LRI_VSmeeting09202011
advertisement

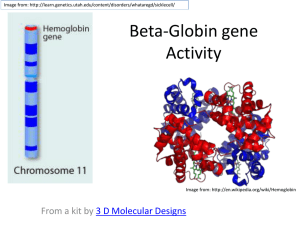
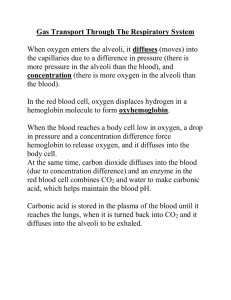
LRI Validation Suite Meeting September 20, 2011 Agenda • Action Item List • Test data update – Selection of core message set – NIST data sets and management of test data • Review policy proposal for validating receiver processing of terminology • Review ELINCS Test Plan and Test Tool • Update on LIS Test Plan Template • Update on EHR Test Plan Template • Juror Document/Spreadsheet Analysis – Mapping CLIA requirements to HL7 Elements – Identifying Reportable Conditions to PH Lab Results • Tooling Update • Face-to-Face Meeting Plans • Planning Selection of Core Test Messages 1. Common Hematology – – 1. CBC and WBC Differential/Morphology What lab results should be included in the CBC test message? Red Blood Cell (RBC) Erythrocyte count (varies with altitude): • • 2. 3. White Blood Cell (WBC) Leukocyte count: 4,500 to 10,000 cells/mcL Hematocrit (varies with altitude): • • 4. 2. Male: 40.7 to 50.3% Female: 36.1 to 44.3% Hemoglobin (varies with altitude): • • 5. 6. 7. 8. – – Male: 4.7 to 6.1 million cells/mcL Female: 4.2 to 5.4 million cells/mcL Male: 13.8 to 17.2 gm/dL Female: 12.1 to 15.1 gm/dL MCV: 80 to 95 femtoliter (Average red blood cell size) MCH: 27 to 31 pg/cell (amount hemoglobin per red blood cell) MCHC: 32 to 36 gm/dL (hemoglobin concentration per red blood cell) Platelet Count 150,000 to 400,000 per microliter (mcL) Note all seem to be A1 format What should be included in the WBC Differential/Morphology test message? Urinalysis – Pick A2 format? Selection of Core Test Messages 3. Comprehensive Metabolic Panel (CMP) – – Calcium; BUN; Creatinine; BUN/Creatinine Ratio (a calculated value); Total Protein; Albumin; Globulin; Albumin/Globulin Ratio (a calculated value); Bilirubin, Total; Glucose; Alkaline Phosphatase; AST; ALT; Sodium; Potassium; Chloride; CO2. Should all of these lab results be included in the test message? 4. Special Chemistry Tests – Lipid Panel???, Prostate Test??? 5. Microbiology tests, plus antibiotic susceptibility tests – A2 data 6. Other Clinical Lab Tests LOINC-RELMA List for Hemoglobin LOINC # 11559-2 19949-7 19951-3 19953-9 19955-4 2714-4 2715-1 2716-9 2717-7 30369-3 30370-1 34969-6 Component Ex. UCUM Units Ex. Units Order/Obs Oxyhemoglobin/Hemoglobin.total % Observation 1 Oxyhemoglobin/Hemoglobin.total % Class MFr % MFr % 2 Oxyhemoglobin/Hemoglobin.total MFr % % 2 Oxyhemoglobin/Hemoglobin.total MFr % PULM 2 Oxyhemoglobin/Hemoglobin.total MFr % PULM 2 Oxyhemoglobin/Hemoglobin.total MFr % % Observation 1 Oxyhemoglobin/Hemoglobin.total MFr % % Observation 1 Oxyhemoglobin/Hemoglobin.total MFr % % Observation 1 Oxyhemoglobin/Hemoglobin.total MFr % % Observation 1 Oxyhemoglobin/Hemoglobin.total MFr % % of tot Observation 1 Oxyhemoglobin/Hemoglobin.total MFr % % of tot Observation 1 Oxyhemoglobin/Hemoglobin.total MFr % % of tot Observation 1 No Method listed in RELMA for any of these tests Property Time Aspect System Scale Long Common Name Type Pt Bld Qn CHEM Fractional oxyhemoglobin in Blood 8H^max PULM BldA Qn Fractional oxyhemoglobin in 8 hour maximum Arterial blood 8H^min PULM BldA Qn Fractional oxyhemoglobin in 8 hour minimum Arterial blood Pt Bld.preductal Qn Fractional oxyhemoglobin in Blood Preductal % Pt Bld.postductal Qn Fractional oxyhemoglobin in Blood Postductal % Pt CHEM BldA Qn Fractional oxyhemoglobin in Arterial blood Pt CHEM BldC Qn Fractional oxyhemoglobin in Capillary blood Pt CHEM BldV Qn Fractional oxyhemoglobin in Venous blood Pt CHEM Plas Qn Fractional oxyhemoglobin in Plasma Pt CHEM BldCoV Qn Fractional oxyhemoglobin in Venous cord blood Pt CHEM BldCoA Qn Fractional oxyhemoglobin in Arterial cord blood Pt CHEM BldMV Qn Fractional oxyhemoglobin in Mixed venous blood Testing Options/Policy LOINC # Component Ex. Units Class Type 11559-2Oxyhemoglobin/Hemoglobin.total MFr % 1 19949-7Oxyhemoglobin/Hemoglobin.total MFr % 2 19951-3Oxyhemoglobin/Hemoglobin.total MFr % 2 Property Time Aspect System Long Common Name Scale Ex. UCUM Units Order/Obs Pt CHEM Bld Fractional oxyhemoglobin in Blood Qn % Observation 8H^max PULM BldA Qn Fractional oxyhemoglobin in 8 hour maximum Arterial blood % 8H^min PULM BldA Qn Fractional oxyhemoglobin in 8 hour minimum Arterial blood % OBR|1|111325^EHR^2.16.840.1.113883.19.3.2.3^ISO|1132896^Lab^2.16.840.1.113883.19.3.1.6^ISO|7187^Hemoglobin^LN|||20070701152505|||||||||100^Hippocrates^Harold||||||20070701162505||CH| F|NA&Not Applicable&LB OBX|1|NM|11559-2^Hemoglobin.Total^LN||^12.4|g/dL^grams per deciliter^UCUM|12.0 to 16.0||||F|||20070701152505|||||||||Effective Labs, Inc^^^^^DRSD&2.16.840.1.113883.19.1.11&ISO^XX^^^6543|3434 Test Loop^^Ann Arbor^MI^48103^^B • Depending on what the order is, what are possible test results? Are there more than one valid test result base on local conventions, etc.? • Potential Test Case Policy: In the data sheet (test case) we can allow any of these to be selected. This assumes that nothing else in the message needs to be changed. It would be an easy way to provide the capability to tests all of these LOINC codes with minimal effort. The Long Common Name is the differentiator. • One of the determining factors likely will be whether or not the same result value can be used for all of the various versions of Oxyhemoglobin/Hemoglobin.total. Issues/Comments: • Other data elements in the HL7 message might also need to be test-specific. For example, if data for the SPM-4: Specimen Type and SPM-8: Specimen Source are included in the message, then the same message probably could not be used for all of the versions of Oxyhemoglobin/Hemoglobin.total. OBX-7: Reference Range also might be a limiting factor if venous blood and arterial blood result values have normal ranges that don’t overlap. • The LOINC code is the anchor that discretely and accurately identifies the lab test that was ordered/performed. No matter what a hospital or physician chooses to call the test, the LOINC code is the one constant that tells everyone which it test was. For our purposes, we’ll need to be sure that all of the data for the data elements in the HL7 message are appropriate for the test indicated by the LOINC code. Note on the use of LOINC • The list of tests has been organized by order panel or, for micro related tests, by target organism for easier readability. • The LOINC terms included here are considered examples only – though they may be the more common LOINC terms, each laboratory needs to be sure to map their own tests to the most appropriate LOINC, even if it is NOT on this list. • This is NOT an exclusive list of LOINC terms – ANY valid LOINC should be accepted in data exchange projects based on this specification. Reporting Format Requirement 1. Tests and/or components with numeric results, units, and normal ranges 2. Tests and/or components with a limited set of textual results with or without normal ranges 1. 2. 3. 4. positive/negative/indeterminate, resistant/intermediate/susceptibility cytology / anatomic pathology mutation type and location organism name 3. Tests with defined structure in Observation Result Segment OBX-3 through OBX-8 for the reporting of Culture Results and Antimicrobial Sensitivities 4. Semi Structured or Unstructured components or results Tests and/or components reported in a PDF or data blob 1. The 4th reporting format may be utilized in the cases where structured data does not apply (e.g. images). Processing of Terminology • Receiver requirements for processing terminology: – The receiver shall persist (store) the original standardized code and the original standardized code text as received in exact representation. – The receiver may perform a translation/mapping to locally defined representations. Assessment of Terminology • Proposed procedure for assessing the receiver for incorporation of terminology: – Where applicable to meet CLIA requirements the receiver shall display on the EHR GUI the equivalent representation of the received coded lab results. The receiver shall display at least one of the following: • Original standardized code text • Original standardized code (will the actual code ever be displayed; is it adequate or good practice to display just the code?) • Local code text – The receiver shall be capable of demonstrating the persistent of the original standardized code and the original standardized code text. Acceptable methods for attestation: • Administrative access to database • Inspector approved method – If applicable the receiver shall be capable of demonstrating the linkage of the original standardized code the locally translated/mapped code. Acceptable methods for attestation: • Administrative access to database • Browse capabilities of configuration files • Inspector approved method Equivalent Representation • The exact original code • The exact original code text • For translated/mapped local code text an equivalent representation as determined by clinical terminology expert. The following rules and guidance are given to promote consistency in assessment: – Rule: A terminology shall never be made more specific in the translation/mapping. – Rule: A terminology shall never be made more specific in the display of standardized terminology. – Guidance: A limited number of synonyms are provided to assist the clinical terminology expert. Note: a predefined definitive set is not possible—there are too many possible equivalent local representations. – Guidance: The inspector must consider the context in which the code is used as this may impact the translation/mapping. Questions • What should be the assessment if a more detailed terminology term is received that is mapped to a less specific term? • This mapping will lead to a loss of information if the original code is not persisted. • Is it valid to display a representation that has less specificity? • Is it valid to display a representation that has less specificity as long as the original data is persisted in the system? • Is it acceptable for a loss of information to occur when data is rendered as a report or forwarded on to another system (e.g., public health)? That is we sent a specific code and then a general code is forwarded on to public health. Is it acceptable for either the general or specific LOINC code to be forwarded? Other Issues • EHR – Implementation Choices for Terminology – Use standardize coding internally – Map to local codes – Need to account for options in test procedure • How to we test for complete coverage of recommended terminology? – Create all messages for all possible terms (for important code system, e.g., LOINC)—This is the preferred approach – Alternative approach: Create a subset and inspect/verify tables for coverage and accuracy – Selection of approach may be made on a case-by-case analysis – It may be necessary to provide coverage for all recommended LOINC codes. However, for other terminology it may not be priority (e.g., state) or may not be feasible (SNOWMED). • Use of UCUM. Can/should UCUM be mapped locally and displayed as local representation? • What terminology can be mapped? Action Item List I • Select message to handle core lab results – Identify 20 or so common lab results – Obtain/Adapt/Create test messages to cover the core set of lab results • Identify/List all pertinent data elements – Create spreadsheet of all data elements with usage of R, RE, and C (rows) – Columns will identify: • Juror Document (How to assess the element) • Identify the elements required for CLIA testing • Identify static, configurable, or indifference data elements • Identify/create value sets – Incorporate the value sets in PHINVADS – Develop download mechanisms and transformation of values to support the NIST tooling format Action Item List II • Review LRI implementation Guide and create a list of all conformance requirements – Create matrix based on data elements – Link all conformance requirements to data elements when possible – Create “higher” level list of conformance requirements • Determine the policy for assessing receiver side terminology – Inspection test requirements and procedure – Automated test requirements and procedure • Complete development of LIS Test Plan Skeleton • Complete development of EHR Test Plan Skeleton Action Item List III • Identify and document the test dimensions – – – – – Coverage of Lab Results Scenarios (e.g., Preliminary, Final, Corrected) Reporting formats Negative testing Minimally and maximally populated • Contact CLIA and CAP inspectors to get their lab inspection process • Determine a process for verifying test cases • Implement process for verifying test cases • Research ELINCS Test Tool – Determine what we can leverage – Process flow, source code, test messages Action Item List IV • Identify all the public health reportable lab results • Identify the data elements that differ from the public health IG and the S & I LRI IG • Determine a policy for validating LRI messages using EHR PH lab results messages • Develop spreadsheets for managing test cases/data – Adapt tooling to process and incorporate data • Create the HL7 standard message profiles – MWB (then produce XML message template) – Need to make updates to the message profile based on changes made in version 2.7 and 2.7.1 – Write XSLT to modify XML message profile Tooling Update • LRI Implementation Guide is in ballot process – Open for comments until October 17th, 2011 • We will begin developing the HL7 standard conformance profile – MWB – Need to make updates to the conformance profile based on changes made in version 2.7 and 2.7.1 • Data Management of test cases/data will be with spreadsheet – Spreadsheet is process to build messages and to create validation context files – Validation context files encapsulates test case related assessment – Leverage/adapt existing NIST Test messages to S&I Framework LRI IG • Early version of prototype tool developed – Limited functionality – Handles message validation based on message profiles and validation context files – Message Editing Validation Methodology HL7 V2.5.1 Message Profile (LRI IG assertions) Test Case Specific Assertions (Validation Context Files) Vocabulary (Stored in PHINVADS than translated to V2.8 Table Library Format) Validation Engine and Juror Document Generator