Seibel_Soper_SFE_Barcelona_July-05
advertisement
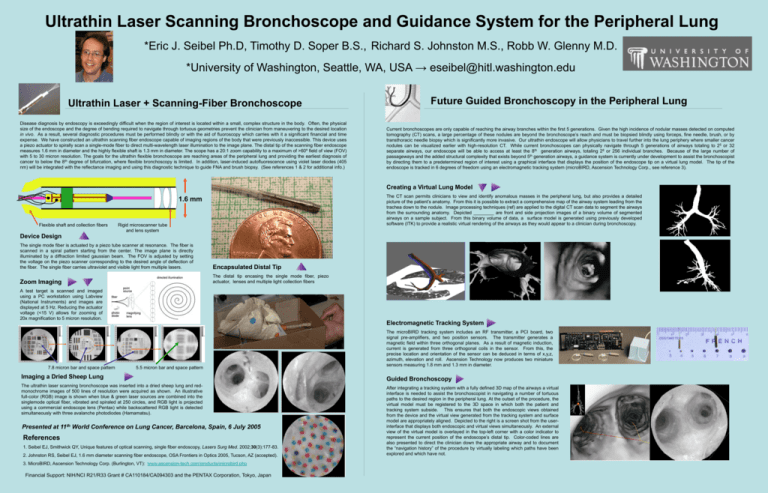
Ultrathin Laser Scanning Bronchoscope and Guidance System for the Peripheral Lung *Eric J. Seibel Ph.D, Timothy D. Soper B.S., Richard S. Johnston M.S., Robb W. Glenny M.D. *University of Washington, Seattle, WA, USA → eseibel@hitl.washington.edu Ultrathin Laser + Scanning-Fiber Bronchoscope Disease diagnosis by endoscopy is exceedingly difficult when the region of interest is located within a small, complex structure in the body. Often, the physical size of the endoscope and the degree of bending required to navigate through tortuous geometries prevent the clinician from maneuvering to the desired location in vivo. As a result, several diagnostic procedures must be performed blindly or with the aid of fluoroscopy which carries with it a significant financial and time expense. We have constructed an ultrathin scanning fiber endoscope capable of imaging regions of the body that were previously inaccessible. This device uses a piezo actuator to spirally scan a single-mode fiber to direct multi-wavelength laser illumination to the image plane. The distal tip of the scanning fiber endoscope measures 1.6 mm in diameter and the highly flexible shaft is 1.3 mm in diameter. The scope has a 20:1 zoom capability to a maximum of >60º field of view (FOV) with 5 to 30 micron resolution. The goals for the ultrathin flexible bronchoscope are reaching areas of the peripheral lung and providing the earliest diagnosis of cancer to below the 8th degree of bifurcation, where flexible bronchoscopy is limited. In addition, laser-induced autofluorescence using violet laser diodes (405 nm) will be integrated with the reflectance imaging and using this diagnostic technique to guide FNA and brush biopsy. (See references 1 & 2 for additional info.) Future Guided Bronchoscopy in the Peripheral Lung Current bronchoscopes are only capable of reaching the airway branches within the first 5 generations. Given the high incidence of nodular masses detected on computed tomography (CT) scans, a large percentage of these nodules are beyond the bronchoscope’s reach and must be biopsied blindly using forceps, fine needle, brush, or by transthoracic needle biopsy which is significantly more invasive. Our ultrathin endoscope will allow physicians to travel further into the lung periphery where smaller cancer nodules can be visualized earlier with high-resolution CT. While current bronchoscopes can physically navigate through 5 generations of airways totaling to 25 or 32 separate airways, our endoscope will be able to access at least the 8th generation airways, totaling 28 or 256 individual branches. Because of the large number of passageways and the added structural complexity that exists beyond 5th generation airways, a guidance system is currently under development to assist the bronchoscopist by directing them to a predetermined region of interest using a graphical interface that displays the position of the endoscope tip on a virtual lung model. The tip of the endoscope is tracked in 6 degrees of freedom using an electromagnetic tracking system (microBIRD, Ascension Technology Corp., see reference 3). Creating a Virtual Lung Model The CT scan permits clinicians to view and identify anomalous masses in the peripheral lung, but also provides a detailed picture of the patient’s anatomy. From this it is possible to extract a comprehensive map of the airway system leading from the trachea down to the nodule. Image processing techniques (ref) are applied to the digital CT scan data to segment the airways from the surrounding anatomy. Depicted ________ are front and side projection images of a binary volume of segmented airways on a sample subject. From this binary volume of data, a surface model is generated using previously developed software (ITK) to provide a realistic virtual rendering of the airways as they would appear to a clinician during bronchoscopy. 1.6 mm Flexible shaft and collection fibers Rigid microscanner tube and lens system Device Design The single mode fiber is actuated by a piezo tube scanner at resonance. The fiber is scanned in a spiral pattern starting from the center. The image plane is directly illuminated by a diffraction limited gaussian beam. The FOV is adjusted by setting the voltage on the piezo scanner corresponding to the desired angle of deflection of the fiber. The single fiber carries ultraviolet and visible light from multiple lasers. Encapsulated Distal Tip Zoom Imaging The distal tip encasing the single mode fiber, piezo actuator, lenses and multiple light collection fibers A test target is scanned and imaged using a PC workstation using Labview (National Instruments) and images are displayed at 5 Hz. Reducing the actuator voltage (<15 V) allows for zooming of 20x magnification to 5 micron resolution. 7.8 micron bar and space pattern Electromagnetic Tracking System 5.5 micron bar and space pattern The microBIRD tracking system includes an RF transmitter, a PCI board, two signal pre-amplifiers, and two position sensors. The transmitter generates a magnetic field within three orthogonal planes. As a result of magnetic induction, current is generated from three orthogonal coils in the sensor. From this, the precise location and orientation of the sensor can be deduced in terms of x,y,z, azimuth, elevation and roll. Ascension Technology now produces two miniature sensors measuring 1.8 mm and 1.3 mm in diameter. Imaging a Dried Sheep Lung Guided Bronchoscopy The ultrathin laser scanning bronchoscope was inserted into a dried sheep lung and redmonochrome images of 500 lines of resolution were acquired as shown. An illustrative full-color (RGB) image is shown when blue & green laser sources are combined into the singlemode optical fiber, vibrated and spiraled at 250 circles, and RGB light is projected using a commercial endoscope lens (Pentax) while backscattered RGB light is detected simultaneously with three avalanche photodiodes (Hamamatsu). After integrating a tracking system with a fully defined 3D map of the airways a virtual interface is needed to assist the bronchoscopist in navigating a number of tortuous paths to the desired region in the peripheral lung. At the outset of the procedure, the virtual model must be registered to the 3D space in which both the patient and tracking system subside. This ensures that both the endoscopic views obtained from the device and the virtual view generated from the tracking system and surface model are appropriately aligned. Depicted to the right is a screen shot from the userinterface that displays both endoscopic and virtual views simultaneously. An external view of the virtual model is overlayed in the top-left corner with a color indicator to represent the current position of the endoscope’s distal tip. Color-coded lines are also presented to direct the clinician down the appropriate airway and to document the “navigation history” of the procedure by virtually labeling which paths have been explored and which have not. Presented at 11th World Conference on Lung Cancer, Barcelona, Spain, 6 July 2005 References 1. Seibel EJ, Smithwick QY, Unique features of optical scanning, single fiber endoscopy, Lasers Surg Med. 2002;30(3):177-83. 2. Johnston RS, Seibel EJ, 1.6 mm diameter scanning fiber endoscope, OSA Frontiers in Optics 2005, Tucson, AZ (accepted). 3. MicroBIRD, Ascension Technology Corp. (Burlington, VT): www.ascension-tech.com/products/microbird.php Financial Support: NIH/NCI R21/R33 Grant # CA110184/CA094303 and the PENTAX Corporation, Tokyo, Japan