3.3. Null mutation in CPH1 decreased susceptibility to antifungal
advertisement

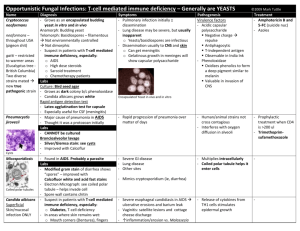
Cph1p negatively regulates MDR1 involved in drug resistance in Candida albicans Hsiu-Jung Lo a,b, Kuo-Yun Tseng a,1, Yeong-Yi Kao c, Ming-Yang Tsao a, Han-Lun Lo c, Yun-Liang Yang c,d,* a National Institute of Infectious Diseases and Vaccinology, National Health Research Institutes, Miaoli, Taiwan b School of Dentistry, China Medical University, Taichung, Taiwan c Department of Biological Science and Technology, National Chiao Tung University, Hsinchu, Taiwan d Institute of Molecular Medicine and Bioengineering, National Chiao Tung University, Hsinchu, Taiwan ARTICLE INFO Article history: Received 4 July 2014 Accepted 22 January 2015 Keywords: Candida albicans Drug resistance Efflux pump Virulence factor Regulation * Corresponding author. Present address: Department of Biological Science and Technology, National Chiao Tung University, Hsinchu, Taiwan, ROC. Tel.: +886 3 571 2121 x56920; fax: +886 3 572 9288. E-mail address: yyang@mail.nctu.edu.tw (Y.L. Yang). 1 Present address: Institute of Cellular and Systems Medicine, National Health Research Institutes, Miaoli, Taiwan. ABSTRACT The cph1/cph1 efg1/efg1 double mutant in Candida albicans is defective in filamentous growth and is avirulent in a mouse model. We previously reported that Efg1p but not Cph1p is involved in drug resistance by negatively regulating ERG3 in C. albicans. In the current study, we have found that overexpression of CPH1 in Saccharomyces cerevisiae increases susceptibility to the antifungal drug fluconazole. Furthermore, in C. albicans, null mutation of CPH1 increased the expression of MDR1 as well as decreased susceptibility to fluconazole and voriconazole but not to amphotericin B. These findings indicate that although Efg1p and Cph1p may have the same effects on virulence, they have opposite effects on drug resistance in C. albicans. 1. Introduction In the past two decades, yeast infections have increased significantly. Among them, Candida albicans is the most frequently isolated fungal pathogen in humans and causes morbidity in immunocompromised hosts [1,2]. Coincident with the increased use of antifungal agents, the incidence of drug resistance has increased [3,4]. However, the mechanisms of drug resistance are not well characterised. Overexpression of efflux pumps and the drug target are major mechanisms contributing to drug resistance in clinical isolates of C. albicans. At least two active efflux pumps are involved in drug resistance: CDR1, belonging to the ATP-binding cassette (ABC) family; and MDR1, belonging to the major facilitator superfamily (MFS). The CDR1 gene was identified by complementing the hypersensitive phenotype to azoles, cycloheximide and chloramphenicol in the PDR5 null mutant in Saccharomyces cerevisiae [5]. Overexpression of CDR1 in S. cerevisiae causes resistance to azole-based antifungal drugs. Recently, two transcription factors, CaNdt80p and CaTac1p, have been identified as positive regulators of CDR1. Consistently, mutations in NDT80 and TAC1 increase the susceptibility to more than one azole type drug [6–9]. The MDR1 gene was primarily identified by its ability to confer both benomyl and methotrexate resistance when transformed into S. cerevisiae [10]. Its expression is induced by drugs such as benomyl, methotrexate, 4-nitroquinoline N-oxide (4NQO), o-phenanthroline and sulfometuron methyl [11]. Overexpression of MDR1 contributes to fluconazole resistance in C. albicans [12]. Mrr1p has been reported as a positive regulator [13], and both Cap1p and Rep1p are negative regulators of MDR1 [14,15]. The predominant target of the azole-based drugs is lanosterol demethylase, the product of ERG11. ERG3, a gene upstream of ERG11, that encodes the sterol 5,6-desaturase, produces a toxic product, 14-methylergosta-8,24-dien-3,6-diol, following azole treatment [16]. Furthermore, it has been reported that null mutation of ERG3 causes fluconazole resistance [17]. STE12 in S. cerevisiae, a transcription factor that is the target of the pheromone response mitogen-activated protein kinase cascade, is involved in mating and filamentous growth. CPH1 in C. albicans was identified by complementing both defects in mating and filamentous growth of ste12 mutants [18]. Cph1p and Ste12p have 74% identical residues among the region containing DNA-binding domains. Furthermore, they use identical residues for pheromone-induced transcription activation. Thus, like Ste12p in S. cerevisiae, Cph1p in C. albicans also binds to pheromone response elements (PREs) and is involved in mating and filamentous growth [18,19]. However, a null mutation of CPH1 does not affect filamentous growth in medium containing serum or the virulence in a mouse systemic infection model [20] owing to other Cph1p-independent pathways. It has been reported that the cph1/cph1 efg1/efg1 double mutant fails to form filaments in vitro and does not cause lethal infections in a mouse model [20,21]. The observation that Efg1p, but not Cph1p, regulates ERG3 and that the null mutations of EFG1 increase the susceptibility of the cells to antifungal agents demonstrates that a transcription factor can be responsible both for drug resistance and virulence [22]. Later, more transcription factors, such as Ndt80p, were reported to be involved in different pathways by regulating different sets of targets [9,23]. Recently, a 35-bp MDR1 promoter element (MDRE) containing the Mcm1p-binding site has been identified. Interestingly, a sequence similar to the PRE overlaps the boundary of the MDRE [24]. In the current study, we found that Cph1p negatively regulates the expression of MDR1 involved in drug resistance in C. albicans. 2. Materials and methods 2.1. Strains and media The S. cerevisiae strain used in this study was Sigma 10560-2B MATa his3::hisG leu2::hisG ura3-52 [6]. A high-copy-number vector pRS426 alone or HLB126 (pRS426-CPH1) was transformed into S. cerevisiae 10560-2B to investigate the effects on drug susceptibility of overexpressing CPH1. The C. albicans strains used in this study were SC5314 (CPH1/CPH1), the wild-type strain [25]; JKC19, the cph1/cph1 null mutant strain, ura3::imm434/ ura3::imm434 cph1::hisG/cph1::hisG -URA3-hisG [18]; and YLO323 (cph1/cph1::CPH1), the cph1/cph1 null mutant with a copy of the wild-type CPH1 allele rescued strain, ura3::imm434/ ura3::imm434 cph1::hisG/cph1::hisG::CPH1-URA3. YLO323 was constructed in this study because we failed to detect the CPH1 mRNA of JKC28 strain (ura3::imm434/ ura3::imm434 cph1::hisG/cph1::hisG::CPH1URA3). Yeast–peptone–dextrose (YPD) (1% yeast extract, 2% peptone and 2% dextrose) and synthetic dextrose (SD) (0.67% yeast nitrogen base without amino acid and 2% dextrose) were prepared as described previously [26]. The compounds added to media were from Difco (Henry St, Detroit, MI, USA) unless otherwise stated. 2.2. Antifungal susceptibility testing Etest was used to determine the susceptibility to antifungal agents as described previously [22]. Homogenised isolated colonies grown on SD agar medium overnight were transferred in 0.85% NaCl to achieve a density of 5 106 cells/mL. A sterile swab was dipped into inoculum suspension and was used to swab the entire agar surface of SD agar medium evenly. Fluconazole Etest strips (0.016–256 mg/L; AB BIODISK, Solna, Sweden) were applied on the plate when the excess moisture was absorbed completely. The agar dilution method was also used to determine the susceptibility to antifungal agents for C. albicans. First, cells were diluted to an optical density at 600 nm (OD600) of 2 (ca. 2 107 CFU/mL) and were spotted (ca. 0.5 L per spot) onto different drug plates with 10-fold serial dilutions. Stock solutions of antifungal drugs were prepared by dissolving drugs in dimethyl sulfoxide (DMSO). The final concentrations of fluconazole and voriconazole were 25 mg/L and 2 mg/L, respectively, in medium containing 1% DMSO. The broth microdilution method was performed according to the guidelines published by the Clinical and Laboratory Standards Institute (CLSI) [27]. The highest concentrations of amphotericin B, fluconazole and voriconazole were 0.5, 16 and 1 mg/L, respectively, and a two-fold serial dilution was applied. The final growth of each isolate was measured using a Biotrak II Visible Plate Reader (Amersham Biosciences, Piscataway, NJ, USA) after 2 days of incubation at 30 C. Growth of cells in the absence of drug was defined as 100 and the relative growth of cells in the presence of different concentrations of drug was normalised accordingly. 2.3. RNA isolation Candida albicans cells were harvested after being grown in 20 mL of YPD liquid medium in the absence or presence of 100 g/mL 4-NQO at 30 C for 1 h (OD600 = 0.7~1.0). Total RNA was isolated by the method of acid hot phenol followed by RQ1 RNase-Free DNase (Promega, Madison, WI, USA) treatment to digest the possible contaminating DNA. 2.4. Northern blot analysis RNA samples (20 g each) were separated by electrophoresis on 1% formaldehyde-agarose gel and were then transferred to Nylon membranes with a positive charge (Roche, Indianapolis, IN, USA) in 20 SSC (3 M NaCl, 0.3 M sodium citrate). The membrane was hybridised to a digoxigenin (DIG)-labelled probe prepared using a PCR DIG Probe Synthesis Kit (Roche) according to the manufacturer’s instructions. The level of ACT1 mRNA was used as the loading control. 2.5. Quantitative analysis of mRNA level by real-time PCR Real-time PCR was performed in a Rotor-Gene 3000 instrument (Corbett Research, Sydney, Australia) with a TITANIUM Taq PCR Kit (BD Clontech, Mountain View, CA,USA) and SYBR Green I Nucleic Acid Stain (Cambrex, Rockland, ME, USA) to determine the level of mRNA as described previously [8]. The sample set-up was processed automatically using a CAS-1200TM (Corbett Research). Real-time PCR was performed according to the manufacturer’s instructions and the expression of ACT1 (for miconazole treatment) or CaSNF3 (for 4-NQO treatment) in each strain was used as the loading control. The relative quantitation was based on two standard curves for comparison and the results were given as a ratio [28]. The level of mRNA isolated from wild-type cells in the absence of drug was defined as 1. The relative level of mRNA isolated from different strains in the absence or presence of drugs was normalised accordingly. 3. Results and discussion 3.1. Overexpression of CPH1 increased susceptibility to fluconazole in Saccharomyces cerevisiae We determined whether Cph1p, like Efg1p, is involved in drug resistance as well as virulence. First, the involvement of CPH1 in fluconazole susceptibility in S. cerevisiae was investigated. Interestingly, cells overexpressing CPH1 were more susceptible to fluconazole than control cells (24 mg/L vs. 64 mg/L) (Fig. 1), suggesting that Cph1p may be a negative regulator of drug resistance. 3.2. The null mutation of CPH1 increased the expression of MDR1 in Candida albicans To elucidate the regulatory network of Cph1p in C. albicans, we determined whether Cph1p regulates the expression of known genes involved in drug resistance. The results are summarised in Table 1. Expression of MDR1 in wildtype CPH1/CPH1 cells was induced significantly by 4-NQO (1 vs. 97.9), which is consistent with a previous report [29]. In the presence of 4-NQO, the null mutation of CPH1 further increased the expression of MDR1 by ca. 2.8-fold (97.9 vs. 269.8). The level of MDR1 mRNA in the cph1/cph1 mutant cells containing a wild-type copy of CPH1 was reduced to that of the CPH1/CPH1 wild-type cells (104.8 vs. 97.9), suggesting that the increased level of MDR1 mRNA results from the null mutation of CPH1. In the absence of 4-NQO, the level of MDR1 mRNA in the cph1/cph1 mutant cells was similar to that in the CPH1/CPH1 wild-type cells, suggesting that Cph1p is not involved in the basal expression of MDR1. To further assess whether Cph1p regulates the expression of MDR1, levels of MDR1 mRNA of different C. albicans strains were determined by northern blot assay. In the absence of 4-NQO, the level of MDR1 mRNA was low and was barely detectable (Fig. 2, lane 1). As expected, expression of MDR1 in the CPH1/CPH1 wild-type cells was highly induced by the addition of 4-NQO (Fig. 2, comparing lanes 1 and 2). Expression of MDR1 was further induced by the null mutation of CPH1 (Fig. 2, comparing lanes 2 and 4), suggesting that Cph1p is a repressor of MDR1. That the level of MDR1 mRNA in the cph1/cph1 mutant cells containing a wild-type copy of CPH1 was reduced to that of the wild-type CPH1/CPH1 cells demonstrated that the increased level of MDR1 mRNA in the cph1/cph1 cells is indeed caused by the null mutation of CPH1. In general, inhibition of one efflux pump may result in overexpression of another different efflux pump as a compensatory mechanism. Thus, we also determined whether the null mutation of CPH1 affects the expression of CDR1 in the presence of 4-NQO. First, unlike MDR1, the expression of CDR1 was not induced significantly by 4-NQO. Expression of CDR1 was similar both in the CPH1/CPH1 wild-type cells and in the cph1/cph1 null mutant cells in the absence (1.0 vs. 1.0) and presence (1. 8 vs. 2.2) of 4-NQO. Expression of MDR1 is barely detectable in the presence of miconazole, consistent with previous reports that the expression of MDR1 is not induced by miconazole. In contrast, expression of CDR1, CDR2, ERG3 and ERG11 were induced by miconazole by ca. 3.2-, 6.9-, 3.2- and 3.4-fold, respectively. These findings indicate that Cph1p acts as a transcription repressor of MDR1 specifically in C. albicans even though the expression of CDR1 (0.8; 3.2 vs. 2.4), CDR2 (0.7; 6.9 vs. 4.9), ERG3 (0.9; 3.2 vs. 2.9) and ERG11 (0.7; 3.2 vs. 2.5) in the presence of miconazole was slightly reduced by the null mutation of CPH1. Recently, Mcm1p has been identified as a positive regulator of MDR1. The promoter of MDR1 from SC5314, the wild-type laboratory strain, does not contain the PRE sequence (TGAAACA), a conserved binding site of Ste12p. Interestingly, sequence TGACACA, similar to a PRE, was identified near the binding site of Mcm1p [24]. Furthermore, in some clinical isolates, such as B792, a PRE sequence can be found at the same location [10]. Here we proposed a working model for how Cph1p regulates the transcription of MDR1. Cph1p alone or in the Cph1p–Mcm1p complex binds the MDR1 promoter and represses the expression of MDR1. Under inducing conditions, Cph1p will be released from the promoter of MDR1 either by modification of Cph1p or the involvement of another regulator. Alternatively, the effect of the complex of Cph1p–Mcm1p will be reversed by the involvement of another regulator. Whether Cph1p regulates the expression of MDR1 through directly binding to its promoter is under investigation. 3.3. Null mutation in CPH1 decreased susceptibility to antifungal drugs in Candida albicans Since the null mutation of CPH1 increased the expression of MDR1, it is a possibility that cph1/cph1 mutant cells are less susceptible to antifungal drugs than wild-type cells. First, the agar dilution method was used to determine the susceptibility to antifungal drugs of different strains as described previously [6]. Cells of different strains grew well on medium containing DMSO in the absence of drug (Fig. 3, left panel), suggesting that the null mutation of CPH1 does not affect the growth rate of C. albicans as previously reported [14]. Interestingly, more cph1/cph1 mutant cells grew on medium containing fluconazole (Fig. 3, middle panel) and voriconazole (Fig. 3, right panel) than the wild-type strain. The drug susceptibilities of the cph1/cph1 mutant cells were restored by a wild-type copy of CPH1 (cph1/cph1::CPH1), suggesting that the decreased drug susceptibilities in the cph1/cph1 cells results from the null mutation in CPH1. Thus, null mutations on CPH1 decreased the susceptibilities to both fluconazole and voriconazole. To confirm the effect of Cph1p on drug susceptibility, we also quantified the drug susceptibility of different strains by a broth microdilution method. Again, the cph1/cph1 mutant cells were more resistant to fluconazole (Fig. 4B) and voriconazole (Fig. 4C) than the CPH1/CPH1 wild-type cells and the cph1/cph1 with a copy of CPH1 wild-type allele (cph1/cph1::CPH1) cells, consistent with the results of the agar dilution assay. To investigate whether Cph1p is also involved in drug resistance of a different type of drug, susceptibility to amphotericin B was also determined. In contrast, the null mutation of CPH1 had no effect on susceptibility to amphotericin B (Fig. 4A). These results showed that Cph1p negatively regulates the expression of MDR1 but not other tested genes known to be involved in drug resistance, including CDR1, CDR2, ERG3 and ERG11. Interestingly, mutations in CPH1 decreased susceptibility to other azole drugs in addition to fluconazole, although MDR1 was reported to be the efflux pump contributing to fluconazole resistance specifically [4]. In the absence of stimulus, cph1/cph1 mutant cells did not lose their fitness in vitro (Fig. 3A) or in vivo [20], since the null mutation of CPH1 does not affect the basal expression of MDR1. The observation that cph1/cph1 mutant cells were more resistant to azole drugs may result from higher expression of MDR1 and/or other novel genes. Hence, a genome-wide approach to identify additional targets of Cph1p involved in azole drug resistance is needed. Furthermore, it would be interesting to investigate whether there are residues of Cph1p specifically responsible for regulating MDR1. Genes regulating both drug resistance and virulence have been suggested previously. Recently, we reported that Efg1p is involved in drug resistance by negatively regulating ERG3 [22]. A null mutation of EFG1 increased the susceptibility to drugs. In current study, we showed that Cph1p, a protein involved in virulence, is also involved in negatively regulating the expression of MDR1, which is responsible for drug resistance in C. albicans. And in this case, a null mutation of CPH1 decreases the susceptibility to drugs. These findings indicate that although Efg1p and Cph1p can have the same effects on virulence, they regulate different targets resulting in opposite effects on drug resistance in C. albicans. It is important to investigate how a transcription factor regulates both virulence and drug resistance. There are multiple interconnected pathways in C. albicans responsible for different sets of environmental conditions [30]. Hence, how Cap1p, Cph1p, Mrr1p and Rep1p co-regulate drug resistance pathways, particularly through MDR1, in C. albicans requires further investigation. Acknowledgments: The authors would like to thank Ms Y.H. Lin, C.L. Su and C.G. Chen (National Health Research Institutes, Miaoli, Taiwan) for their technical assistance. The authors would also like to thank Dr G.R. Fink for Saccharomyces cerevisiae strain 10560-2B. Funding: This work was supported in part by grants from the National Science Council [102-2320-B-009-001 to Y-LY and 102-2311-B-400-001 to H-JL] and the National Health Research Institutes [IV-103-PP-08 to H-JL]. Competing interests: None declared. Ethical approval: Not required. References [1] Pfaller MA, Diekema DJ, Jones RN, Sader HS, Fluit AC, Hollis RJ, et al. International surveillance of bloodstream infections due to Candida species: frequency of occurrence and in vitro susceptibilities to fluconazole, ravuconazole, and voriconazole of isolates collected from 1997 through 1999 in the SENTRY antimicrobial surveillance program. J Clin Microbiol 2001;39:3254–9. [2] Hung CC, Yang YL, Lauderdale TL, McDonald LC, Hsiao CF, Cheng HH, et al. Colonization of human immunodeficiency virus-infected outpatients in Taiwan with Candida species. J Clin Microbiol 2005;43:1600–3. [3] White TC, Marr KA, Bowden RA. Clinical, cellular, and molecular factors that contribute to antifungal drug resistance. Clin Microbiol Rev 1998;11:382– 402. [4] Yang YL, Lo HJ. Mechanisms of antifungal agent resistance. J Microbiol Immunol Infect 2001;34:79–86. [5] Prasad R, De Wergifosse P, Goffeau A, Balzi E. Molecular cloning and characterization of a novel gene of Candida albicans, CDR1, conferring multiple resistance to drugs and antifungals. Curr Genet 1995;27:320–9. [6] Chen CG, Yang YL, Shih HI, Su CL, Lo HJ. CaNdt80 is involved in drug resistance in Candida albicans by regulating CDR1. Antimicrob Agents Chemother 2004;48:4505–12. [7] Coste AT, Karababa M, Ischer F, Bille J, Sanglard D. TAC1, transcriptional activator of CDR genes, is a new transcription factor involved in the regulation of Candida albicans ABC transporters CDR1 and CDR2. Eukaryot Cell 2004;3:1639–52. [8] Wang JS, Yang YL, Wu CG, Ouyang KJ, Tseng KY, Chen CG, et al. The DNA binding domain of CaNdt80p is required to activate CDR1 involved in drug resistance in Candida albicans. J Med Microbiol 2006;55:1403–11. [9] Yang YL, Wang CW, Leaw SN, Chang TP, Wang IC, Chen CG, et al. R432 is a key residue for the multiple functions of Ndt80p in Candida albicans. Cell Mol Life Sci 2012;69:1011–23. [10] Fling ME, Kopf J, Tamarkin A, Gorman JA, Smith HA, Koltin Y. Analysis of a Candida albicans gene that encodes a novel mechanism for resistance to benomyl and methotrexate. Mol Gen Genet 1991;227:318–29. [11] Ben Yaacov R, Knoller S, Caldwell GA, Becker JM, Koltin Y. Candida albicans gene encoding resistance to benomyl and methotrexate is a multidrug resistance gene. Antimicrob Agents Chemother 1994;38:648–52. [12] White TC. Increased mRNA levels of ERG16, CDR, and MDR1 correlate with increases in azole resistance in Candida albicans isolates from a patient infected with human immunodeficiency virus. Antimicrob Agents Chemother 1997;41:1482–7. [13] Morschhauser J, Barker KS, Liu TT, Blass-Warmuth J, Homayouni R, Rogers PD. The transcription factor Mrr1p controls expression of the MDR1 efflux pump and mediates multidrug resistance in Candida albicans. PLoS Pathog 2007;3:1603–16. [14] Alarco AM, Raymond M. The bZip transcription factor Cap1p is involved in multidrug resistance and oxidative stress response in Candida albicans. J Bacteriol 1999;181:700–8. [15] Chen CG, Yang YL, Tseng KY, Shih HI, Liou CH, Lin CC, et al. Rep1p negatively regulating MDR1 efflux pump involved in drug resistance in Candida albicans. Fungal Genet Biol 2009;46:714–20. [16] Sanglard D, Ischer F, Koymans L, Bille J. Amino acid substitutions in the cytochrome P-450 lanosterol 14-demethylase (CYP51A1) from azoleresistant Candida albicans clinical isolates contribute to resistance to azole antifungal agents. Antimicrob Agents Chemother 1998;42:241–53. [17] Sanglard D, Ischer F, Parkinson T, Falconer D, Bille J. Candida albicans mutations in the ergosterol biosynthetic pathway and resistance to several antifungal agents. Antimicrob Agents Chemother 2003;47:2404–12. [18] Liu H, Kohler J, Fink GR. Suppression of hyphal formation in Candida albicans by mutation of a STE12 homolog. Science 1994;266:1723–6. [19] Magee BB, Legrand M, Alarco AM, Raymond M, Magee PT. Many of the genes required for mating in Saccharomyces cerevisiae are also required for mating in Candida albicans. Mol Microbiol 2002;46:1345–51. [20] Lo HJ, Kohler JR, DiDomenico B, Loebenberg D, Cacciapuoti A, Fink GR. Nonfilamentous C. albicans mutants are avirulent. Cell 1997;90:939–49. [21] Chen CG, Yang YL, Cheng HH, Su CL, Huang SF, Chen CT, et al. Non-lethal Candida albicans cph1/cph1 efg1/efg1 transcription factor mutant establishing restricted zone of infection in a mouse model of systemic infection. Int J Immunopathol Pharmacol 2006;19:561–5. [22] Lo HJ, Wang JS, Lin CY, Chen CG, Hsiao TY, Hsu CT, et al. Efg1 involved in drug resistance by regulating the expression of ERG3 in Candida albicans. Antimicrob Agents Chemother 2005;49:1213–5. [23] Sellam A, Askew C, Epp E, Tebbji F, Mullick A, Whiteway M, et al. Role of transcription factor CaNdt80p in cell separation, hyphal growth, and virulence in Candida albicans. Eukaryot Cell 2010;9:634–44. [24] Riggle PJ, Kumamoto CA. Transcriptional regulation of MDR1, encoding a drug efflux determinant, in fluconazole-resistant Candida albicans strains through an Mcm1p binding site. Eukaryot Cell 2006;5:1957– 68. [25] Gillum AM, Tsay EY, Kirsch DR. Isolation of the Candida albicans gene for orotidine-5'-phosphate decarboxylase by complementation of S. cerevisiae ura3 and E. coli pyrF mutations. Mol Gen Genet 1984;198:179– 82. [26] Sherman F. Getting started with yeast. Methods Enzymol 2002;350:3–41. [27] Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts; approved standard. Document M27-A. Wayne, PA: CLSI; 1997. [28] Kofron M, Demel T, Xanthos J, Lohr J, Sun B, Sive H, et al. Mesoderm induction in Xenopus is a zygotic event regulated by maternal VegT via TGF growth factors. Development 1999;126:5759–70. [29] Franz R, Kelly SL, Lamb DC, Kelly DE, Ruhnke M, Morschhäuser J. Multiple molecular mechanisms contribute to a stepwise development of fluconazole resistance in clinical Candida albicans strains. Antimicrob Agents Chemother 1998;42:3065–72. [30] Braun BR, Johnson AD. TUP1, CPH1 and EFG1 make independent contributions to filamentation in Candida albicans. Genetics 2000;155:57– 67. Fig. 1. Susceptibility to fluconazole of Saccharomyces cerevisiae strain 10560-2B containing (A) pRS426 vector alone or (B) HLB126 overexpressing CPH1 as determined by Etest. The results were photographed after 2 days of growth on synthetic dextrose agar medium at 30 C. Fig. 2. Levels of MDR1 mRNA of different Candida albicans strains. The upper panels represent MDR1 mRNA and the lower panels represent ACT1 mRNA used as the loading control. Cells were grown in the absence (lanes 1, 3 and 5) or presence (lanes 2, 4 and 6) of 4-nitroquinoline N-oxide (4-NQO). Lanes 1 and 2, CPH1/CPH1 wild-type cells (SC5314); lanes 3 and 4, chp1/cph1 mutant cells (JKC19); and lanes 5 and 6, cph1/cph1::CPH1 cells (YLO323). Fig. 3. Susceptibilities to antifungal drugs of three Candida albicans strains [CPH1/CPH1 wild-type cells (SC5314), chp1/cph1 mutant cells (JKC19) and cph1/cph1::CPH1 cells (YLO323)] as determined by the agar dilution assay. (Left panel) Yeast–peptone–dextrose (YPD) medium containing an equal amount of dimethyl sulfoxide (DMSO) in the absence of drug was used as the growth control. Fluconazole (middle panel) and voriconazole (right panel) were prepared to final concentrations of 25 mg/L and 2 mg/L, respectively, in DMSO. The results were photographed after 2 days of growth at 30 C. Fig. 4. Susceptibilities of three Candida albicans strains [CPH1/CPH1 wild-type cells (SC5314), chp1/cph1 mutant cells (JKC19) and cph1/cph1::CPH1 cells (YLO323)] to (A) amphotericin B, (B) fluconazole and (C) voriconazole as determined by the broth microdilution assay. Growth of cells in the absence of drug was defined as 100.