P. falciparum - WordPress.com
advertisement
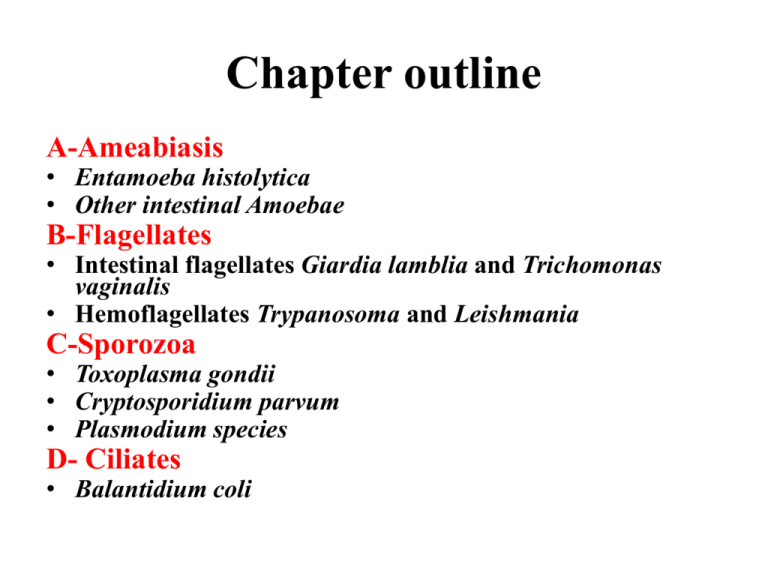
Chapter outline A-Ameabiasis • Entamoeba histolytica • Other intestinal Amoebae B-Flagellates • Intestinal flagellates Giardia lamblia and Trichomonas vaginalis • Hemoflagellates Trypanosoma and Leishmania C-Sporozoa • Toxoplasma gondii • Cryptosporidium parvum • Plasmodium species D- Ciliates • Balantidium coli Sporozoa These protozoa have no locomotory extensions of the body and all species are parasitic. Their motile stages move by bending, creeping and gliding and the Apicomplexa have an APICAL COMPLEX formed by micronemes, rhoptries, dense granules and microtubules at their anterior end playing a role in the invasion Coccidia constitute a very large group called Apicomplexa, some members of which are intestinal parasites and others are blood and tissue parasites. All coccidia demonstrate typical characteristics, especially the existence of asexual (schizogony) and sexual (gametogony) reproduction. Most members of the group also share alternative hosts; for example, in malaria, mosquitoes harbor the sexual cycle and humans the asexual cycle. Micronemes Rhoptries Dense Granules Cliché JF Dubremetz Micronemes: adhesion and motility Rhoptry neck proteins RONs+ MICs: Moving junction formation Rhoptry Bulb Content: Parasitophorous vacuole formation Dense Granules: Parasitophorous vacuole remodeling • Most sporozoans are intracellular parasites or at least part of their life-cycle takes place inside a host cell. • The Apicomplexa are a large group of protists, characterized by the presence of a unique organelle called an apical complex. Some diseases caused by apicomplexan organisms include: • Malaria (Plasmodium) • Coccidian diseases including: – Cryptosporidiosis (Cryptosporidium parvum) – Toxoplasmosis (Toxoplasma gondii) Sporozoa 1- TOXOPLASMA GONDII T. gondii is a typical coccidian parasite related to Plasmodium, Isospora, and other members of the phylum Apicomplexa. T. gondii is an intracellular parasite, and it is found in a wide variety of animals, including birds and humans. The essential reservoir host of T. gondii is the common house cat and other felines. Sporozoa 1- TOXOPLASMA GONDII Physiology and Structure Organisms develop in the intestinal cells of the cat, as well as during an extraintestinal cycle with passage to the tissues via the bloodstream. The organisms from the intestinal cycle are passed in cat feces and mature into infective cysts within 3 to 4 days in the external environment. Infection in cats is established when the tissues of infected rodents are eaten. Some infective forms, or trophozoites, from the oocyst develop as slender, crescentic types, called tachyzoites. These rapidly multiplying forms are responsible for the initial infection and the tissue damage. Slow-growing, shorter forms called bradyzoites also develop and form cysts in chronic infections. Life cycle of Toxoplasma gondii. bradyzoite Reactivation 20 µm 20 µm BRADYZOITES Slow multiplication Cyst formation TACHYZOITES Fast multiplication tachyzoite carnivorism Intermediate host sporozoite sporogony a schizogony b 10 µm OOCYSTES a- non sporulated b- sporulated merozoite zygote gamogony Final host Toxoplasma gondii Obligate Intracellular Parasite Responsible of toxoplasmosis Neurotoxoplasmosis Congenital Toxoplasmosis Chorioretinitis Immunocompromised individuals Cliché JF Dubremetz Sporozoa 1- TOXOPLASMA GONDII Epidemiology Human infection with T. gondii is ubiquitous; however, it is increasingly apparent that certain immunocompromised individuals (patients with acquired immune deficiency syndrome [AIDS]) are more likely to have severe manifestations. The wide variety of animals that harbor the organism-carnivores and herbivores, as well as birds-accounts for the widespread transmission. Humans become infected from two sources: (1) ingestion of improperly cooked meat from animals that serve as intermediate hosts and (2) the ingestion of infective oocysts from contaminated cat feces. Serologic studies show an increased prevalence in human populations where the consumption of uncooked meat or meat juices is popular. It is noteworthy that serologic tests of human and rodent populations are negative in the few geographic areas where cats have not existed. Outbreaks of toxoplasmosis in the United States are usually traced to poorly cooked meat (e.g., hamburgers) and contact with cat feces. Transplacental infection can occur in pregnancy, either from infection acquired from meat and meat juices or from contact with cat feces. Transfusion infection via contaminated blood can occur but is not common. Transplacental infection from an infected mother has a devastating effect on the fetus. Although the rate of seroconversion is similar for individuals within a geographic location, the rate of severe infection is dramatically affected by the immune status of the individual. Patients with defects in cell-mediated immunity, especially those who are infected with the human immunodeficiency virus (HIV) or who have had an organ transplant or immunosuppressive therapy, are most likely to have disseminated or central nervous system (CNS) disease. It is believed that illness in this setting is caused by reactivation of previously latent infection rather than new exposure to the organism. Sporozoa 1- TOXOPLASMA GONDII Clinical syndromes Most T. gondii infections are benign and asymptomatic, with symptoms occurring as the parasite moves from the blood to tissues, where it becomes an intracellular parasite. When symptomatic disease occurs, the infection is characterized by cell destruction, reproduction of more organisms, and eventual cyst formation. Many tissues may be affected; however, the organism has a particular predilection for cells of the lung, heart, lymphoid organs, and CNS, including the eye. Symptoms of acute disease include chills, fever, headaches, myalgia, lymphadenitis, and fatigue; the symptoms occasionally resemble those of infectious mononucleosis. In chronic disease the signs and symptoms include lymphadenitis, occasionally a rash, evidence of hepatitis, encephalomyelitis, and myocarditis. In some of the cases, chorioretinitis appears and may lead to blindness. Congenital infection with T. gondii also occurs in infants born to mothers infected during pregnancy. If infection occurs in the first trimester, the result is spontaneous abortion, stillbirth, or severe disease. Manifestations in the infant infected after the first trimester include epilepsy, encephalitis, microcephaly (abnormal smallness of the head), intracranial calcifications, hydrocephalus (Hydrocephalus is an abnormal expansion of cavities (ventricles) within the brain that is caused by the accumulation of cerebrospinal fluid), psychomotor or mental retardation, chorioretinitis, blindness, anemia, jaundice, rash, pneumonia, diarrhea, and hypothermia (Hypothermia, a potentially fatal condition, occurs when body temperature falls below 35°C). Infants may be asymptomatic at birth, only to develop disease months to years later. Most often these children develop chorioretinitis with or without blindness or other neurologic problems, including retardation, seizures, microcephaly, and hearing loss. A different spectrum of disease is seen in immunocompromised older patients. Reactivation of latent toxoplasmosis is a special problem for these people. The presenting symptoms of Toxoplasma infection in immunocompromised patients are usually neurologic, most frequently consistent with diffuse encephalopathy, meningoencephalitis, or cerebral mass lesions. Reactivation of cerebral toxoplasmosis has emerged as a major cause of encephalitis in patients with AIDS. Sporozoa 1- TOXOPLASMA GONDII Laboratory Diagnosis Serologic testing is required for the diagnosis of acute active infection; the diagnosis is established by the finding of increasing antibody titers documented in serially collected blood specimens. Because contact with the organism is common, attention to increasing titers is essential to differentiate acute, active infection from previous asymptomatic or chronic infection. Currently the enzyme-linked immunosorbent assay (ELISA) for detecting immunoglobulin (Ig) M antibodies appears to be the most reliable procedure because of its simplicity and rapidity in documenting acute infections. The test is not generally satisfactory in AIDS patients with latent or reactivated infections, because they fail to produce an IgM response or increasing IgG titer. Demonstration of these organisms as trophozoites and cysts in tissue and body fluids is the definitive method of diagnosis. Biopsy specimens from lymph nodes, brain, myocardium, or other suspected tissue, as well as body fluids, including cerebrospinal fluid, amniotic fluid, or bronchoalveolar lavage fluid, can be directly examined for the organisms. Newer monoclonal antibody-based fluorescent stains may facilitate direct detection of T. gondii in tissue. Culture methods for T. gondii are largely experimental and not usually available in clinical laboratories. Cyst of T. gondii in tissue. Hundreds of organisms may be present in the cyst, which may become active and initiate disease with decreased host immunity (e.g., immunosuppression in transplant patients and in diseases such as AIDS). The two methods available are to inoculate potentially infected material into either mouse peritoneum or tissue culture. Advances in developing polymerase chain reaction-based detection methods are promising and may provide rapid and sensitive approaches for detecting the organism in blood, cerebrospinal fluid, amniotic fluid, and other clinical specimens. Sporozoa 2- CRYPTOSORIDIUM SPECIES Physiology and Structure The life cycle of Cryptosporidium species is typical of coccidians, as is the intestinal disease, but this species differs in the intracellular location in the epithelial cells. Cryptosporidium organisms are found just within the brush border of the intestinal epithelium. The coccidia attach to the surface of the cells and replicate by a process that involves schizogony. 2- CRYPTOSORIDIUM SPECIES Epidemiology Cryptosporidium species are distributed worldwide. Infection is reported in a wide variety of animals, including mammals, reptiles, and fish. Waterborne transmission of cryptosporidiosis is well documented as an important route of infection. The massive outbreak of cryptosporidiosis in Milwaukee (approximately 300,000 individuals infected) was linked to contamination of the municipal water supply. Cryptosporidia are resistant to the usual water-purification procedures (chlorination and ozone), and it is believed that runoff of local waste and surface water into municipal water supplies is an important source of contamination. Zoonotic spread from animal reservoirs to humans, as well as personto-person spread by fecal-oral and oral-anal routes, is also common means of infection. Veterinary personnel, animal handlers, and homosexuals are at particularly high risk for infection. Many outbreaks have now been described in daycare centers where fecal-oral transmission is common. CLINICAL SYNDROMES As with other protozoan infections, exposure to Cryptosporidium organisms may result in asymptomatic carriage. Disease in previously healthy individuals is usually a mild, self-limiting enterocolitis characterized by watery diarrhea without blood. Spontaneous remission after an average of 10 days is characteristic. In contrast, disease in immunocompromised patients (e.g., patients with AIDS), characterized by 50 or more stools per day and tremendous fluid loss, can be severe and last for months to years. In some patients with AIDS, disseminated Cryptosporidium infections have been reported. LABORATORY DIAGNOSIS Cryptosporidium may be detected in large numbers in unconcentrated stool specimens obtained from immunocompromised individuals with diarrhea. Specimens may be stained using the modified acid-fast method or by an indirect immunofluorescence assay. The number of oocysts shed in stool may fluctuate; therefore a minimum of three specimens should be examined. Serologic procedures for diagnosing and monitoring infections are under investigation but are not yet widely available. Acid-fast stained (red) Cryptosporidium oocysts (approximately 5 to 7 μm in diameter). Sporozoa 3- PLASMODIUM SPECIES Plasmodia are coccidian or sporozoan parasites of blood cells, and as seen with other coccidia, they require two hosts: the mosquito for the sexual reproductive stages and humans and other animals for the asexual reproductive stages. Infection with Plasmodium spp. (i.e., malaria) accounts for 1 to 5 billion febrile episodes and 1 to 3 million deaths annually, 85% of which are in Africa. The four species of plasmodia that infect humans are Plasmodium vivax, Plasmodium ovale, Plasmodium malariae, and Plasmodium falciparum. These species share a common life cycle. Human infection is initiated by the bite of an Anopheles mosquito, which introduces infectious plasmodia sporozoites via its saliva into the circulatory system. Human Malarial Parasites Parasite Plasmodium vivax Disease Benign tertian or vivax malaria P. ovale P. malariae P. falciparum Benign tertian or ovale malaria Quartan or malarial malaria Malignant tertian or falciparum malaria Life cycle of Plasmodium species. Asexual reproduction (Human Liver and Red Blood Cells) Sexual reproduction (Anopheles midgut) Salivary glands Liver Red Blood Cells Midgut Plasmodium falciparum: Blood Stage Parasites A: Stages of P. falciparum in thin blood smears. Fig. 1: Normal red cell; Figs. 218: Trophozoites (among these, Figs. 2-10 correspond to ring-stage trophozoites); Figs. 19-26: Schizonts (Fig. 26 is a ruptured schizont); Figs.27, 28: Mature macrogametocytes (female); Figs. 29, 30: Mature microgametocytes (male). Illustrations from: Coatney GR, Collins WE, Warren M, Contacos PG. The Primate Malarias. Bethesda: U.S. Department of Health, Education and Welfare; 1971 The sporozoites are carried to the parenchymal cells of the liver, where asexual reproduction (schizogony) occurs. This phase of growth is termed the exoerythrocytic cycle and lasts 8 to 25 days, depending on the plasmodial species. Some species (e.g., P. vivax, P. ovale) can establish a dormant hepatic phase in which the sporozoites (called hypnozoites or sleeping forms) do not divide. The presence of these viable plasmodia can lead to the relapse of infections months to years after the initial clinical disease (relapsing malaria). The hepatocytes eventually rupture, liberating the plasmodia (termed merozoites at this stage), which in turn attach to specific receptors on the surface of erythrocytes and enter the cells, thus initiating the erythrocytic cycle. Asexual replication progresses through a series of stages (ring, trophozoite, schizont) that culminates in the rupture of the erythrocyte, releasing up to 24 merozoites, which initiates another cycle of replication by infecting other erythrocytes. Some merozoites also develop within erythrocytes into male and female gametocytes. If a mosquito ingests mature male and female gametocytes during a blood meal, the sexual reproductive cycle of malaria can be initiated, with the eventual production of sporozoites infectious for humans. This sexual reproductive stage within the mosquito is necessary for the maintenance of malaria within a population. Most malaria seen in the United States is acquired by visitors or residents of countries with endemic disease (imported malaria). However, the appropriate vector Anopheles mosquito is found in several sections of the United States, and domestic transmission of disease has been observed (introduced malaria). In addition to transmission by mosquitoes, malaria can also be acquired by blood transfusions from an infected donor (transfusion malaria). This type of transmission can also occur among narcotic addicts who share needles and syringes ("mainline" malaria). Congenital acquisition, although rare, is also a possible mode of transmission (congenital malaria). . Sporozoa 3-1-PLASMODIUM VIVAX P. vivax is selective in that it invades only young, immature erythrocytes. In infections caused by P. vivax, infected red blood cells are usually enlarged and contain numerous pink granules or Schüffner's dots, the trophozoite is ring shaped but amoeboid in appearance, more mature trophozoites and erythrocytic schizonts containing up to 24 merozoites are present, and the gametocytes are round. These characteristics are helpful in identifying the specific plasmodial species, which is important for the treatment of malaria. Plasmodium vivax ring forms and young trophozoites. Note the multiple stages of the parasite (rings and trophozoite) seen in the peripheral blood smear, the enlarged parasitized erythrocytes, and the presence of Schüffner's dots with the trophozoite form. These are characteristic of P. vivax infections. Epidemiology P. vivax is the most prevalent of the human plasmodia, with the widest geographic distribution, including the tropics, subtropics, and temperate regions. Clinical Syndromes After an incubation period (usually 10 to 17 days) the patient experiences vague influenza-like symptoms with headache, muscle pains, photophobia, anorexia, nausea, and vomiting. Clinical Syndromes As the infection progresses, increased numbers of rupturing erythrocytes liberate merozoites and toxic cellular debris and hemoglobin into the circulation. Together, these produce the typical pattern of chills, fever, and malarial rigors. These paroxysms usually reappear periodically (generally every 48 hours) as the cycle of infection, replication, and cell lysis progresses. The paroxysms may remain relatively mild or progress to severe attacks, with hours of sweating, chills, shaking, persistently high temperatures (103° to 106°F [39° to 41°C]), and exhaustion. Clinical Syndromes P. vivax causes "benign tertian malaria," which refers to the cycle of paroxysms every 48 hours (in untreated patients) and the fact that most patients tolerate the attacks and can survive for years without treatment. If left untreated, however, chronic P. vivax infections can lead to brain, kidney, and liver damage as a result of the malarial pigment, cellular debris, and capillary plugging of these organs by masses of adherent erythrocytes. Laboratory Diagnosis Microscopic examination of thick and thin films of blood is the method of choice for confirming the clinical diagnosis of malaria and identifying the specific species responsible for disease. The thick film is a concentration method and may be used to detect the presence of organisms. With training, thick films may be used to diagnose the species as well. The thin film is most useful for establishing species identification. Blood films can be taken at any time over the course of the infection, but the best time is midway between paroxysms of chills and fever, when the greatest numbers of intracellular organisms are present. Laboratory Diagnosis It may be necessary to take repeated films at intervals of 4 to 6 hours. Serologic procedures are available, but they are used primarily for epidemiologic surveys or for screening blood donors. Serologic findings usually remain positive for approximately a year, even after complete treatment of the infection. Sporozoa 3-2-PLASMODIUM OVALE Physiology and Structure P. ovale is similar to P. vivax in many respects, including its selectivity for young, pliable erythrocytes. As a consequence, the host cell becomes enlarged and distorted, usually in an oval form. Schüffner's dots appear as pale-pink granules, and the cell border is frequently fimbriated or ragged. The schizont of P. ovale, when mature, contains approximately half the number of merozoites seen in P. vivax. Epidemiology P. ovale is distributed primarily in tropical Africa, where it is often more prevalent than P. vivax. It is also found in Asia and South America. Clinical Syndromes The clinical picture of tertian attacks for P. ovale (benign tertian or ovale malaria) infection is similar to that for P. vivax. Untreated infections last only approximately a year instead of the several years for P. vivax. Both relapse and recrudescence phases are similar to P. vivax. Laboratory Diagnosis As with P. vivax, thick and thin blood films are examined for the typical oval host cell with Schüffner's dots and a ragged cell wall. Serologic tests reveal cross-reaction with P. vivax and other plasmodia. Sporozoa 3-3-PLASMODIUM MALARIAE Physiology and Structure In contrast with P. vivax and P. ovale, P. malariae can infect only mature erythrocytes with relatively rigid cell membranes. As a result, the parasite's growth must conform to the size and shape of the red blood cell. This produces no red cell enlargement or distortion, as seen in P. vivax and P. ovale, but it does result in distinctive shapes of the parasite seen in the host cell: "band and bar forms," as well as very compact, dark-staining forms. The schizont of P. malariae shows no red cell enlargement or distortion and is usually composed of eight merozoites appearing in a rosette. Occasionally, reddish granules called Ziemann's dots appear in the host cell. Unlike for P. vivax and P. ovale, hypnozoites of P. malariae are not found in the liver, and relapse does not occur. Recrudescence does occur, and attacks may develop after apparent abatement of symptoms. Epidemiology P. malariae infection occurs primarily in the same subtropical and temperate regions as the other plasmodia but is less prevalent. Clinical Syndromes The incubation period for P. malariae is the longest of the plasmodia, usually 18 to 40 days, but possibly several months to years. The early symptoms are influenza-like, with fever patterns of 72 hours (quartan or malarial malaria) in periodicity. Attacks are moderate to severe and last several hours. Untreated infections may last as long as 20 years. Laboratory Diagnosis Observing the characteristic bar and band forms and the rosette schizont in thick and thin films of blood establishes the diagnosis of P. malariae infection. As already noted, serologic tests cross-react with other plasmodia. Sporozoa 3-4-PLASMODIUM FALCIPARUM Physiology and Structure P. falciparum demonstrates no selectivity in host erythrocytes and invades any red blood cell at any stage in its existence. Also, multiple sporozoites can infect a single erythrocyte. Thus three or even four small rings may be seen in an infected cell. P. falciparum is often seen in the host cell at the very edge or periphery of the cell membrane, appearing almost as if it were "stuck" on the outside of the cell. This is called the appliqué or accolé position and is distinctive for this species. Ring forms of Plasmodium falciparum. Note the multiple ring forms within the individual erythrocytes, which is characteristic of this organism. Growing trophozoite stages and schizonts of P. falciparum are rarely seen in blood films because their forms are sequestered in the liver and spleen. Only in very heavy infections are they found in the peripheral circulation. Thus, peripheral blood smears from patients with P. falciparum malaria characteristically contain only young ring forms and, occasionally, gametocytes. The typical crescentic gametocytes are diagnostic for the species. Erythrocytic Stages of P. falciparum Ring Mature gametocyte of P. falciparum. The presence of this sausage-shaped form is diagnostic of P. falciparum malaria. Infected red blood cells do not enlarge and become distorted, like they do with P. vivax and P. ovale. Occasionally, reddish granules known as Maurer's dots are observed in P. falciparum. P. falciparum, like P. malariae, does not produce hypnozoites in the liver. Relapses from the liver are not known to occur. Sporozoa 3-4-PLASMODIUM FALCIPARUM Epidemiology P. falciparum occurs almost exclusively in tropical and subtropical regions. Clinical Syndromes The incubation period of P. falciparum is the shortest of all the plasmodia, ranging from 7 to 10 days, and does not extend for months to years. After the early influenza-like symptoms, P. falciparum rapidly produces daily (quotidian) chills and fever, as well as severe nausea, vomiting, and diarrhea. The periodicity of the attacks then becomes tertian (36 to 48 hours), and fulminating disease develops. The term malignant tertian malaria is appropriate for this infection. Because the symptoms of this type of malaria are similar to those of intestinal infections, the nausea, vomiting, and diarrhea have led to the observation that malaria is "the malignant mimic." Although any malaria infection may be fatal, P. falciparum is the most likely to result in death if left untreated. The increased numbers of erythrocytes infected and destroyed result in toxic cellular debris, adherence of red blood cells to vascular endothelium and to adjacent red blood cells, and formation of capillary plugging by masses of red blood cells, platelets, leukocytes, and malarial pigment. Involvement of the brain (cerebral malaria) is most often seen in P. falciparum infection. Capillary plugging from an accumulation of malarial pigment and masses of cells can result in coma and death. Kidney damage is also associated with P. falciparum malaria, resulting in an illness called blackwater fever. Intravascular hemolysis with rapid destruction of red blood cells produces a marked hemoglobinuria (hemoglobinuria is a condition in which the oxygen transport protein hemoglobin is found in abnormally high concentrations in the urine) and can result in acute renal failure, tubular necrosis, nephrotic syndrome, and death. Liver involvement is characterized by abdominal pain, vomiting of bile, severe diarrhea, and rapid dehydration. Sporozoa 3-4-PLASMODIUM FALCIPARUM Laboratory Diagnosis Thick and thin blood films are searched for the characteristic rings of P. falciparum, which frequently occur in multiples within a single cell, as well as in the accolé position. The distinctive crescentic gametocytes are also diagnostic. Laboratory personnel must perform a thorough search of the blood films because mixed infections can occur with any combination of the four species, but most often the combination is P. falciparum and P. vivax. The detection and proper reporting of a mixed infection directly affects the treatment chosen.