirza N, Rowan PT, Lanza D, Weinstein G. Head and neck manifestations of plasma cell neoplasms. Laryngoscope. 1997, 107(6):741-746. 12. Wax MK, Yun KJ, Omar RA. Extramedullary plasmacytomas of the head and neck. Otolaryngol Head Neck Surg. 1993, 109(5):877-885. 13. Bataille R, Sany J. Solitary myeloma: clinical and prognostic features of a review of 114 cases. Cancer. 1981, 48(3):845-851. 14. Bachar G, Goldstein D, Brown D, Tsang R, Lockwood G, Perez-Ordonez B, et al. Solitary extramedullary plasmacytoma of the head and neck - long-term outcome analysis of 68 cases. Head Neck. 2008, 30(8): 1012-1019. Table 1. Multiple extramedullary plasmacytoma (EMP) at two or more sites in the upper airway in the related English-language literature Figure legends A: Physical examination demonstrated a sessile polypoid lesion at the right laryngeal ventricle (arrow 1); a sessile polypoid lesion at the laryngeal surface of epiglottis (arrow 2); and a smooth, bulging mass at the right vallecula (arrow 3). B: Histopathologically, there was diffuse subepithelial plasmacytoid cell infiltration containing mature Marschalko-type plasma cells, which were indistinguishable from normal plasma cells (H&E stain, 400). C: Immunohistochemically, these cells were positive for CD138 (400 ). Table 1: Table 1.docx Table 1. Multiple extramedullary plasmacytoma (EMP) at two or more sites in the upper airway in the related English-language literature Case Age (years) Past history EMP sites Post-excisional therapy Outcome Author (follow-up time) (year of publication) Radiotherapy Uneventful (2 years) Lewis (2007) [6] Radiotherapy (40 Gy) Not mentioned Yavas (2004) [7] Larynx Radiotherapy (40 Gy) Uneventful (2 years) Iseri (2009) [8] Nasopharynx Chemotherapy Larynx No Uneventful (3 years) The present case /Gender 1 71/M Nil Larynx Parapharyngeal wall 2 43/F Nil Larynx Nasopharynx 3 4 46/F 63/F A cutaneous EMP Nil Vallecula Figure 1: Figure.tif