Organophosphorous poisoning mgmc
advertisement
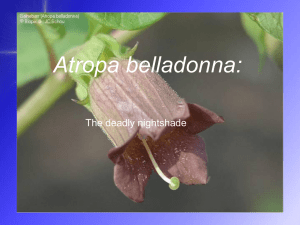
Organophosphorous poisoning Dr. S. Parthasarathy MD., DA., DNB, MD (Acu), Dip. Diab.DCA, Dip. Software statistics, Phd (physio) Mahatma Gandhi Medical college and research institute , puducherry , India Out of 5 lakh self inflicted deaths • Organophosphorus pesticide self-poisoning is a major clinical and public-health problem across much of rural Asia. • OPC – responsible for 2 lakh death a year in ASIA • Intentional only !! • Readily available …. Any body can buy !! • 75000 /year – India – estimation ?? Source ?? • Organophosphorus compounds are chemical agents in wide-spread use throughout the world, mainly in agriculture. • They are also used as nerve agents in chemical warfare (e.g. Sarin gas), • therapeutic agents, such as ecothiopate used in the treatment of glaucoma. Types Most organophosphates can be divided into two types: • diethyl (e.g. chlorpyrifos, diazinon, parathion, phorate and dichlofenthion) • dimethyl (e.g. dimethoate, dichlorvos, fenitrothion, malathion and fenthion). Another classification Classification Malathion Normal physiology • Acetylcholine (ACh) is the neurotransmitter released at all postganglionic parasympathetic nerve endings and at the synapses of both sympathetic and parasympathetic ganglia. It is also released at the skeletal muscle myoneural junction, and serves as a neurotransmitter in the central nervous system. • ACh is hydrolyzed by acetylcholinesterase into two fragments: acetic acid and choline. Acetylcholinesterase • Two forms • True acetylcholinesterase which is found primarily in the tissues and erythrocytes, • pseudocholinesterase which is found in the serum Mechanism of action Instead of 60 seconds – may take hours to weeks What is anaesthetic drug which works like this ?? Acetyl choline is pouring in all places – not getting metabolized • Usually ingestion, • inhalation and skin absorption also Clinical features Five important features • There are five important features assessed for cholinergic syndrome• Miosis--- local ?? • excessive sweating • bronchorrhea and bronchospasm • bradycardia and hypotension. • OP compounds can be absorbed through skin, conjunctiva, oral mucosa, GI tract, respiratory tract, by direct contact, ingestion, inhalation and injection • Lipid soluble --- CNS • Resecretion • Bronchorrhea is the usual mechanism of early morbidity and mortality in OPP. • The origin of this excess fluid is from the airway secretions and not exudation of fluid across the alveolar-capillary membrane. • The obstruction of upper and lower airways and the potential intrusion of these bronchial secretions into the alveolar sacs produces hypoxia that is the primary concern Cardiovascular • Phase I: A brief period of increased sympathetic tone • Phase II: A prolonged period of parasympathetic activity including AV node blockade • Phase III: Q-T prolongation followed by torsade de pointes, ventricular ventricular fibrillation. tachycardia and Respiration • Secretions may choke • Nicotinic effects – weakness • CNS depression Neurological • Type I paralysis or acute paralysis- cholinergic crisis • Type II paralysis or Intermediate syndrome • 24 – 48 hours later ,proximal , head lift ?? Respiration OK ?? Extraocular muscles, VII and X – 4 – 18 days persist • Type III paralysis or Organophosphate- induced delayed polyneuropathy • 4 weeks later, weakness of hand and feet , calf pain • Rarely seizures and coma Diagnosis • Clinical features ,History ,Suspicion Unconsciuos ?? • Smell ( vomitus ?? Breath, sweat) alcohol ?? • Cholinesterase levels – true and pseudo • Normal serum acetylcholinesterase level is 3,500 - 8,500 U/L • < 1700 , < 700 < 100 – should improve with treatment • electro diagnostic abnormalities, the 30 Hz rapid nerve stimulation decremental response correlates best with clinically detectable weakness and hence it is the most useful diagnostic test for IMS Red cell cholinesterase • These assays measure acetylcholinesterase expressed on the surface of red cells. • Red-cell acetylcholinesterase inhibition is a good marker of such inhibition in synapses and of poisoning severity. • Atropine ?? • P2 AM stoppage ?? GOALS OF TREATMENT • Reduce absorption of the toxin • Enhance elimination • Neutralize toxin. • ABC remains Reduce absorption of the toxin • • • • • • • • Removal from surface of skin, eyes and hair • Emesis induction • Gastric lavage • Activated charcoal administration and cathartics • Dilution—milk/other drinks for corrosives • Whole bowel irrigation • Endoscopic removal of ingested chemical • Skin decontamination—important aspect—not to be neglected: • – Remove contaminated clothing • – Wash with soap and water Wash, wash and wash • Skin folds and underside of fingernails and long hairs require particular attention. • Ocular decontamination is to be carried out by washing eyes with water/normal saline • Contaminated leather articles should be discarded as the leather absorbs the chemical and cannot effectively be cleaned - document in notes and explain necessity to the family. • Gastric lavage • Activated charcoal 25 g 2 hourly • Sorbitol as cathartic. Gastric lavage • Gastric lavage decreases absorption by 42% if done at • • • • • • • 20 minutes and by 16% if performed at 60 minutes Performed by first aspirating the stomach and then repetitively instilling and aspirating fluid Left lateral position delays spontaneous absorption No evidence that a larger tube is better Simplest, quickest and least expensive way—funnel Choice of fluid - tap water: 5–10 mL/kg (sodium ?) Preferably done on awake patients More will – vomit or push into the small bowel For our staff • Charcoal mask and impermeable gown are to be worn in the isolation room. • • When caring for the patient, rubber gloves are to be worn (as per chemotherapeutic precautions). • • In severe poisoning, industrial goggles for eye protection/comfort should be worn. • Rotate staff frequently • Hypochlorite solution on transfer Atropine • The recommended starting dose of atropine is 2 mg IV bolus. • Subsequent doses of 2-5mg every 5-15 minutes should be for adequate atropinization • increased heart rate (>100 beats/min.), moderately dilated pupils, • a reduction in bowel sounds, a dry mouth (axillae) and a decrease in bronchial secretions. • The drying of pulmonary secretions is the most important and most reliable endpoint and not tachycardia or mydriasis. • Double the dose in 15 minutes if no effect • Prefer atropine if oxygen is NA • Rate increase by more than 25 + flushing ?? • Table maintain To note • Genaral wheezing decreased ?? • Localised wheezing ?? Aspiration • Miosis ?? Indicator • Some use atropine to maintain consciousness!! How to continue • Shots of atropine every 5 minutes • Atropinised in one hour • Then every hour he/ she may need 10- 20 % of the dose received in the first hour as one hour infusion • Inbetween atropinisation lost– one more bolus and increase the infusion rate by 10 % Atropine • Continuous atropine infusions are used in some centres in doses of 0.02-0.08mg/kg/hr. • Day 1 maximum • Usually weaned off in around 7 days • Nebulised atropine may improve respiratory distress and oxygenation by decreasing bronchial secretions • Hyoscine was used successfully to treat a patient with severe extra-pyramidal features Glycopyrrolate- (Dose-0.05mg/kg) • The main advantages of glycopyrrolate over atropine are – • nil central toxicity (central antichoilinergic syndrome) as it is a quaternary ammonium compound and hence has penetration, no CNS NO DELIRIUM • lesser tachycardia, better control of tracheobronchial secretions lower incidence of respiratory tract infection. • Atropine glyco combinations • First day – atropine High atropine • Excess atropine causes agitation, confusion, urinary retention, hyperthermia, bowel ileus and tachycardia • Stop , watch for 30 minutes – restart at 70 % dose • Catheterize for agitation Oximes To quote a few • obidoxime, diacetyl monoxime, bisaldoxime, • pralidoxime (2-PAM or P2AM –2hydroxy iminomethyl-1-methyl pyridinium chloride) is most often used, world wide • Reversal of Nicotinic effects How do oximes act ?? • These agents reactivate acetyl cholinesterase by removing the phosphoryl group P2AM Now acetyl cholinesterse is ready to destroy acetyl choline P2AM • The WHO recommendation is a loading dose of 30mg/kg followed by an infusion of >8mg/kg/hr. • The therapeutic endpoint for P2AM therapy is the resolution of muscle fasciculations and weakness, reactivation and permanent clinical improvement and incremental SChE levels • Nicotinic • Usually anticholinergics a few days later – stop P2AM • Serum levels of P2AM >4mg/lit is necessary for effectively treating OP toxicity • Less IMS • Lipid solubility low – CNS penetration is less • diethyl compounds (OPCs) reactivate and “age” at a significantly slower rate than dimethyl compounds. More effective in diethyl poisons WHO tells what?? • WHO recommends that oximes be given to all symptomatic patients who need atropine • Effectiveness after 2 hours ?? • The loading dose of oxime should not be given rapidly as a bolus because this method causes vomiting (risking aspiration), diastolic hypertension. tachycardia, and Other options • HupA has been proven to be a powerful, highly specific, and reversible inhibitor of Acetyl cholinesterase • Butane - 2, 3-dionethiosemicarbazone is an oxime with antioxidant properties • detoxification routes of OPs (both insecticides and nerve agents) is hydrolysis ‘phosphotriesterases’ (PTEs). by esterases called Other options • The alpha2-adrenergic receptor agonist clonidine also reduces acetylcholine synthesis • Soda bicarb to increase pH • toxic molecules can be counteracted by antioxidants such as vitamins C and E, melatonin • Circulation –Give 500–1000 ml (10–20 ml/kg) of normal saline over 10–20 min and assess • cautious use of noradrenaline • Fits – atropine and benzodiazepines Other options • Benzodiazepines • No opioids • No deriphyllin • No scoline • Mechanical ventilation • FFP • • • • Organo carbamates Reversible Atropine ‘’Ok but no oximes • Organochlorides Organochlorides • endosulfan, chlordane, aldrin, dieldrin, endrin, • isoflurane.?? • Pesticides • Decontamination and supportive therapy • No atropine and no pralidoxime Summary • • • • • • • OPC Clinical features Mechanism Treatment Atropine P2AM Newer things Thank you all