Microbiology 52 [9-2
advertisement

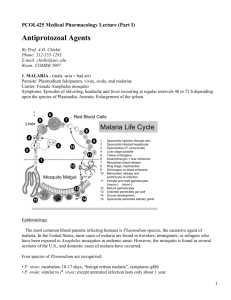
Microbiology 52 Blood and Tissue Protozoa Key Concepts: - - - Tissue invasive have intracellular stage Fever symptom of disseminated protozoal infection Plasmodium falciparum (malaria) more virulent and likely to be resistant to drugs o Distinguish promptly Babesiosis = protozoal infection of erythrocytes (transmitted by ticks) Cats are intestinal host for Toxoplasma gondii; other animals have dormant cyst in muscles and viscera o In humans, mono-like primary infection, chorioretinitis, congenital infection, or mass in lesions in brain (if AIDS) Leishmania species virulence fctors determine if skin ulcer or disseminiated chronic febrile illness (liver, spleen, lymph nodes) Infection with Chagas (Trypanosoma cruzi) may damage heart and GI tract African sleeping sickness (Trypanosoma brucei) evades host by antigenic variation Bloodstream infection -> anemia (destroy RBCs) o Malaria and babesiosis Tissue infection -> damage to eye, brain, heart (toxoplasmosis); brain (African sleeping sickness); heart and GI tract (Chagas) Parasites of RBCs - Plasmodium species o Malaria caused by P. falciparum, P. vivax, P. ovale and P. malariae Humans only reservoir o Transmitted by mosquito vector (female anopheles) Symptoms 8-30 days after bite Most carried over to nonendemic areas = imported malaria o Transmitted by blood transfusion or sharing of needles = induced malaria o Inhabit salivary gland of mosquito as sporozoite (infectious to human) Injected into bloodstream and enter liver cells -> mature and increase (hepatocellular cycle) Released back into blood as merozoites (infectious to RBCs) -> divide and mature (shiznots, ring, trophozoits) = erythrocytic cycle -> lyse host and infect other RBCs o Multiply asexually (fission) Some merozoites are sexual (haploid) = gametocytes -> fuse in mosquito to form diploid and then meiosis -> sporozoites (haploid) o P. falciparum invades all age RBCs (high mortality) o o o o o o o o o o o P. vivax invades reticulocytes and young RBCs P. ovale almost identically Both may harbor in liver for long period so cause relapse/recurrent malaria Dormant parasites = hypnozoites P. malariae infects 1-2% of RBCs (less severe) RBC infection makes them less deformable -> spleen recognizes and removes (splenomegaly) Also P. falciparum infection have “knoblike” structures containing pfEMP-1 -> binds to receptors on cells of venules and capillaries (intercellular adhesion molecule 1, ICAM-1 and CD36) -> block BF so don’t get to spleen Clinically: fever, chills, anemia RBC lysis releases glycophosphatidylinositol (GPI) stimulating TNF and IL-1 in macrophages -> chill and fever Regular, periodic fever from synchronized lysis 2 days w/ P. vivax/ovale; 3 days with P. malariae; irregular with P. falciparum May also have muscle aches, malaise, and gastroenteritis Diagnosis: Giemsa-stained smear using oil immersion If parasitemia is low, “thick smear” increases sensitivity Lyses RBCs in process so no info on intracellular location of parasite “thin smear” differentiates among Plasmodium species Serologic testing bad because too long; use PCR Acutely ill usually P. falciparum or P. vivax Differentiate by: P. vivax produces “stippling” (Schuffner dots) P. malariae cuases subacute or chronic infections Natural immunity imperfect but may allow less sever infection Merozoite major surface protein (MSP-1) undergoes antigenic variation Thwarts natural immunity and vaccination Chloroquine widley used for chemoprophylaxis and treatment Enters parasite’s food vacuole and blocks heme detoxification (kills parasite) Resistance by mutation of membrane protein causing drug pump out of food No resistance in Haiti by P. falciparum resistance in Asia, S America, Africa o Treat with malarone, mefloquine, quinine, quinidine, halofantrine, or atesunate o Doxycycline as chemoprophylaxis before traveling to SE Asia Only antimalarial effective against hypnozoite stage of P. vivax/ovale = primaquine (used with chloroquine) Causes nausea, vomiting, and diarrhea Hemolysis in G6PD patients o - Insecticides and drainage of water breeding sites can control malaria (expensive and not effective) Use netting, screening and insect repellants Babesia species o Infect RBCs and generate fever o Babesia microti mostly in US Concentrated in same area as Lyme disease (Borrelia burgdorferi) because infect same reservoir (white-footed mouse) and use same deer tick (Ixodes scaplaris) Outside of Midwest to Pacific, usually B. divergens o Illness is nonspecific (flulike) = “summer flu” More severe in splenectomized o Infects 0.2% of RBCs o Hard-bodied tick inject merozoites -> infect RBCs -> binary fission (form tetrads and lyse) o Giemsa-stain with oil immersion = rings in tetrads Distinguish between P. falciparum and Babesia for treatment Use clindamycin + quinine for babesiosis Tissue Protozoa - Toxoplasma gondii o Less than 1% diagnosed o 3 syndromes Mono-like syndrome (Epstein-Barr virus and CMV negative) Congenital infection (bad in first trimester) Infections of immunocompromised (AIDs) in brain and heart o Acquired through eating inadequately cooked meat (lamb, mutton, beef) or feces of cats (oocysts) Toxoplasmosis absent from areas that don’t have cats o Oocysts mature to tachyzoites -> enter blood and disseminate -> immune response eliminates active tachyzoites and leaves dormant cysts -> immunosuppression causes reactivation o Found in macrophages (enters via invasion) Parasitophorous vesicle invisible to host cell with no endocytic proteins o Elevated antibody titer (IgM) in normal host and self-limited o In immunocompromised -> neurologic symtoms and ring-enhancing lesions in CT or MRI Stain brain biopsy with antitoxoplasma antibodies for sensitivity o Local inflammation -> necrosis, tissue damage, death Treat with pyrimethamine and sulfadiazine or clindamycin o Fetus acquisition fatal so women screened for antitoxoplasma antibody when married or first pregnancy detection Complications greatest for serconversion in first trimester Chorioretinitis = only manifestations of congenital infection - - - - Leishmania Species o Produce superficial ulcers, lesions in liver, spleen and BM, fever, weight loss, and anemia o Superficial lesions in species growing at lower temperatures (25-30°C) o Invasion of viscera in species growing at 37°C o Possess prominent flagellum connected to kinetoplast (own DNA) o Bite of phlebotomine sand flies in tropical areas Reservoirs = rodents, dogs, infected humans o Cause skin ulcers, mucocutaneous lesions (espundia), disseminated cutaneous leishmaniasis, and disseminated visceral leishmaniasis (kala azar) o Parasite protein binds complement on macrophage -> phagocytosis -> superoxide dismutase protects them -> differentiate into amastigote (nonflagellated) -> resistant to lysosomes o Immunity via interferon-gama (Th1 response) To survive, has antigens that produces Th2 response (protective) o Fever in AIDS patients in Mediterranean o Culture media to distinguish species o Treat with antimony-containing compounds, or allopurinol or ketoconazole Trypanosoma cruzi o Chagas disease o Bite of reduviid bug (kissing bug) -> feces of bug goes into bite by itching -> most have fever, revor, and asymptomtic Complications from GI nerve damage (megaesophagus, megacolon), conducting heart tissue (right bundle branch block) or cardiomyopathy Sudden death from cardiac arrhythmia o Fibrosis = hallmark o Diagnosis based on appearance, antibody titers positive for years o Treat with nifrutimox or benznidazole Trypanosoma brucei o African sleeping sickness o Bite of infected tsetse flies (Glossina; in salivary glands) and undergoes antigenic variation o Main reservoirs are wild game (E Africa) or domestic animals (W Africa) o Trypanosomes in blood (parasatiemia) -> several months/years invade CNS Each bout, changes variable surface glycoprotein to avoid host (genetic rearrangement) o Eflornithine, pentamidine and suramin are useful in systemic stage Free-living Amebas o Naegleria, Acanthamoeba, Hartmanella have no animal reservoirs o Naegleria fowleri (amebic meningoencephalitis) in young people from warm, freshwater lakes enters CNS via cribriform plate on olfactory nerve o Acanthamoeba or Hartmanella in in older immunocompromised o CNS via bloodstream Acanthamoeba infects cornea (keratitis) and causes blindless -> treat with imidazoles Treat with amphotericin B, miconazole, and rifampin