Upper Gastrointestinal Problems
Zoya Minasyan
RN, MSN-Edu
The digestive system
Nausea and Vomiting
•
•
Most common manifestations of GI diseases
Nausea
–
–
–
•
Vomiting
–
–
–
•
Feeling of discomfort in the epigastric area with a conscious desire to vomit
Usually occurs before vomiting
Related to slowing of gastric motility and emptying
Forceful ejection of partially digested food and secretions (emesis) from the upper GI tract
Complex act requiring coordination of several structures
Receives input from various stimuli
Occurs from
–
–
–
–
–
–
–
–
GI disorders
Pregnancy
Infectious diseases
CNS disorders
Cardiovascular problems
Metabolic disorders
Side effects of drugs
Psychologic factors
Stimuli Involved in Vomiting
Stimuli involved in the act of vomiting. CTZ,
Chemoreceptor trigger zone; GI, gastrointestinal.
Clinical Manifestations
• Nausea
– Subjective complaint
– Usually accompanied by anorexia
• Vomiting
– Dehydration can rapidly occur when prolonged.
– Water and essential electrolytes are lost.
– Metabolic alkalosis—from loss of gastric HCl
– Metabolic acidosis—from loss of bicarbonate if
the contents from the small intestine are vomited
Collaborative Care
• Differentiate among vomiting, regurgitation, and
projectile vomiting
• Regurgitation
– Partially digested food slowly brought up into stomach
• Projectile vomiting
– Forceful expulsion of stomach contents without
nausea
• Fecal odor and bile indicate a lower intestinal
obstruction.
• Color of emesis aids in determining presence and
source, if bleeding.
Collaborative Care
• Drug therapy
– Antiemetics act on CNS to block chemicals that trigger nausea
and vomiting.
– Examples
• Anticholinergics
– Scopolamine transdermal (Transderm-Scop)
• Antihistamines
–
–
–
–
Dimenhydrinate (Dramamine)
Promethazine (Phenergan)
Meclizine (Antivert)
Hydroxyzine (Vistaril)
• Phenothiazines
– Prochlorperazine (Compazine)
• Chlorpromazine (Thorazine)
– Common side effects include
•
•
•
•
•
Dry mouth
Hypotension
Sedative effects
Rashes
GI disturbances
Esophageal Disorders
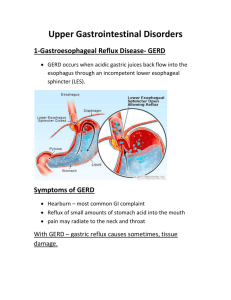
• Gastroesophageal reflux disease (GERD)
(discussed in another PowerPoint)
•
•
•
•
•
•
Hiatal hernia
Esophageal cancer
Esophageal diverticula
Esophageal strictures
Achalasia
Esophageal varices
Gastroesophageal reflux disease
(GERD)
Description
• Not a disease but a syndrome, secondary to
reflux of gastric contents into lower esophagus
Etiology and Pathophysiology
Esophagitis with esophageal ulcerations.
Etiology and Pathophysiology
•
Predisposing factors
– Hiatal hernia
– Incompetent lower esophageal sphincter (LES)
•
Antireflux barrier
– Decreased esophageal clearance
– Decreased gastric emptying
•
HCl acid and pepsin secretions reflux—cause irritation and inflammation
•
Intestinal proteolytic enzymes and bile salts add to irritation.
– Primary factor in GERD
•
•
•
•
•
•
•
Results in ↓ in pressure in distal portion of esophagus
Gastric contents move from stomach to esophagus.
Can be due to certain foods (caffeine, chocolate) and drugs (anticholinergics)
Obesity is a risk factor.
Pregnant women are at increased risk.
Cigarette and cigar smoking can contribute to GERD.
Hiatal hernia is a common cause of GERD.
Clinical Manifestations
• Symptoms of GERD
– Heartburn (pyrosis)
• Most common clinical manifestation
• Burning, tight sensation felt beneath the lower sternum and
spreading upward to throat or jaw
• Felt intermittently
• Relieved by milk, alkaline substances, or water
– Dyspepsia
• Pain or discomfort centered in upper abdomen
– Hypersalivation
– Noncardiac chest pain
• More common in older adults
Clinical Manifestations
• Most individuals have mild symptoms.
– Heartburn after a meal
– Occurs once a week
– No evidence of mucosal damage
• Individual may also report
–
–
–
–
–
–
–
–
Wheezing
Coughing
Dyspnea
Hoarseness
Sore throat
Lump in throat
Choking
Regurgitation
Clinical Manifestations
• Regurgitation
– Effortless return of food or gastric contents from stomach into
esophagus or mouth
– Described as hot, bitter, or sour liquid coming into the mouth or
throat
– Can mimic angina
• Related to direct local effects of gastric acid on esophageal
mucosa
– Esophagitis
•
•
•
•
Inflammation of esophagus
Frequent complication
Other risk factors include hiatal hernia, chemical irritation.
Repeated exposure—esophageal stricture
– Resulting in dysphagia
Esophagitis
Nissen fundoplication for repair of hiatal hernia. A, Fundus of stomach is wrapped around
distal esophagus. B, The fundus is then sutured to itself.
Complications
• Respiratory
– Due to irritation of upper airway by secretions
•
•
•
•
Cough
Bronchospasm
Laryngospasm
Potential for asthma, bronchitis, and pneumonia
– Dental erosion
• From acid reflux into mouth
• Especially posterior teeth
Diagnostic Studies
• History and PE
• Barium swallow
– Can detect protrusion of gastric fundus
• Upper GI endoscopy
– Useful in assessing LES competence, degree of
inflammation, scarring, strictures
Collaborative Care
• Lifestyle modifications
– Avoid triggers
• Nutritional therapy
–
–
–
–
–
Decrease high-fat foods.
Take fluids between rather than with meals.
Avoid milk products at night.
Avoid late-night snacking or meals.
Avoid chocolate, peppermint, caffeine, tomato
products, orange juice.
– Weight reduction therapy
Collaborative Care: Drug therapy
– Histamine (H2)-receptor blockers
•
•
•
•
Decrease secretion of HCl acid
Reduce symptoms and promote esophageal healing in 50% of patients
Side effects uncommon
Pepcid, Zantac, Tagamet
– Proton pump inhibitors (PPIs)
•
•
•
•
•
Decrease gastric HCl acid secretion
Promote esophageal healing in 80% to 90% of patients
May be beneficial in ↓ esophageal strictures
Headache: Most common side effect
Prilosec, Nexium, Aciphex
– Antacids
•
•
•
•
Quick but short-lived relief
Neutralize HCl acid
Taken 1 to 3 hours after meals/bedtime
Maalox, Mylanta
– Acid protective
•
•
Used for cytoprotective properties
Sucralfate (Carafate)
– Cholinergic
•
•
•
•
•
Increase LES pressure
Improve esophageal emptying
Increase gastric emptying
Negative: Stimulate HCl acid secretion
Bethanechol (Urecholine)
– Prokinetic drugs
•
•
Promote gastric emptying
Reduce risk of gastric acid reflux
–
Metoclopramide (Reglan)
Medications
•
•
•
•
Antacids – e.g. Mylanta Neutralize excess acids.
administer 1-3 hours after eating and at HS.
Should be separated with other meds at
least 1 hour.
Histamine 2 receptor antagonist – e.g. Zantac
(Ranitidine). Reduce the secretion of acid.
Proton Pump Inhibitors (PPIs) – e.g Protonix
(Pantoprazole).
Reglan (Metochlopramide HCL) to increase motility of the esophagus and
stomach
.
Nursing Management
• Avoidance of factors that cause reflux
– Stop smoking
– Avoid alcohol and caffeine
– Avoid acidic foods
•
•
•
•
•
•
•
•
Stress reduction techniques
Weight reduction, if appropriate
Small frequent meals
Elevation of HOB 30 degrees
Not lying down for 2 to 3 hours after eating
Avoidance of late-night eating
Evaluation of effectiveness of medications
Observing for side effects of medications
Hiatal Hernia
• Herniation of portion of the stomach into
esophagus through an opening or hiatus in
diaphragm
• Also referred to as diaphragmatic hernia and
esophageal hernia
– Sliding
• Stomach slides into thoracic cavity when supine, goes back
into abdominal cavity when standing upright.
• Most common type
– Paraesophageal or rolling
• Esophageal junction remains in place, but fundus and
greater curvature of stomach roll up through diaphragm.
Hiatal Hernia
• Many factors involved
•
•
•
•
•
•
•
•
•
•
Weakening of muscles in diaphragm
Increased intraabdominal pressure
Obesity
Pregnancy
Heavy lifting
Increasing age
Trauma
Poor nutrition
Forced recumbent position
Congenital weakness
Hiatal Hernia
Clinical Manifestations
Symptoms include
– Heartburn
• After meal or lying supine
– Dysphagia
Complications
• GERD
• Esophagitis
• Hemorrhage from erosion
• Stenosis
• Ulcerations of herniated portion
• Strangulation of hernia
• Ulcerations of herniated portion
• Regurgitation with tracheal aspiration
• Increased risk of respiratory problems
Hiatal Hernia
Diagnostic Studies
• Barium swallow
– May show protrusion of gastric fundus through
esophageal hiatus
• Endoscopy
– Visualize lower esophagus
– Information on degree of inflammation or other
problems
Hiatal Hernia
Conservative Therapy
• Lifestyle modifications
– Eliminate alcohol.
– Elevate HOB.
– Stop smoking.
– Avoid lifting/straining.
– Reduce weight, if appropriate.
– Use antisecretory agents and antacids.
Hiatal Hernia
Surgical Therapy
• Reduction of herniated stomach
• Herniotomy
– Excision of hernia sac
• Herniorrhaphy
– Closure of hiatal defect
Esophageal Cancer
Arise from glands lining esophagus
• Resemble cancers of stomach and small intestine
• Cause is unknown.
– Incidence ↑ with age.
– ↑ incidence in African Americans and Alaska Natives.
• Risk factors
–
–
–
–
–
–
Smoking
Excessive alcohol intake
Central obesity
Diet low in fruits and vegetables
Exposure to lye, asbestos, and metal
History of achalasia
Esophageal Cancer
Etiology and Pathophysiology
• Majority of tumors located in middle and
lower portions of esophagus
• Malignant tumor
– Usually appears as ulcerated lesion
– May penetrate muscular layer and outside wall of
esophagus
– Obstruction in later stages
Esophageal Cancer: Clinical Manifestations
• Symptom onset is late.
• Progressive dysphagia is most common.
– Initially with meat, then with soft foods and liquids
• Pain develops late.
– Substernal, epigastric, or back area
• Increases with swallowing
• May radiate
• Weight loss
• Regurgitation of blood-flecked esophageal contents
• If tumor is in upper third of esophagus
– Sore throat
– Choking
– Hoarseness
• Hemorrhage
– If erodes into aorta
• Esophageal perforation with fistula formation
• Esophageal obstruction
• Metastasis
– Liver and lung common
Esophageal Cancer
Diagnostic Studies
• Endoscopy with biopsy
– Necessary for definitive diagnosis
• Endoscopic ultrasonography (EUS)
– Important tool to stage
• Barium swallow with fluoroscopy
• Bronchoscopic examination
– Detect involvement of lung
• Computed tomography (CT)
• Magnetic resonance imaging (MRI)
Esophageal Diverticula
• Sac-like outpouchings of one or more layers of esophagus
• Esophageal achalasia. A, Early stage, showing tapering of lower
esophagus. B, Advanced stage, showing dilated esophagus.
Esophageal Diverticula
Clinical Manifestations
• Traction diverticulum: May not have signs and
symptoms
• Symptoms
– Dysphagia
– Regurgitation
– Chronic cough
– Aspiration
– Weight loss
Esophageal Diverticula
• Diagnostic Studies
– Endoscopy
– Barium studies
• Surgery
– Endoscopic or external cervical approach
Esophageal Strictures
Etiology and Pathophysiology
• Usually develop over a long time
• Result in
– Dysphagia
– Regurgitation
– Weight loss
• Causes include
– GERD
– Ingestion of strong acids or alkalis
– Trauma
• Throat lacerations, gunshot wounds
• Due to scar formation
Esophageal Strictures
Collaborative Care
• Treatment
– Dilated endoscopically
– Surgical excision
• Patient may have a temporary or a permanent
gastrostomy.
Esophageal Achalasia
Pneumatic dilation attempts to treat achalasia by maintaining
an adequate lumen and decreasing lower esophageal sphincter
(LES) tone.
Achalasia
Etiology and Pathophysiology
• Food and fluid accumulate in lower esophagus.
• Result: Dilation of lower esophagus
• Symptoms
– Dysphagia
• Most common symptom
– Globus sensation
– Substernal chest pain
• During/after a meal
–
–
–
–
–
Halitosis
Inability to belch
GERD
Regurgitation
Weight loss
Achalasia
Diagnostic Studies
•
•
•
•
Radiologic studies
Manometric studies of lower esophagus
Endoscop
Goals
– Relieve symptoms
– Improve esophageal emptying
– Prevent development of megaesophagus
Pneumatic Dilation to Treat Achalasia
Multiple stress ulcers of the stomach, highlighted by dark
digested blood on their surfaces.
Achalasia
Collaborative Care
• Drug therapy
– Smooth muscle relaxants
– Botulinum toxin injection
• 1 to 2 years relief
• Symptomatic relief
– Semisoft bland diet
– Eating slowly
– Drinking with meals
– Sleeping with HOB elevated
Esophageal Varices
•
•
•
Dilated veins in lower portion of esophagus
Result of portal hypertension
Common complication of liver cirrhosis
Upper GI (UGI) Bleeding
Etiology and Pathophysiology
• Most serious loss of blood from UGI
characterized by sudden onset
• Insidious occult bleeding can also be a major
problem.
• Increased incidence of UGI bleeding in older
adults, especially women, and use of NSAIDs
• Severity depends on bleeding origin.
– Venous
– Capillary
– Arterial
Etiology and Pathophysiology
• Types of UGI bleeding
– Obvious bleeding
• Hematemesis
– Bloody vomitus
» Appears fresh, bright red blood or “coffee grounds”
• Melena
– Black, tarry stools
» Caused by digestion of blood in GI tract
» Black appearance—due to iron
Etiology and Pathophysiology
• Bleeding from arterial source is profuse, and
the blood is bright red.
• The bright red color indicates that the blood
has not been in contact with the stomach’s
acid secretions.
• “Coffee ground” vomitus reveals that the
blood has been in the stomach for some time
and has been changed by gastric secretions.
Etiology and Pathophysiology
• The longer the passage of blood through
intestines, the darker the stool color caused by
breakdown of Hb—release of iron
• Cause of bleeding is not always easy to
determine.
– Variety of areas in GI tract may be involved.
Nursing Management
• Nursing assessment
– LOC
– VS
• Orthostatic
• Every 15 to 30 minutes
–
–
–
–
–
Appearance of neck veins
Skin color
Capillary refill
Abdominal distention, guarding, peristalsis
Signs/symptoms of shock
•
•
•
•
•
Low BP
Rapid, weak pulse
Increased thirst
Cold, clammy skin
Restlessness
Nursing Management
• Nursing diagnoses
– Deficient fluid volume
– Ineffective tissue perfusion
– Anxiety
– Ineffective coping
– Risk for aspiration
– Decreased cardiac output
Nursing Management
• Planning: Overall goals
– No further GI bleeding
– Cause of the bleeding identified and treated
– Return to normal hemodynamic state
– Minimal or no symptoms of pain or anxiety
Nursing Management
• Health promotion
– Patient with a history of chronic gastritis or peptic ulcer disease is at high risk.
– Patient who has had one major bleeding episode is more likely to have
another.
– Patient with cirrhosis or previous UGI bleed is also at high risk.
– Nurse education
• Disease process and drug therapy
• Avoidance of gastric irritants
– Alcohol
– Smoking
– Prevent or decrease stress-inducing situations.
• Take only prescribed medications.
• Methods of testing vomitus/stools for occult blood
– Patient teaching
• Potential adverse effects related to GI bleeding
• Prompt treatment of upper respiratory infection in patient with esophageal varices
• If aspirin must be prescribed, enteric-coated tablets can be substituted for regular
tablets.
• Taking the medications with meals or snacks lessens the potential irritating effects.
Nursing Management
•
Acute intervention
–
–
–
–
–
Approach in calm, assured manner to decrease anxiety.
Use caution when administering sedatives for restlessness.
Warning sign of shock may be masked by drugs.
IV maintenance
Accurate I/O record
•
•
•
–
Urine output hourly
At least 0.5 mL/kg/hr indicates adequate renal perfusion.
Urine-specific gravity should be measured. Normal (1.005 to 1.025)
Nutrition
•
•
•
•
Observed for symptoms of nausea and vomiting
Recurrence of bleeding
Feedings initially include clear fluids or milk given hourly.
Gradual introduction of food follows as tolerated
– Monitor laboratory studies.
•
•
Hb and Hct every 4 to 6 hours
BUN assessed
– Oxygen management
Nursing Management
• Ambulatory and home care
– Patient teaching
• Patient/family taught how to avoid future bleeding
episodes
• Made aware of consequences of noncompliance with
diet and drug therapy
• Emphasis that no drugs other than those prescribed
should be taken
• No smoking, alcohol
• Need for long-term follow-up care
• Instruction if an acute hemorrhage occurs in future
Nursing Management
• Evaluation
– Have no further GI bleeding
– Maintain normal fluid volume
– Experience return to normal hemodynamic state
– Experience absence of or tolerable levels of pain
and be comfortable
– Understand potential etiologic factors, and make
appropriate lifestyle modifications
Audience Response Question
When teaching a patient with a history of upper GI bleeding to
check the stools for blood, the nurse informs the patient that:
1. If vomiting of bright red blood occurs, stools will not be black and
sticky.
2. Blood is never obvious in stools and must be detected by fecal
occult blood testing.
3. Acute bleeding in the upper GI tract will result in bright red blood in
the stools.
4. Stools that are black and tarry occur with prolonged bleeding from
the stomach or small intestine.
Peptic Ulcer Disease
• Erosion of GI mucosa resulting from digestive
action of HCl acid and pepsin
• Ulcer development can occur in
– Lower esophagus
– Stomach
– Duodenum
Peptic Ulcers
Peptic ulcers, including an erosion, an acute ulcer, and a chronic ulcer. Both the acute ulcer and
the chronic ulcer may penetrate the entire wall of the stomach.
Peptic Ulcer of the Duodenum
Etiology and Pathophysiology
• Develops only in the presence of an acid environment
• Excess of gastric acid not necessary for ulcer development
• Pepsinogen is activated to pepsin in presence of HCl acid and at pH of
2 to 3.
• Stomach normally protected from auto digestion by gastric mucosal
barrier
• Surface mucosa of stomach is renewed about every 3 days. Mucosa can
continually repair itself, except in extreme instances.
• Water, electrolytes, and water-soluble substances can pass through
barrier.
• Mucosal barrier prevents back diffusion of acid and pepsin from gastric
lumen through mucosal layers to underlying tissue.
• Mucosal barrier can be impaired, and back diffusion can occur.
– Cellular destruction and inflammation occur.
– Release of histamine
• Vasodilation
• Increased capillary permeability
• Secretion of acid and pepsin
Etiology and Pathophysiology
• Destroyers of mucosal barrier
– Helicobacter pylori
• Produces enzyme urease
– Mediates inflammation, making mucosa more vulnerable
– Aspirin and NSAIDs
• Inhibit syntheses of prostaglandins
– Cause abnormal permeability
– Corticosteroids
• ↓ rate of mucosal cell renewal
– ↓ protective effects
– Lifestyle factors
• Alcohol, coffee, smoking, psychologic stress
Clinical Manifestations
• Pain high in epigastrium
• 1 to 2 hours after meals
• “Burning” or “gaseous”
• Food aggravates pain as ulcer has eroded through gastric
mucosa.
• Duodenal ulcer pain
•
•
•
•
•
Midepigastric region beneath xiphoid process
Back pain—if located in posterior aspect
2 to 5 hours after meals
“Burning” or “cramplike”
Tendency to occur, then disappear, then occur again
Complications
• Three major complications include
– Hemorrhage
– Perforation
– Gastric outlet obstruction
• All considered emergency situations
Complication of peptic ulcer disease
Perforation develops from erosion of
– Granulation tissue found at base of ulcer during healing
– Ulcer through a major blood vessel
– Sudden, dramatic onset
– Severe upper abdominal pain spreads throughout
abdomen.
– Tachycardia, weak pulse
– Rigid, board-like abdominal muscles
– Shallow, rapid respirations
– Bowel sounds absent
– Nausea/vomiting
– Bacterial peritonitis may occur within 6 to 12 hours.
– Difficult to determine from symptoms alone if gastric or
duodenal ulcer has perforated
Gastric Outlet Obstruction
• Predisposition to gastric outlet obstruction
includes
– Ulcers located in
• Antrum and prepyloric and pyloric areas of stomach
• Duodenum
–
–
–
–
–
Edema
Inflammation
Pylorospasm
Fibrous scar tissue formation
All contribute to narrowing of pylorus.
Gastric Outlet Obstruction
• Early phase: Gastric emptying normal
• Over time, ↑ contractile force needed to empty
stomach
– Hypertrophy of stomach wall
• After long-standing obstruction
– Stomach dilates and becomes atonic.
• Clinical manifestations
– Usually long history of ulcer pain
– Pain progresses to generalized upper abdominal
discomfort.
Gastric Outlet Obstruction
• Clinical manifestations (cont’d)
– Pain worsens toward end of day as stomach fills and
dilates.
– Relief obtained by belching or vomiting
– Vomiting is common.
– Constipation is a common complaint.
• Dehydration, lack of roughage in diet
–
–
–
–
Swelling in stomach and upper abdomen
Loud peristalsis
Visible peristaltic waves
If stomach grossly dilated, may be palpable
Collaborative Care
•
Medical regimen consists of
–
–
–
–
–
–
–
–
–
•
Adequate rest
Dietary modification
Drug therapy
Elimination of smoking and alcohol
Long-term follow-up care
Stress management
Aim of treatment program
Reduce degree of gastric acidity
Enhance mucosal defense mechanisms
Generally treated in ambulatory care clinics
– Ulcer healing requires many weeks of therapy.
– Pain disappears after 3 to 6 days.
•
Complete healing may take 3 to 9 weeks.
– Should be assessed by means of x-rays or endoscopic examination
•
•
Aspirin and nonselective NSAIDs may be stopped.
Smoking cessation
Drug Therapy
H2R blockers. Ex: Cimetidine, Ranitidine ,Famotidine
PPIs proton pump inhib. Ex: Esomeprazole,Omeprazole
Antibiotics. Ex: Ranitidine bismuth citrate (Tritec) with
clarithromycin (Biaxin)
Antacids . Ex:Effects on empty stomach 20 to 30
minutes; If taken after meals, may last 3 to 4 hours
Therapy Related to Complications
• Perforation
– Immediate focus:
• Stop spillage of gastric or duodenal contents into peritoneal cavity.
• Restore blood volume.
– NG tube is placed into stomach.
• Continuous aspiration
• Placement of tube near to perforation site facilitates decompression.
– Circulating blood volume: Replaced with lactated Ringer’s and albumin
solutions
• Blood replacement in form of packed RBCs may be necessary. Central venous
pressure line inserted and monitored hourly
• Indwelling urinary catheter inserted and monitored hourly
• ECG—if history of cardiac disease
– Broad-spectrum antibiotics
– Pain medication
– Open or laparoscopic repair
Therapy Related to Complications
• Gastric outlet obstruction
–
–
–
–
–
Decompress stomach.
Correct any existing fluid and electrolyte imbalances.
Improve patient’s general state of health.
NG tube inserted in stomach, attached to continuous suction
Continuous decompression allows
• Stomach to regain its normal muscle tone
• Ulcer to begin to heal
• Inflammation and edema to subside
– After several days, NG clamped and residual volumes checked
• Common to clamp tube overnight for
8 to 12 hours and measure residual in morning
– When aspirate below 200 mL
• Within normal range
• Oral intake of clear liquids can begin
– Watch patient carefully for signs of distress or vomiting.
– As residual ↓, solid foods added and tube removed
Nursing Implementation
• Hemorrhage
– Changes in vital signs, ↑ in amount and redness
of aspirate
• Signal massive upper GI bleeding
– ↑ amount of blood in gastric contents
– ↓ pain because blood neutralizes acidic
gastric contents
– Maintain patency of NG tube.
• Prevent blood clot blockage.
• If blocked, distention results.
Nursing Implementation
• Perforation
– Sudden, severe abdominal pain unrelated in intensity and location to
pain that brought patient to hospital
• Possibility of perforation
–
–
–
–
–
–
Indicated by a rigid, board-like abdomen
Severe generalized abdominal and shoulder pain
Shallow, grunting respirations
Bowel sounds diminished or absent
Vital signs every 15 to 30 minutes
Stop all oral, NG feeds/drugs until health care provider notified. IV
fluids may be increased to replace volume lost.
– Ensure any known allergies are reported on chart.
• Antibiotic therapy is usually started.
Surgical or laparoscopic closure may be necessary if perforation does not heal
spontaneously.
Nursing Implementation
• Gastric outlet obstruction
– Can occur at any time
• Likely in patients whose ulcer is located close to pylorus
– Gradual onset
– Constant NG aspiration of stomach contents may relieve
symptoms.
– If occurs during treatment of acute exacerbation
• Regular irrigation of NG tube
• Repositioning from side to side
– IV fluids for hydration
– Accurate I/O
– Surgery may be performed if conservative treatment not
successful
Ambulatory and Home Care
• Patient teaching
– Disease
• Teach basic etiology/pathophysiology.
– Drugs
– Actions, side effects, danger of taking any medication
without health care provider approval
– Lifestyle changes
• Appropriate changes in diet
– Regular follow-up care
• Discuss medications.
• Encourage compliance with plan of care.
• Importance of immediate reporting of N/V, epigastric pain, bloody
emesis, or tarry stools
Surgical Therapy
• Uncommon because of anti secretory agents
• Indications for surgical interventions
– Unresponsive to medical management
– Concern about gastric cancer
Billroth I: Gastroduodenostomy
Partial gastrectomy with removal of distal 2/3 stomach and
anastomosis of gastric stump to duodenum
Billroth II: Gastrojejunostomy
Partial gastrectomy with removal of distal 2/3 stomach and
anastomosis of gastric stump to jejunum
Surgical Therapy
A, Billroth I procedure (subtotal gastric resection with gastroduodenostomy anastomosis). B, Billroth II procedure
Copyright
© 2007,
2004, 2000, Mosby, Inc.,
an affiliate of Elsevier Inc. All Rights Reserved.
(subtotal gastric resection
with
gastrojejunostomy
anastomosis).
Surgical Therapy
• Surgical therapies (cont’d)
– Vagotomy
• Severing of vagus nerve
• Can be total or selective
– Pyloroplasty
•
•
•
•
Surgical enlargement of pyloric sphincter
Commonly done after vagotomy
↓ gastric motility and gastric emptying
If accompanying vagotomy, ↑ gastric emptying
Postoperative Complications
• Most common
– Dumping syndrome
– Postprandial hypoglycemia
– Bile reflux gastritis
Postoperative Complications
• Dumping syndrome
– 20% of patients experience after surgery.
– Direct result of surgical removal of a large portion of
stomach and pyloric sphincter
– ↓ ability of stomach to control amount of gastric
chyme entering small intestine
• Large bolus of hypertonic fluid enters intestine
• ↑ fluid drawn into bowel lumen
– Occurs at end of meal or 15 to 30 minutes after eating
– Symptoms include
• Weakness, sweating, palpitations, dizziness, abdominal
cramps, borborygmi, urge to defecate
• Last no longer than an hour
Postoperative Complications
• Postprandial hypoglycemia
– Result of uncontrolled gastric emptying of a bolus
of fluid high in carbohydrate into small intestine
• ↑ blood sugar
• Release of excessive amounts of insulin into circulation
– Secondary hypoglycemia occurs with symptoms
~2 hours after meals.
– Symptoms include sweating, weakness, mental
confusion, palpitations, tachycardia, and anxiety.
Postoperative Complications
• Bile reflux gastritis
– Surgery can result in reflux alkaline gastritis.
• Prolonged contact of bile causes damage to gastric
mucosa.
• May result in back diffusion of H+ ions through gastric
mucosa
• Peptic ulcer disease may reoccur.
– Continuous epigastric distress that ↑ after meals
– Administration of cholestyramine (Questran)
relieves irritation.
Nutritional Therapy Postoperatively
• Start as soon as immediate postoperative period has
successfully passed.
• Patient should be advised to reduce drinking fluid (4
oz) with meals.
• Diet should consist of
–
–
–
–
–
Small, dry feedings daily
Low carbohydrates
Restricted sugar with meals
Moderate amounts of protein and fat
30 minutes of rest after each meal. The dietitian usually
gives dietary instructions, and the nurse needs to reinforce
them.
• Location:
ulcer on stomach=Gastric Ulcer
ulcer on upper intestine=Duodenal Ulcer
ulcer on esophagus=Esophageal Ulcer
Gastric Ulcer
Duodenal Ulcer
30 to 60 min after meal
1.5 to 3 hr after meal
Rarely occurs at night
Often occurs at night
Pain worsens with food ingestion
Pain relieved by food
ingestion
•Peptic ulcer disease can be differentiated between gastric, duodenal, and
stress ulcers.
•Silent ulcers may occur with pts with diabetes, NSAID users such as
aspirin and ibuprofen.
•If left untreated, complications may occur such as bleeding, perforation,
penetration or the obstruction of the digestion tract.
Gastroenteritis
• Definition - Gastroenteritis is a condition that causes
irritation and inflammation of the stomach and intestines (the
gastrointestinal tract). Diarrhea, crampy abdominal pain,
nausea, and vomiting are the most common symptoms.
• Causes:
- Viral infection
- Bacterial infection (Salmonella)
- Parasites
- Food-borne illness (such as shellfish) can be the
offending agent.
Causes of Gastroenteritis
• Viruses and bacteria are very contagious and can spread
through contaminated food or water. Gastroenteritis
caused by viruses may last one to two days. Bacterial cases
can last for a longer period of time.
Virus e.g. Norovirus, Rotavirus
Bacteria e.g Staphylococci, E. Coli, Shigella, Salmonella,
Campylobacter. Clostridium Difficile.
Parasite – Giardia (Giardiasis)
• Improper handwashing following a bowel movement or
handling a diaper can spread the disease from person to
person.
• Gastroenteritis that is not contagious to others can be
caused by chemical toxins, most often found in seafood,
food allergies, heavy metals, antibiotics, and other
medications.
Sign and Symptoms
Common symptoms may include:
• Low grade fever to 100°F (37.7°C)
• Nausea with or without vomiting
• Mild-to-moderate diarrhea
• Crampy, painful abdominal bloating
More serious symptoms:
• Blood in vomit or stool
• Vomiting more than 48 hours
• Fever higher than 101°F (40°C)
• Swollen abdomen or abdominal pain
• Dehydration - weakness, lightheadedness, decreased urination, dry
skin, dry mouth and lack of sweat and tears are characteristic
findings.
• Signs and symptoms of both include pain, cramping, belching,
nausea, and vomiting. Severe cases may include hematemesis.
Diarrhea may occur with gastroenteritis.
Exams and Diagnostic Tests
• Blood and stool tests to determine the cause of the vomiting and
diarrhea.
• Physical examination.
• Complete Blood Count
• Ask if other family or friends have similar exposure or symptoms.
Ask about the duration, frequency, and description of the patient's
bowel movements and whether they are vomiting.
• Travel history: Travel may suggest E. coli bacterial infection or a
parasite infection from something that client ate or drank.
• Exposure to poisons or other irritants: Swimming in contaminated
water or drinking from suspicious fresh water such as mountain
streams or wells may indicate infection from Giardia - an organism
found in water that causes diarrhea.
• Diet change, food preparation habits, and storage.
Tests for Gastroenteritis
• In general, symptoms caused by bacteria or their
toxins will become apparent after the following
amount of time:
Staphylococcus aureus in 2-6 hours
Clostridium 8-10 hours
Salmonella in 12-72 hours
• Medications: If the patient has used broadspectrum or multiple antibiotics recently, they
may have antibiotic-associated irritation of the
gastrointestinal tract.
Other conditions associated with Gastroenteritis
• Physical examination will provide reasons for
symptoms that may not be related to infection.
• If there are specific tender areas in the abdomenappendicitis, gallbladder disease, pancreatitis,
diverticulitis, or other conditions that may be the
cause of the patient's symptoms.
• Other noninfectious gastrointestinal diseases like
Crohn's disease or ulcerative colitis must also be
considered.
Treatments for Gastroenteritis
• Antibiotics are not usually prescribed until bacteria have been
identified.
• Antibiotics may be given for certain bacteria, specifically
Campylobacter, Shigella, and Vibrio cholerae, if properly identified
through laboratory testing. Otherwise, using any antibiotic or the
wrong antibiotic can worsen some infections or make them last
longer.
• Infections, like salmonella, are not treated with antibiotics.
Supportive care of fluids and rest, the body is able to resolve the
infection without antibiotics.
• For adults, medications to stop vomiting (antiemetics) such as
promethazine (Phenergan, Anergan), prochlorperazine
(Compazine), or Ondansetron (Zofran). These medications are
prescribed as a suppository.
• IV fluids
• Most common antidiarrheal agents for people older than three
years are over-the-counter medications such as diphenoxylate
atropine (Lomotil, Lofene, Lonox) or loperamide hydrochloride
(Imodium).
Nursing Care
• Gastritis may be caused by a chemical, thermal, or
bacterial insult ( alcohol, aspirin, and
chemotherapeutic agents;hot, spicy, rough, or
contaminated foods).
• Management involves symptomatic treatment
measures after removal of the causative agent.
• Stop all P.O. intakes until symptoms subside.
• Assess the client's symptoms and administer the
prescribed symptomatic relief medications such as
antacids and antiemetics.
• Monitor intake and output.
• Administer IV to replace lost fluids.
• Weigh daily.
• Encourage the prescribed diet.